Hoarseness of voice due to Vocal Cord Palsy (VCP) resulting from aortic aneurysm is a rare entity. Hoarseness due to left Recurrent Laryngeal Nerve (RLN) paralysis caused by identifiable cardiovascular disease has been described as Ortner’s syndrome or Cardiovocal syndrome. Very rarely, thoracic aortic aneurysm can cause Phrenic Nerve (PN) palsy causing hemidiaphragm paralysis. But, aortic aneurysm causing both RLN and PN palsy is an extremely rare occasion. Our literature review showed only three cases of combined RLN and PN palsy due to thoracic aortic aneurysm. Here we report a 70-year-old patient having hoarseness of voice for six years for which he was on symptomatic treatment. He presented to us with cough and blood tinged sputum, left sided chest pain, loss of appetite and weakness since two months duration. Based on clinical history and chest radiograph, lung malignancy was suspected. To our surprise, Contrast Enhanced Computed Tomography (CECT) revealed partially thrombosed saccular thoracic aneurysm originating distal to origin of left subclavian artery. He was referred to the cardiothoracic vascular surgeon for surgical treatment, but was reluctant to go for surgery. He is now being followed up by cardiothoracic vascular surgery and cardiology department and his condition has remained the same.
Computed tomography, Hoarseness, Ortners’ syndrome, Thoracic malignancy, Vocal cord paralysis
Case Report
A 70-year-old male patient presented with left sided chest pain, cough with blood tinged sputum, loss of appetite and weakness since two months. He had history of hoarseness of voice for six years. He had no significant medical or surgical history. He was a non-smoker. No other significant neurological or cardiorespiratory symptoms were found. There was no family history of malignancy or connective tissue disorders. He was admitted to Pulmonary Medicine Department due to suspected thoracic malignancy.
On physical examination, his vitals were within normal limits. There was no cervical lymphadenopathy, clubbing and engorged neck vein. Routine blood test was normal. Sputum AFB staining and cytology for malignant cells were all negative.
Fiberoptic laryngoscopy revealed left VCP without any mass lesion in the larynx and paramedian position of the left vocal cord.
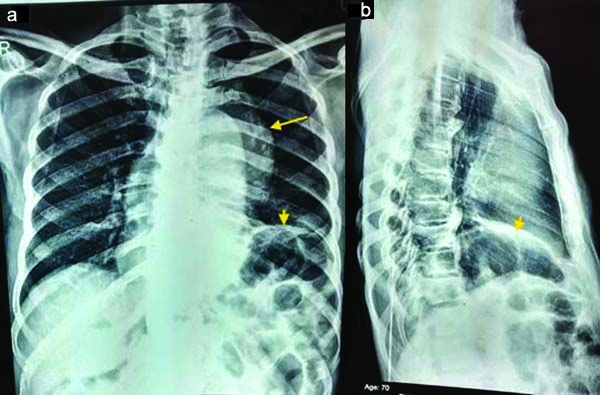
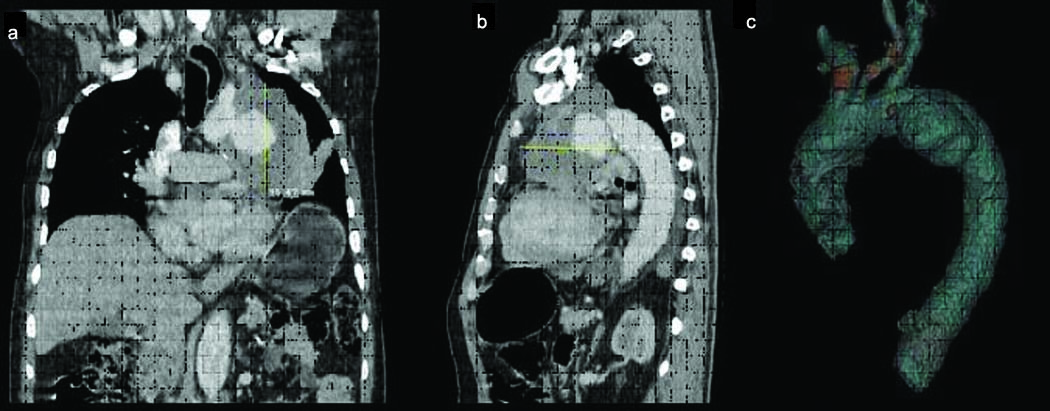
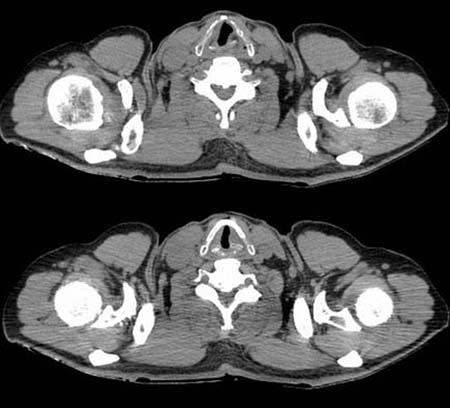
Right vocal cord showed normal position. Chest radiograph revealed large bulging contour overlying aorta and left hilar shadow along with elevated left hemidiaphragm [Table/Fig-1]. Hilar mass couldn’t be ruled out and patient was suggested for a CECT of the thorax to evaluate for the possible neoplastic etiology in neck or chest. CECT of the thorax revealed a partially thrombosed saccular aneurysm originating from arch of aorta distal to origin left subclavian artery. The size of aneurysm was 8.2×7.8×9.5 cm (Anteroposterior× Transverse×Craniocaudal) [Table/Fig-2]. Left vocal cord was in paramedian positon on neck CT [Table/Fig-3].
Chest radiograph a) posteroanterior (PA) view and b) lateral view showing lobular bulging contour overlying aorta (long arrow) with elevated left hemidiaphragm (short arrow).
a, b) Contrast enhanced CT showing a partial thrombosed saccular aneurysm of aortic arch just distal to origin of left subclavian artery; c) A 3D volume rendered image well depicts the aneurysm.
Neck CT at the level of the larynx showing anteromedial deviation of the left arytenoid cartilage suggestive of vocal cord paralysis.
The final diagnosis of Ortner’s syndrome with left PN palsy due to thoracic aortic aneurysm was made on the basis of clinical presentation and CT aortographic appearance. Aortic aneurysm was responsible for stretching or compression of the left RLN and PN with resultant left vocal cord and PN palsy.
He was referred to the cardiothoracic vascular surgeon for surgical intervention, but refused to go for surgery. He underwent medical management with antihypertensive and antilipidemic drugs. He was explained the risk of impending rupture and advised regular follow up by cardiothoracic vascular surgery and cardiology department. His condition has remained essentially the same till now.
Discussion
Hoarseness of voice due to RLN palsy and elevated hemidiaphragm due to PN palsy can sometimes point to a very serious underlying pathology, such as thoracic aortic aneurysm [1-4]. But, it is extremely unusual to find their association in the same patient.
Norbert Ortner, an Austrian physician, in 1897 described three cases of left RLN palsy due to mitral stenosis which he termed as Ortner’s syndrome or cardiovocal syndrome. Many cardiopulmonary conditions are associated with this syndrome including mitral stenosis, mitral valve prolapse, aortic aneurysm, left ventricular aneurysm, septal defect, following cardiothoracic surgery, primary pulmonary hypertension, ductal aneurysm, aortic dissection and so on [5]. The most common cause is mitral valve stenosis with prevalence of 0.6–5%. There are only few reports of combination of RLN and PN palsy due to aortic aneurysm [6-8]. Another interesting feature of our case is that the patient had a long history of hoarseness of voice (six years) without any complication of aneurysm. The patient was alive at the time of writing the case report.
An aortic aneurysm is said to be present when there is a focal permanent dilatation of at least 1.5 times greater than its normal calibre [9]. Morphologically, it can be classified as saccular and fusiform types. Atherosclerosis is the most common cause. Other causes include hypertension, smoking, advanced age, trauma, connective tissue disorders such as the Marfan and Ehler-Danlos syndromes. Thoracic aneurysms are mostly asymptomatic and often diagnosed incidentally on chest X-ray. Sometimes it presents with chest pain due to compression or erosion of surrounding structures. Only 5% of cases of thoracic aortic aneurysm present with hoarseness of voice [10]. Association with phrenic nerve palsy is also rare. To the best of our knowledge, there are only three cases of both RLN and PN palsy reported in world literature [6-8]. Rabago G et al., in 1999 described a patient with chronic aneurysm of descending thoracic aorta presenting with elevated left hemi-diaphragm secondary to left PN palsy without hoarseness of voice [4]. Right PN palsy is very rare and only one case has been reported [6].
PN palsy is mostly idiopathic. Identifiable causes include malignancy such as bronchogenic carcinoma, mediastinal and neck tumours and penetrating injury. Iatrogenic trauma can also lead to PN palsy as in, during cardiac surgery and central venous catheterisation [6,8].
The left RLN follows an intimate anatomic course to the aortic arch, left lung apex, trachea, oesophagus, left pulmonary artery, and mediastinal lymph nodes with much of its course being mediastinal. It has long circuitous course. The right RLN is 5-6 cm in length whereas the left RLN is nearly 12 cm in length. These factors make the left RLN more vulnerable to compression neuropathy from mediastinal abnormalities than right RLN [11,12].
The most frequent causes of paralysis are tumours of the lung, oesophagus and thyroid. VCP is also associated with many cardiovascular diseases, such as pulmonary hypertension, mitral stenosis, mitral valve prolapse, aortic aneurysm, septal defect, following cardiothoracic surgery, high altitude pulmonary hypertension, ductal aneurysm, aortic dissection where it is called Ortner’s syndrome [1,2,12].
The proposed mechanism of left RLN palsy secondary to aortic aneurysm is compression of nerve between the pulmonary artery and the aorta as it hooks around the ligamentum arteriosum [13].
Lung cancer (42%) is the commonest cause of unilateral VCP followed by iatrogenic cause (24%) [2]. As previously mentioned, only 5% cases of thoracic aortic aneurysm clinically manifest with hoarseness of voice. So, it is common to suspect lung malignancy as the cause of hoarseness of voice in the clinical setting of old age, cough and dyspnoea, as in our case. However, it is very important to keep cardiovascular causes such as aortic aneurysm as the cause of hoarseness of voice to avoid inappropriate interventions and treat this potential catastrophic condition.
CT scan with contrast from skull base to mid thorax that includes the peripheral pathway of the vagus, and the RLN is of paramount importance in patients with vocal cord paralysis after ruling out laryngeal pathology by laryngoscopy. It is also the best modality to assess aortic aneurysm and its complication thereby helping in timely management [3].
According to Ohki M, RLN palsy might be prodrome of aneurysm rupture. However, in our case the patient was having hoarseness of voice for six years without any aneurysmal complications [13].
Surgical correction is the treatment of choice and is advised based on its size, growth rate and symptoms. It can be done by open surgical repair and endovascular stent graft aneurysm repair [14].
Recovery from RLN palsy after both types of surgery may take from six to 12 months. But this does not happen always. Delayed recovery of PN palsy may persist at 12 to 14 postoperative months, in accordance with the known rate of regeneration of peripheral nerves [4,13].
Conclusion
Hoarseness of voice as the presenting feature of thoracic aortic aneurysm is rare. Its association with PN palsy is extremely rare. A thorough history, clinical examination, and investigations (laryngoscopy and CECT from skull base to thorax) are necessary to evaluate a case of hoarseness of voice. Thoracic aortic aneurysm is important cardiovascular cause of VCP. Early intervention is required to avoid fatal complications, hence the role of CT is important in prompt diagnosis.
[1]. Rizvi MM, Singh RB, Jain A, Sarkar A, Asymptomatic aortic aneurysm causing right vocal cord palsy and hoarseness: A rare presentationAnesthesia, Essays and Researches 2014 8(3):397-400. [Google Scholar]
[2]. Wang H-W, Chen M-C, Chao P-Z, Lee F-P, Cardiovocal syndrome secondary to an aortic aneurysmCase Reports in Otolaryngology 2016 (9):867-942. [Google Scholar]
[3]. Elzamzamy UA, Joharjy IA, Thoracic aortic aneurysm presenting only as vocal cord paralysisNeurosciences 2007 12(3):245-48. [Google Scholar]
[4]. Rábago G, Martín-Trenor A, López-Coronado JL, Chronic aneurysm of the descending thoracic aorta presenting with right pleural effusion and left phrenic paralysisTexas Heart Institute Journal 1999 26(1):96-98. [Google Scholar]
[5]. Chan P, Lee CP, Ko JS, Hung JS, Cardiovocal (Ortner’s) syndrome: left recurrent laryngeal nerve palsy associated with cardiovascular diseasesEur J Med 2004 11:69-70. [Google Scholar]
[6]. Akhtar J, Siddiqui MA, Khan NA, Alam MA, Right phrenic nerve palsy: a rare presentation of thoracic aortic aneurysmMalays J Med Sci 2013 20(4):98-101. [Google Scholar]
[7]. Joseph TK, Nair RM, Combined recurrent laryngeal and phrenic nerve paralysis due to aortic arch aneurysmInt J Phonosurg Laryngol 2013 3(2):58-60. [Google Scholar]
[8]. Ejazi MA, Alam MM, Shameem M, Bhargava R, Adil Wafi C, Salauddin Thoracic aortic aneurysm: A rare cause of elevated hemidiaphragm 2016 33(4)Lung IndiaOfficial Organ of Indian Chest Society:430-33. [Google Scholar]
[9]. Lavall D, Schafers HJ, Bohm M, Laufs U, Aneurysms of the ascending aortaDtsch Arztebl Int 2012 109(13):227-33. [Google Scholar]
[10]. Teixido MT, Leonetti JP, Recurrent laryngeal nerve paralysis associated with thoracic aortic aneurysmOtolaryngol Head Neck Surg 1990 102:140-44. [Google Scholar]
[11]. Paquette CM, Manos DC, Psooy BJ, Unilateral vocal cord paralysis: a review of CT findings, mediastinal causes, and the course of the recurrent laryngeal nervesRadioGraphics 2012 32(3):721-40. [Google Scholar]
[12]. Zangirolami ACA, Oliveira FV de, Tepedino MS, Ortner’s syndrome: secondary laryngeal paralysis caused by a great thoracic aorta aneurysmInternational Archives of Otorhinolaryngology 2015 19(2):180-82. [Google Scholar]
[13]. Ohki M, Thoracic saccular aortic aneurysm presenting with recurrent laryngeal nerve palsy prior to aneurysm rupture: a prodrome of thoracic aneurysm rupture?Case Rep Otolaryngol 2012 2012:367873 [Google Scholar]
[14]. Bavaria JE, Appoo JJ, Makaroun MS, Verter J, Yu ZF, Mitchell RS, Gore TAG Investigators. Endovascular stent grafting versus open surgical repair of descending thoracic aortic aneurysms in low risk patients: A multicenter comparative trialJ Thorac Cardiovasc Surg 2007 133:369-77. [Google Scholar]