Staged Approach for Advanced Gingival Recession: Free Gingival Autograft Followed by Coronally Advanced Flap with PRF Membrane
Sowmiya Lingeshwaran1, Ramakrishnan Theyagarajan2, Ambalavanan Namasivayam3
1 Senior Lecturer, Department of Periodontics, Meenakshi Ammal Dental College and Hospital, Chennai, Tamil Nadu, India.
2 Professor and Head, Department of Periodontics, Adhiparasakthi Dental College and Hospital, Chennai, Tamil Nadu, India.
3 Professor and Head, Department of Periodontics, Meenakshi Ammal Dental College and Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sowmiya Lingeshwaran, Allapakam Main Road, Maduravoyil, Chennai-600095, Tamil Nadu, India.
E-mail: drsowmiyal@gmail.com
Attached gingiva, Periodontal plastic surgery, Regeneration
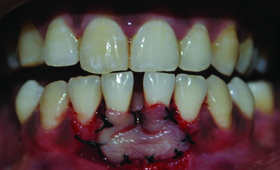
A 37-year-old female reported with chief complaint of severe sensitivity in lower front tooth region for past six months while intake of cold food items. On history, she reported with a faulty brushing habit and on clinical examination, the affected site revealed Miller’s [1] Class II buccal recession (31, 41) in the mandibular front tooth region [Table/Fig-1].
Preoperative view depicting recession in 31, 41.

Clinical parameters were recorded using Williams periodontal probe.
Presurgical therapy
Full-mouth scaling and polishing followed by thorough planning of exposed root surface was performed four weeks before the commencement of the surgery followed by which oral hygiene instructions were given to eliminate habits related to the aetiology of the recession.
Surgical protocol
Stage 1: Free gingival autograft
Pre-rinse was given for intraoral disinfection with 0.12% chlorhexine (CHX) mouth rinse. The surgical field was isolated; the operative sites were anaesthetized using 2% xylocaine hydrochloride with adrenaline (1:200000). The recipient bed was prepared apical to the area of recession by giving a horizontal incision using Bard- parker No:15 blade (kehr surgical private ltd) along the mucogingival junction which extended upto the non affected tooth site (32, 42) on either sides [Table/Fig-2]. Free gingival autograft was obtained from the palate and was adapted onto the recipient bed. The free gingival graft was immobilized and secured using 4-0 black silk suture [Table/Fig-3].
Preparation of the recipient site.

Transfer of the graft and secured with 4-0 silk suture.
Postoperative care: Systemic antibiotics (amoxycillin 500 mg three times a day for seven days) and analgesics (ibuprofen 400 mg three times a day for five days) with instructions to rinse the mouth daily with a solution of 0.2% CHX for seven days. There was significant augmentation of attached gingiva and some reduction in the size of the recession after three months [Table/Fig-4].
Healing after three months.

Stage 2: Coronally advanced flap with Platelet rich fibrin (PRF) membrane
After the achievement of complete healing, the second stage surgery was performed. PRF membrane was prepared by using a tabletop centrifuge (Remi R8C Laboratory®). Coronally Advanced Flap (CAF) was done by giving intrasulcular incision and full thickness flap was raised to expose denuded root surface [Table/Fig-5] and beyond which it was continued as partial thickness flap so that it can be repositioned coronally without any tension. PRF membrane was placed on the denuded root surface [Table/Fig-6] and simple interrupted suture was placed to advance the flap coronal to the cementoenamel junction [Table/Fig-7]. Surgical site was covered with periodontal dressing (Coe-Pak). Patient was put under strict maintenance protocol. After six months postoperative measurements were recorded [Table/Fig-8] which showed significant gain in the width of the attached gingiva with good aesthetic root coverage [Table/Fig-9].
Reflected Mucoperiosteal flap showing the denuded root surface.

PRF membrane was positioned against denuded root surface.

Flap was coronally positioned and sutured.

Clinical parameters measured at baseline and after six months.
| Measurements | Preoperative | Postoperative(after six months) |
|---|
| 31 | 41 | 31 | 41 |
|---|
| Probing pocket depth | 2.0 mm | 1.0 mm | 1.0 mm | 1.0 mm |
| Width of attached gingiva | 0.5 mm | 2.0 mm | 5.5 mm | 7.0 mm |
| Clinical attachment loss | 8.0 mm | 6.0 mm | 2.0 mm | 1.0 mm |
| Recession height | 6.0 mm | 5.0 mm | 1.0 mm | 0.0 mm |
| Recession width | 4.0 mm | 3.0 mm | 1.0 mm | 0.0 mm |
A six months postoperative view.

Numerous approaches are in practise to treat mild gingival recession but not for severe gingival recessions because of unpredictable success rate. However, Blanes RJ and Allen EP [2] stated that the achievement of root coverage is possible in cases where the interproximal soft tissue remained intact. In this case, free gingival autograft was done to increase the width of the attached gingiva followed by the CAF with PRF membrane as this technique was first described by Bernimoulin JP et al., [3].
Baiju RM et al., achieved superior results when PRF was combined with CAF [4]. Mishra D et al., concluded that when CAF used along with PRF results in better aesthetic outcome with gain in clinical attachment and width of keratinized tissue [5]. Mhaske M et al., reported PRF as a boon as it provides complete root coverage when used in combination with pedicle flap [6].
The two-stage surgical procedure is highly predictable for root coverage in the case of severe gingival recessions with inadequate attached gingiva. PRF membrane gave promising clinical outcome when combined with CAF in the present case. But, there is a need for long term clinical trials to prove the efficacy of this technique.
[1]. Miller PD, Aclassification of marginal tissue recessionInt J Periodontics Restorative Dent 1985 5(2):08-13. [Google Scholar]
[2]. Blanes RJ, Allen EP, The bilateral pedicle flap-tunnel technique: a new approach to cover connective tissue graftsInt J of Periodontics Restorative Dent 1999 19(5):471-79. [Google Scholar]
[3]. Bernimoulin JP, Luscher B, Mühlemann HR, Coronally repositioned periodontal flap. Clinical evaluation after one yearJ Clin Periodontol 1975 2:01-13. [Google Scholar]
[4]. Baiju RM, Ahuja R, Ambili G, Janam P, Autologous platelet-rich fibrin: a boon to periodontal regeneration - report of two different clinical applicationsHealth Sciences 2013 2:01-13. [Google Scholar]
[5]. Mishra D, Kalapurakkal VB, Misra SR, Using platelet rich fibrin and synthetic collagen membrane. a report of two casesJ Clin Diagn Res 2015 9(10):01-0.4. [Google Scholar]
[6]. Mhaske M, Thakur N, Raut S, Coronally advanced flap along with autologous platelet rich fibrin: boon for recession coverage- a case reportIJCMR 2016 3:1190-93. [Google Scholar]