Intracorneal Amphotericin B Injection in a Case of Indolent Candidal Keratitis
Jyoti Deswal1, Sudesh Kumar Arya2
1 Senior Resident, Department of Ophthalmolgy, GMCH, Chandigarh, India.
2 Professor, Department of Ophthalmology, GMCH, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jyoti Deswal, Senior Resident, Department of Ophthalmolgy, H.NO. 25/10-A, Jasbir Colony (Near Sheela By-Pass), Rohtak-124001, Haryana, India.
E-mail: jyoti_deswal@yahoo.co.in
Ocular candidiasis is one of the opportunistic infection occurring in human body. Pathogenesis wise, Candida is very virulent and slow growing organism. We report a case of 76-year-old female with left eye candidal stromal abscess, not responding to topical and oral antifungal drugs. Patient was administered intrastromal amphotericin B injection in the affected eye. Four midstromal injections were given in the areas surrounding the corneal abscess. A total of approximately 0.05 mL of amphotericin B, 5 μg per 0.1 mL, was administered. Within next four weeks, the eye became completely quiet with healed epithelial defect and corneal scarring. Intracorneal injection of amphotericin B is a safe and effective treatment option for recurrent and recalcitrant fungal infections.
Abscess, Candida, Intrastromal, Photophobia
Case Report
A 76-year-old female presented with complaint of painful decrease in vision in left eye for the last one month. The decrease in vision was associated with photophobia and redness. There was no history of any trauma or entry of any foreign body in the eye. The patient was non-diabetic and did not have any systemic illness.
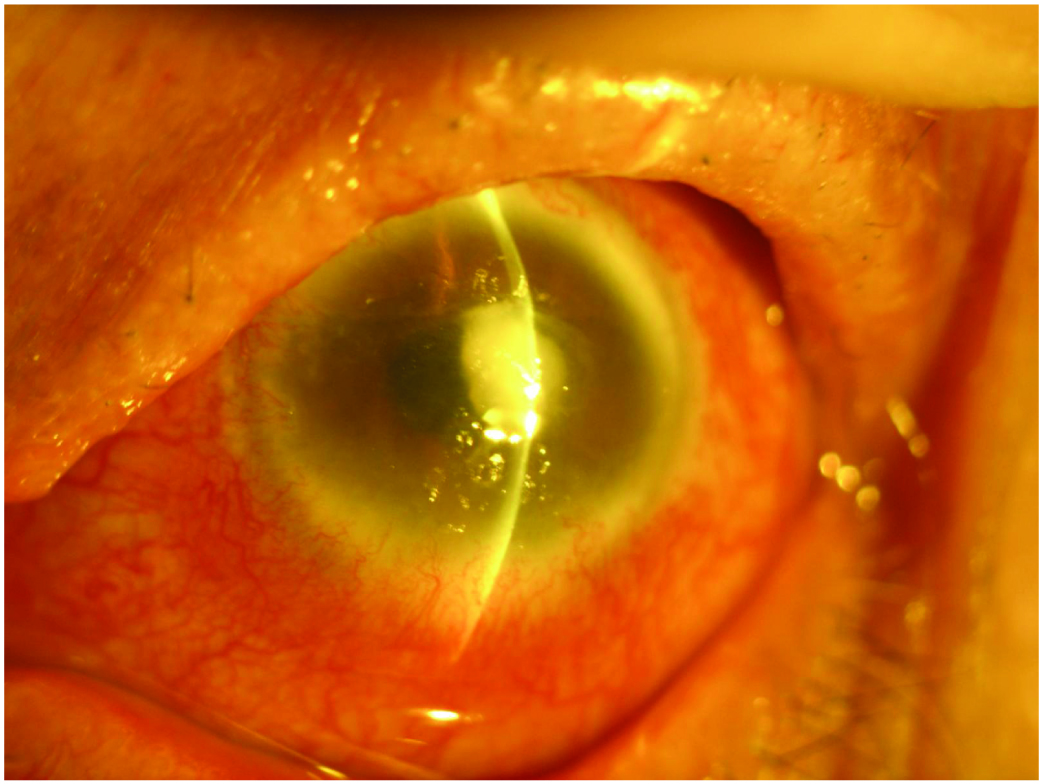
On examination, patient was thin built and well-nourished. Best corrected visual acuity in right eye was 6/12 and Finger Counting (FC) 1m with accurate Projection of Rays (PR) in left eye. Right eye was essentially normal except presence of immature senile cataract. In left eye, slit lamp examination revealed circumciliary congestion with thick creamish-white stromal corneal infiltrates upto 90% of corneal depth with overlying epithelial defect measuring 4 x 3.5 mm in the central part of cornea. There was surrounding stromal oedema with superficial vascularization all around the cornea. Anterior chamber reaction was 2+ with no hypopyon [Table/Fig-1].
Showing thick anterior stromal corneal infiltrates with overlying epithelial defect measuring 4 x 3.5 mm in the central part of cornea;
Patient was already on treatment before coming to us. She had been putting topical moxifloxacin 0.5% and natamycin 5% at two hourly intervals along with cycloplegic and artificial tears for the past two weeks. The clinical picture was suggestive of infection caused by an indolent organism. Corneal scrapings were sent for gram stain, KOH mount and culture. KOH mount revealed presence of yeast.
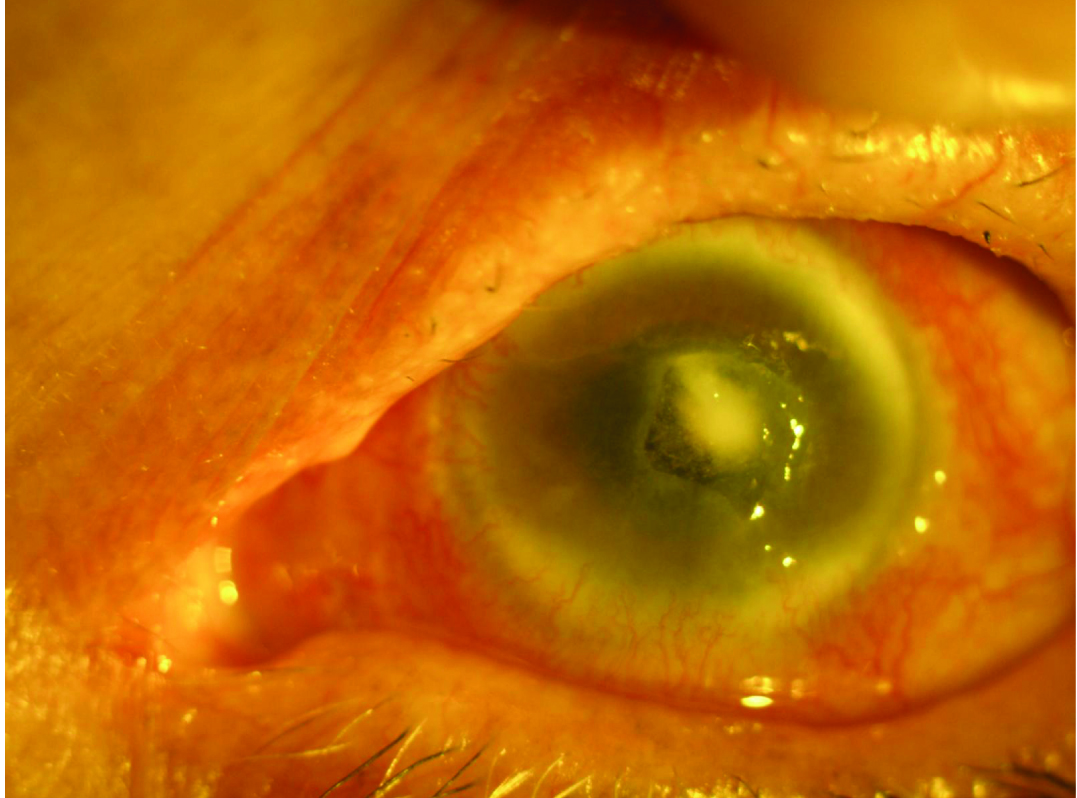
The treatment was revised and topical amphotericin B (0.25%) drops were added at two hour intervals. Patient did not respond to topical antifungal treatment as the size of stromal abscess remained the same for next few days. The patient was then administered intrastromal amphotetericin B injection in the affected eye with the patient in supine position, using a 1 mL syringe with a 30-gauge needle with bevel down. Four mid-stromal injections were given in the areas surrounding the corneal abscess in all the four quadrants, 0.5 mm away from abscess margin and upto mid-stromal depth. A total of approximately 0.05 mL of amphotericin B, 5 μg per 0.1 mL, was administered, resulting in hydration of the cornea. Within next few days, the size of stromal infiltrates reduced to 2 x 2 mm, the depth of infiltrates decreased as they were now present only in anterior stroma, size of epithelial defect decreased to 3 x 3 mm and corneal oedema and circumciliary congestion reduced markedly [Table/Fig-2].
Showing reduction in size of stromal abscess three days after intrastromal injection of amphotericin B.
Repeat injections were not given and patient was advised to follow same treatment regime as earlier. Within next four weeks, the eye became completely quiet with healed epithelial defect and corneal scarring. On three months follow-up, patient was asymptomatic with central macular corneal opacity of size 3 x 3 mm.
Discussion
Corneal tissue is most susceptible to fungal infections amongst all the ocular tissues. In India, prevalence of fungal keratitis ranges from 7.3 to 44.8% [1]. Filamentous fungi are more prevalent in tropical regions and yeasts, specifically candida, in temperate. Excessive use of antibiotics and corticosteroids, contact lens wear, trauma with vegetative matter and immunodeficiency are the risk factors for candida infection [2]. Candida species show morphological transition between yeast and hyphal forms due to mechanism of phenotypic switching. Expression of adhesions and invasions on the cell surface, formation of biofilms and secretion of hydrolytic enzymes make candida highly virulent [3].
Mainstay therapy for candida infection is topical amphotericin B and oral azoles. Flucytosine and fluconazole have also been recommended for the treatment of candida infection in the eye. Topical voriconazole also has good bioavailability and activity [4]. In 1/3rd of cases, penetrating keratoplasty may be required [5]. Efficacy of amphotericin B is closely dependent on the ability to achieve its optimal levels in the cornea. So, selecting a proper formulation and mode of application is the key to improve the efficacy of amphotericin B. Ophthalmologists have tried site-directed drug delivery in the form of intracameral injections, intrastromal injections, and posterior sub-tenon injections [6-10]. Intracorneal drug delivery has been performed previously on animals in an experimental setting [11]. A literature search produced one report of a bioassay in rabbits in which several antifungal agents were evaluated in an effort to achieve therapeutic corneal levels [12]. In a study by Qu L et al., on rabbit model, the concentrations of amphotericin B in the cornea and aqueous humor using three different routes of administration were measured, and comparisons of concentrations with each other were made. They reported that a single intrastromal injection of amphotericin B could raise the local drug concentration in the deep cornea, high concentrations being maintained for seven days or longer. Intrastromal injection is simple, less invasive, and can directly deliver drug into the deep cornea. Intrastromal injection can be repeated after seven days or later, avoiding high injection frequency, which might cause anthropogenic trauma to the cornea. Intracameral injection may be a sort of efficacy therapy for intraocular fungal extension and corneal infection that penetrated the endothelium into the anterior chamber. But the aqueous concentrations decreased abruptly within one day after a single injection [13]. In some studies on rabbits, it is reported that intrastromal injection of amphotericin B at a concentration of less than 10 μg per 0.1 mL is safe in rabbit corneas [14], and at a concentration of 5 μg per 0.1 mL it does not appear to be deleterious to keratocytes or endothelial cells in the clinic [6]. Up to 50 μg of intracamerally injected amphotericin B is also well tolerated by rabbit eyes, and it causes only reversible iritis and clouding of the lens [15]. Consistent with our experience reported herein, intrastromal injections of amphotericin B at a concentration of 5 μg per 0.1 mL do not appear to be deleterious to corneal keratocytes or endothelial cells.
Conclusion
We suggest intracorneal injection of amphotericin B is a safe and effective treatment option for recurrent and recalcitrant fungal infections. Intrastromal corneal injections of amphotericin B offer less invasive, in-office alternative to penetrating keratoplasty.
[1]. Rautaraya B, Sharma S, Kar S, Das S, Sahu SK, Diagnosis and treatment outcome of mycotic keratitis at a tertiary eye care center in eastern IndiaBMC Ophthalmol 2011 11:39-47. [Google Scholar]
[2]. Hemady RK, Microbial keratitis in patients infected with the human immunodeficiency virusOphthalmology 1995 102:1026-30. [Google Scholar]
[3]. Mayer FL, Wilson D, Hube B, Candida albicans pathogenicity mechanismsVirulence 2013 4:119-28. [Google Scholar]
[4]. Sengupta J, Khetan A, Saha S, Banerjee D, Gangopadhyay N, Pal D, Candida keratitis Emerging problem in IndiaCornea 2012 31:371-75. [Google Scholar]
[5]. Xie L, Dong X, Shi W, Treatment of fungal keratitis by penetrating keratoplastyBr J Ophthalmol 2001 85:1070-74. [Google Scholar]
[6]. Garcia-Valenzuela E, Song CD, Intracorneal injection of amphothericin B for recurrent fungal keratitis and endophthalmitisArchives of Ophthalmology 2005 123(12):1721-23. [Google Scholar]
[7]. Yilmaz S, Ture M, Maden A, Efficacy of intracameral amphotericin B injection in the management of refractory keratomycosis and endophthalmitisCornea 2007 26(4):398-402. [Google Scholar]
[8]. Kuriakose T, Kothari M, Paul P, Jacob P, Thomas R, Intracameral amphotericin B injection in the management of deep keratomycosisCornea 2002 21(7):653-56. [Google Scholar]
[9]. Sharma N, Agarwal P, Sinha R, Titiyal JS, Velpandian T, Vajpayee RB, Evaluation of intrastromal voriconazole injection in recalcitrant deep fungal keratitis: case seriesBritish Journal of Ophthalmology 2011 95(12):1735-37. [Google Scholar]
[10]. Sharma N, Chacko J, Velpandian T, Titiyal JS, Sinha R, Satpathy G, Comparative evaluation of topical versus intrastromal voriconazole as an adjunct to natamycin in recalcitrant fungal keratitisOphthalmology 2013 120(4):677-81. [Google Scholar]
[11]. Claudio C, Gino G, Homologous antilymphocyte antibodies synthesized by limbocorneal lymphoid foci during the delayed hypersensitivity phase: analysis of the limbal immunologic reaction after intracorneal injection of homospecific spleen homogenateRiv Anat Patol Oncol 1968 33:336-50. [Google Scholar]
[12]. O’Day DM, Head WS, Robinson RD, Williams TE, An evaluation of intrastromal injection of antifungal agentsJ Ocul Pharmacol 1991 7:325-28. [Google Scholar]
[13]. Qu L, Li L, Xie H, Corneal and aqueous humor concentrations of amphotericin B using three different routes of administration in a rabbit modelOphthalmic Research 2010 43(3):153-58. [Google Scholar]
[14]. Qu L, Li L, Xie H, Toxicity and pharmacokinetics of intrastromal injection of amphotericin B in a rabbit modelCurrent Eye Research 2014 39(4):340-47. [Google Scholar]
[15]. Foster JB, Almeda E, Littman ML, Wilson ME, Some intraocular and conjunctival effects of amphotericin B in man and in the rabbitArchives of Ophthalmology 1958 60(4):555-64. [Google Scholar]