Acute Ischaemic Stroke as a Manifestation of Pituitary Apoplexy in a Young Lady
Shaik Afsar Pasha1, Laxmi Narasimhan Ranganthan2, Vamsi Krishna Setty3, Ramakrishna Reddy4, Deepika Ananda Ponnuru5
1 Associate Professor, Department of Neurology, NRI Medical College and General Hospital, Chinakakani, Guntur, Andhra Pradesh, India.
2 Professor, Department of Neurology, Institute of Neurology, Madras Medical College, Chennai, India.
3 Assistant Professor, Department of Radiology, NRI Medical College and General Hospital, Chinakakani, Guntur, Andhra Pradesh, India.
4 Professor, Department of Neurosurgery, NRI Medical College and General Hospital, Chinakakani, Guntur, Andhra Pradesh, India.
5 Postgraduate, Department of Medicine, NRI Medical College and General Hospital, Chinakakani, Guntur, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shaik Afsar Pasha, Department of Neurology, NRI Medical College and General Hospital, Chinakakani, Guntur-522503, Andhra Pradesh, India.
E-mail: afsarpasha81@gmail.com
Pituitary Apoplexy (PA) is defined as a clinical syndrome comprising headache, visual deficits and altered sensorium, which can result from haemorrhage or infarction of the pituitary gland. Acute ischaemic stroke following PA is very rare. We are presenting a 35-year-old young otherwise healthy lady who presented with neuro ophthalmological and vascular symptoms on a background of PA. Imaging revealed a pituitary macro adenoma with parasellar extension with internal bleed. Cerebral angiography revealed that the mass compressed the bilateral cavernous sinuses (left more than right), resulting in obliteration of the cavernous portion of the left Internal Carotid Artery (ICA). She was treated with steroids and surgical debulking of the tumour through trans-sphenoidal approach and postoperative imaging showed recanalization of the ICA with reduction of the tumour size. The histopathological diagnosis was consistent with pituitary macro adenoma. Patient improved in level of sensorium, eye movement and the patient showed almost full recovery after the operation. PA resulting in ICA occlusion is very rare. Early intervention is required for reducing mortality and morbidity and to improve quality of life.
Haemiplegia, Internal carotid artery, Pituitary haemorrhage, Visual failure
Case Report
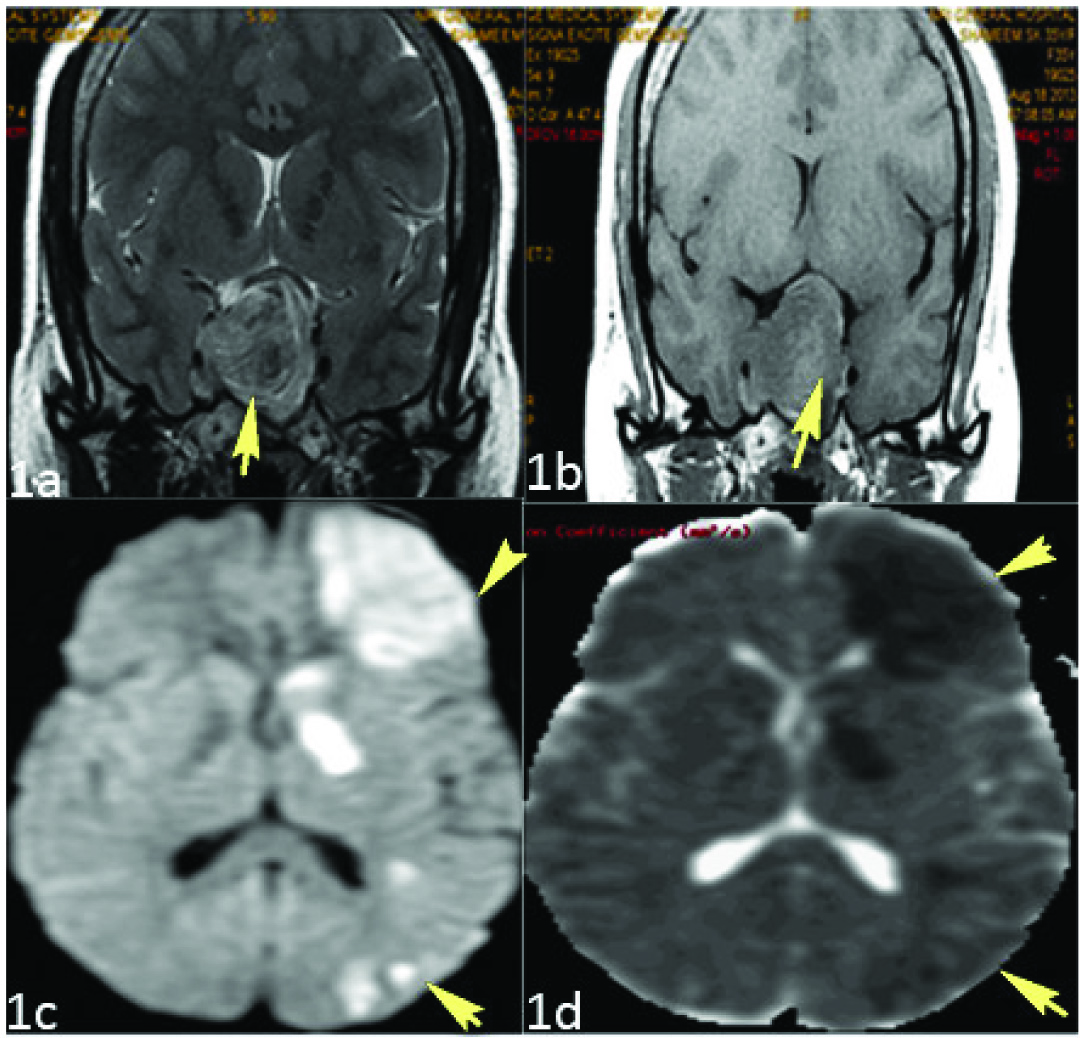
A 35-year-old young healthy lady presented with one day history of fever, right frontal headache, vomiting, drooping of right eyelid, visual failure in both eyes all concurring on same day evening. Next day fever, headache and vomiting subsided, but the patient had persistent visual failure and lid ptosis, however she could walk, verbalize and feed herself for initial three days of illness. She was imaged with MRI brain [Table/Fig-1a,b], which showed large suprasellar mass with left parasellar extension into the left cavernous sinus with T1 hyperintensity suggesting internal bleed probably pituitary macroadenoma with apoplexy. On the fifth day of illness, she had developed sudden onset difficulty in walking with right lower limb weakness which progressed to involve the right upper limb with inability to speak but able to comprehend minimally.
a-b MRI Brain, T2 and T1 coronals of pituitary showing a large lobulated macroadenoma in sella with changes of bleed (arrow); c-d: DWI-MRI Brain, hyperintensity on Diffusion Weighted Imaging (DWI) (arrow head) and corresponding Apparent Diffusion Coefficient (ADC) map showing hypointensity (arrow head) suggestive of acute infarcts in left apsuloganglionic, frontal and parietal lobes (left ICA acute infarct).
On examination she was conscious with Broca’s aphasia, right eyelid ptosis, bilateral visual failure to the extent of no perception of light with right eye, total ophthalmoplegia with bilateral mydriatic non reactive pupil (right more than left) and right haemiplegia with right seventh UMN (Upper Motor Neuron) facial palsy.
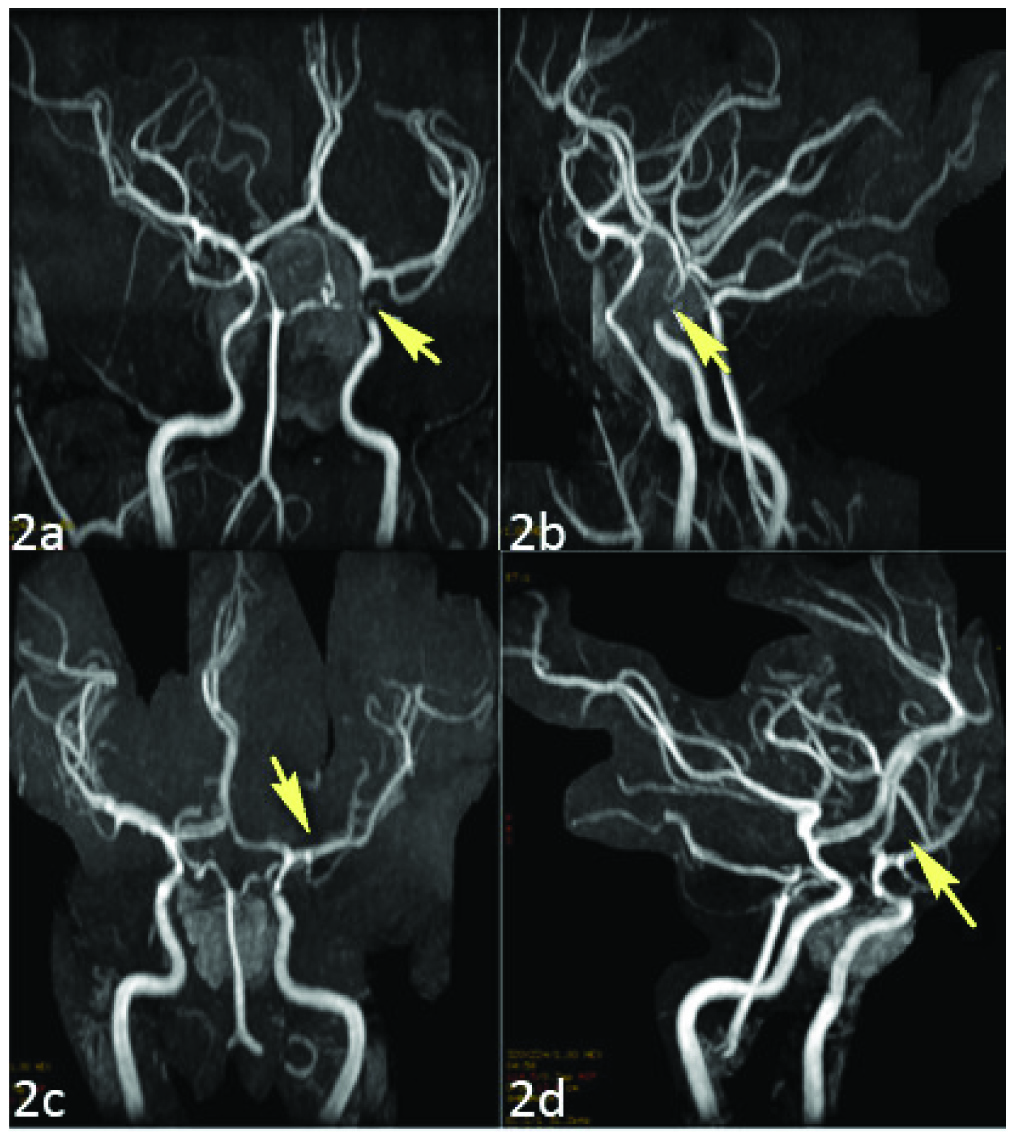
She was reimaged with MRI brain [Table/Fig-1c,d], revealing acute left ICA infarct with pituitary apoplexy in T2 and DWI sequences. Cerebral angiogram [Table/Fig-2a,b] revealed narrowing of bilateral ICA left side more than the right side. She had history of amenorrhea of one year without galactorrhea. She was the mother of four children (two neonatal deaths) with age of the last child being four years. She was non-diabetic and normotensive and she denied use of oral contraceptive pills. She was treated with steroids and subjected to definitive trans-sphenoidal resection of pituitary tumour. Postoperatively she was alert and eye movements were completely improved with slightly reactive pupils and vision improved to counting fingers to two meters with persistent lid ptosis. Two weeks later she could regain ability to speak and was ambulant with one-person support a week later. Two months postoperative imaging revealed complete resolution of tumour with complete recanalisation of ICA [Table/Fig-2c-d].
(a-b) Pre op MR 3D TOF angiogram show critical stenosis of the left cavernous ICA (arrow) with splaying of bilateral ICA. (c-d) Post op 3D TOF angiogram showing opening of the left cavernous ICA.
Evaluation revealed normocytic normochromic blood picture with negative viral parameters like HIV, HBsAg and HCV. Cardiac work up was normal through 2D Echocardiogram. We consider this tumour as non-secretory as levels of hormones (PRL, TSH, IGF-1) were within normal limits. Being a non-functioning (null-cell) tumour, post-operative medications like steroids or hormones were not advised. Despite the obvious aetiology of apoplexy, we made an attempt to rule out all causes of stroke in young like hypercoagulable states (normal protein C, S, ATIII, APLA, Homocysteine), vasculitidis (ANA, dsDNA) which were negative.
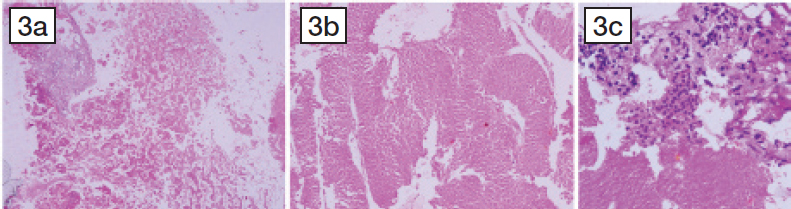
Histopathological examination [Table/Fig-3a-c] revealed large areas of infarcted pituitary adenoma with ghost outlines of relatively monomorphous cells in lobulous and sinusoidal pattern with adjoining areas showing sheets of foamy macrophages and a few lymphocytes suggestive of apoplexy.
(a) Section showing pituitary adenomatous tissue with inflammatory cells (lymphocytes) and extensive liquifactive necrosis (H&E X400); (b) Showing pituitary adenomatous tissue with haemosiderin pigment and ghost outlines of necrotic monomorphous tumour cells arranged in broad bands (H&E X400); (c) Showing pituitary adenomatous tissue with infarcted necrotic tumour with monomorphic cells (with roud cells, scant cytoplasm, dense nucleus) (H&E X400).
Discussion
Acute ischaemic stroke following PA is an extremely rare event and a few cases have been reported in the literature. Apoplexy occurs in 10% of intracranial tumours and 2-7% of pituitary adenomas [1].
PA results in a rapid increase in intrasellar contents with consequent sudden rise in Intrasellar Pressure (ISP) up to a median value of 47 mmHg [2]. Normal ISP is not known, but is believed to be similar or less than the normal intracranial pressure of 7–15 mmHg [3]. The sharp increase in ISP leads to disturbance of anterior pituitary cell viability, which could increase the risk of ischaemic necrosis and limit the potential for recovery of pituitary function.
Usually carotid artery strokes results in ipsilateral visual failure and contra lateral haemiplegias [4]. In our case bilateral visual failure was due to the tumour compressing the optic chiasm. Though bilateral cavernous sinuses are involved, it is the left sided ICA (carotid siphon), which produced contralateral right haemiplegia. Opthalmic manifestations in pituitary macroadenoma results from lateral expansion of the tumour compressing the III, IV and VI cranial nerves (causing ophthalmoplegia) and superior extension of the tumour compressing the optic nerve or optic chiasm (causing visual loss) [5,6]. Ptosis at the level of the cavernous sinus can be either due to palsy of parasympathetic third nerve, sympathetic plexus around ICA (Horner’s) or can be parasympathetico sympathetic palsy (Dilatation lag) [5].
The probable two most important mechanisms of cerebral ischaemic in patients with PA are mechanical obstruction of the circle of willis by the enlarging mass [7] and cerebral arterial vasospasm [8]. The ICA was occluded in the cavernous sinus or supraclinoid portion by the enlarged tumour in most cases [9]. The pathophysiology of vasospasm could be the release of vasoactive substances from the necrotic haemorrhagic tumour itself [8,10], hypothalamic dysfunction, intra-operative manipulation, direct arterial wall injury and the subarachnoid blood [11]. In our case the compression of cavernous portion of left ICA is the mechanism of ischaemic stroke.
There are only a few cases reporting mechanical compression of circle of willis as the chief event of cerebral ischaemic as illustrated by Rosenbaum TJ et al., Lath R and Rajshekar V et al., [12,13], and few other studies [7,9,14], while a few reporting cerebral vasospasm as the primary event [10,11,15-18]. Following [Table/Fig-4] reviews the published studies on association of acute ischaemic stroke following PA. Bilateral caudate nuclear infarcts secondary to PA was also described recently by Rebeiz T et al., [18].
Reviews the published studies on association of acute ischaemic stroke following pituitary apoplexy.
| Author | Age/ Sex | Symptoms | Days after onset | Vascular territory | Angiographical findings | Mechanism of Stroke |
|---|
| Rosenbaum TJ et al., [12] | 77/M | Stupor, Left Haemiparesis | 0 | Rt MCA | Rt ICA occlusion, Lt ICA stenosis | Compression |
| Cordoso ER and Peterson EW [10] | 34/F | Altered consciousness | 21 | Diffuse | Bilateral ICA, MCA, ACA stenosis | Vasospasm |
| Haens D et al., [15] | 43/M | Aphasia, Rt Haemiparesis | 0 | Bil ACAs | Lt ICA stenosis | Vasospasm |
| Pozzati E et al., [8] | 15/M | Drowsiness Rt facial palsy | 0 | Rt MCA | Bilateral ICA stenosis | Vasospasm |
| Clark JD et al., [14] | 40/M | Dysphagia, Rt haemiplegia, Rt facial palsy | 0 | Lt ACA | Rt ICA stenosis, Lt ICA occlusion | Compression |
| Itoyamma Y et al., [17] | 45/M | Rt Haemiparesis | 14 | _ | Lt ACA and MCA stenosis | Vasospasm |
| Lath R and Rajshekar V [13] | 40/M | Lt Haemiplegia | 1 | Rt ACA | - | Compression |
| Akutsu H et al., [16] | 29/M | Drowsiness Lt Haemiplegia | 5 | Lt Heubner’s and medial lenticulo striate arteries | Lt ACA mild stenosis | Vasospasm |
| Rebeiz T et al., [18] | 81/F | Stupor, blindness, quadriparesis | 0 | Bil ACA/MCA MCA/PCA | Anterior displacement of ACA | Compression |
| Present case | 35/F | Headache, right Haemiplegia, blindness | 3 | Lt MCA | Left ICA Stenosis | Compression |
Conclusion
Acute ischaemic stroke following PA is very rare. High index of suspicion is required in every case of sellar lesions to identify the signs of neurovascular compromise to prevent lethal complications. Surgical decompression through the trans-sphenoidal approach is appropriate. Early intervention is required to reduce the mortality and morbidity and to increase health related quality of life.
[1]. Cardoso ER, Peterson EW, Pituitary apoplexy: A reviewNeurosurgery 1984 14:363-73. [Google Scholar]
[2]. Zayour DH, Selman WR, Arafah BM, Extreme elevation of intrasellar pressure in patients with pituitary tumour apoplexy: relation to pituitary functionJ Clin Endocrinol Metab 2004 89:5649-54. [Google Scholar]
[3]. Kruse A, Astrup J, Cold GE, Hansen HH, Pressure and blood flow in pituitary adenomas measured during transsphenoidal surgeryBr J Neurosurg 1992 6:333-41. [Google Scholar]
[4]. Lavallée PC, Cabrejo L, Labreuche J, Mazighi M, Meseguer E, Guidoux C, Spectrum of transient visual symptoms in a transient ischemic attack cohortStroke 2013 44(12):3312-17. [Google Scholar]
[5]. Lee CC, Cho AS, Carter WA, Emergency department presentation of pituitary apoplexyAm J Emerg Med 2000 18:328-31. [Google Scholar]
[6]. Verrees M, Arafah BM, Selman WR, Pituitary tumour apoplexy; characteristics, treatments, and outcomesNeurosurgery Focus 2004 16:1-7. [Google Scholar]
[7]. Yang SH, Lee KS, Lee KY, Lee SW, Hong YK, Pituitary apoplexy producing internal carotid artery compression: a case reportJ Korean Med Sci 2008 23:1113-17. [Google Scholar]
[8]. Pozzati E, Frank G, Nasi MT, Giauliani G, Pituitary apoplexy bilateral carotid vasospasm, and cerebral infarction in a 15-year-old boyNeurosurgery 1987 20:56-59. [Google Scholar]
[9]. Chokyu I, Tsuyuguchi N, Goto T, Chokyu K, Chokyu M, Ohata K, Pituitary apoplexy causing internal carotid artery occlusion—case reportNeurol Med Chir (Tokyo) 2011 51(1):48-51. [Google Scholar]
[10]. Cardoso ER, Peterson EW, Pituitary apoplexy and vasospasmSurg Neurol 1983 20:391-95. [Google Scholar]
[11]. Jeon BC, Park YS, Oh HS, Kim YS, Chun BK, Pituitary apoplexy complicated by chemical meningitis and cerebral infarctionJ Korean Med Sci 2007 22(6):1085-89. [Google Scholar]
[12]. Rosenbaum TJ, Houser OW, Laws ER, Pituitary apoplexy producing internal carotid artery occlusionJ Neurosurg 1977 47:599-604. [Google Scholar]
[13]. Lath R, Rajshekar V, Massive cerebral infarction as a feature of Pituitary apoplexyNeurol India 2001 49:191-93. [Google Scholar]
[14]. Clark JD, Freer CE, Wheatly T, Pituitary apoplexy: an unusual cause of strokeClin Radiol 1987 38:75-77. [Google Scholar]
[15]. Haens D, Baleriaux D, Mockel J, Apoplexie hypophysaire ischemique et accident vasculaire cerebralNeurochirurgie 1983 29:401-05. [Google Scholar]
[16]. Akutsu H, Noguchi S, Tsunoda T, Sasaki M, Matsumura A, Cerebral infarction following pituitary apoplexy—case reportNeurol Med Chir (Tokyo) 2004 44:479-83. [Google Scholar]
[17]. Itoyama Y, Goto S, Miura M, Kuratsu J, Ushio Y, Matsumato T, Intracranial arterial vasospasm associated with pituitary apoplexy after head trauma-case reportNeurol Med Chir(Tokyo) 1990 30:350-53. [Google Scholar]
[18]. Rebeiz T, Cueva W, Ardelt A, Unusual case of bilateral caudate infarcts following pituitary apoplexyJAMA Neurol 2014 71:226-27. [Google Scholar]