Fractures of the IT region are some of the most common fractures encountered by an orthopaedic surgeon. With increase in life expectancy, the incidence of these fractures is also increasing [1]. By 2040, the incidence is expected to have doubled [2]. IT fractures account for approximately 45% to 50% of all hip fractures in the elderly [2] and out of these, 50% to 60% are classified as unstable [3]. Unstable IT fractures are those having comminution of the posteromedial buttress, exceeding a simple lesser trochanteric fragment or those with subtrochanteric extension [4]. Unstable IT fractures are a major cause of concern in the elderly due to the associated increase in morbidity and mortality [5].
The goal of treatment is restoring mobility safely and efficiently, while minimizing the risk of medical complications and technical failure. Restoration of mobility depends on the quality of bone and the type of implant used. The incidence of failure with unstable IT fractures is as high as 50% [3] and the cut out rate can be as high as 8% for hip screws [6]. Publications in the last two decades have suggested that the use of prosthetic replacement or PFN for unstable IT fractures have allowed early postoperative mobilization and prevents excessive collapse at fracture site. Patients can return to their preinjury level of activity much earlier by treatment with either of these modalities; thus, eliminating the postoperative complications caused by prolonged immobilization or implant failures [7].
The purpose of this study was to primarily compare functional recovery in patients with unstable IT fractures of femur treated with DHS or BH or PFN using Harris hip score and mobility score of Parker and Palmer. The secondary objective was to compare intraoperative and postoperative parameters of patients in all the three groups.
Materials and Methods
This was a prospective study carried out in a tertiary care setup of Medical College in Mumbai, Maharashtra, India, between July 2010 to January 2013. Approval of Institutional Ethics Committee and written informed consent was obtained from all patients. A total of 50 patients above the age of 60 years, with unstable IT fractures were included in the study and classified according to Evans Classification [8]. The type of implant for a particular patient and a particular type of fracture was randomly selected and the same surgical team treated all patients. Randomization was carried out on the basis of sealed envelopes and a total of 50 envelopes were generated. An envelope was then selected so that an appropriate operative planning could be performed. However, 50 patients were recruited which led to the discrepancy in the three groups. Patients having IT fractures with subtrochanteric extension, pathological fractures, and stable undisplaced fractures were not included in the study. Each patient was graded according to Singh’s index [9] for osteoporosis and scored for mobility prior to injury based on the mobility score of Parker and Palmer [10]. Also, the ASA physical status score [11] and the average duration between occurrence of fracture and day of surgery was noted.
All patients were operated under regional anaesthesia. A standard operative procedure was followed for all cases of DHS, BH and PFN. In cases where DHS was used, an additional derotational screw was inserted over the derotation wire under the guidance of intraoperative imaging. While in cases where BH was done where severe comminution of trochanter was found, a stainless steel wire of 20 gauge was used to hold the trochanteric fragments. In all the cases of PFN, a standard PFN of length 240 mm was used. Intraoperative parameters considered were the total duration of surgery, amount of blood loss and units of blood transfused intraoperatively and occurrence of any intraoperative complications. It was also noted if greater trochanter wiring was done or not.
Postoperatively, patients operated by DHS were made to walk non weight bearing with support from fifth or seventh postoperative day. At first follow up, at six weeks from surgery, toe-touch weight bearing was initiated. In the next follow up, after four to six weeks, patients showing both clinical and radiological signs of union were allowed to bear full weight. Patients operated with BH, were made to stand with support of a walker and allowed to walk FWB by fourth or fifth postoperative day. Patients were not allowed to squat or sit crossed legged. Patients operated with PFN were made to stand by the third or fourth postoperative day and made to walk FWB with support of a walker. Postoperative complications were treated prior to discharge. The patients were followed up every month for the first three months and then every three months for the first year and every six monthly from then onwards [Table/Fig-1,2,3,4,5,6,7,8 and 9]. Functional outcome was measured at 12 months using Harris hip score [12] and mobility score of Parker And Palmer [10].
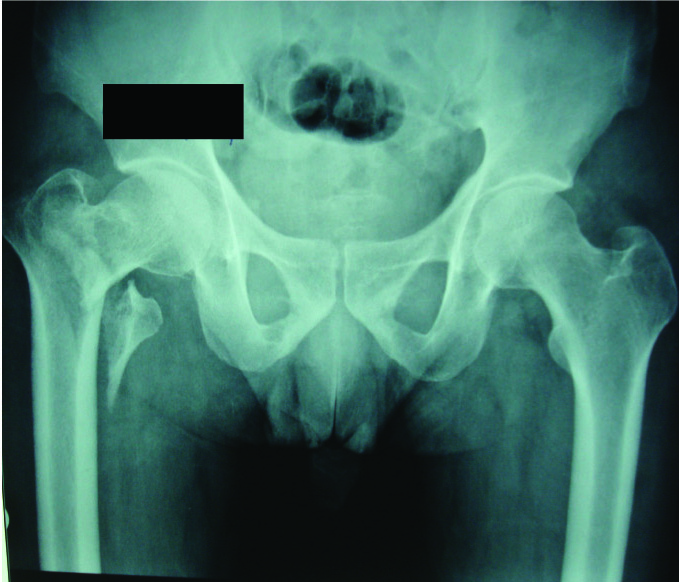
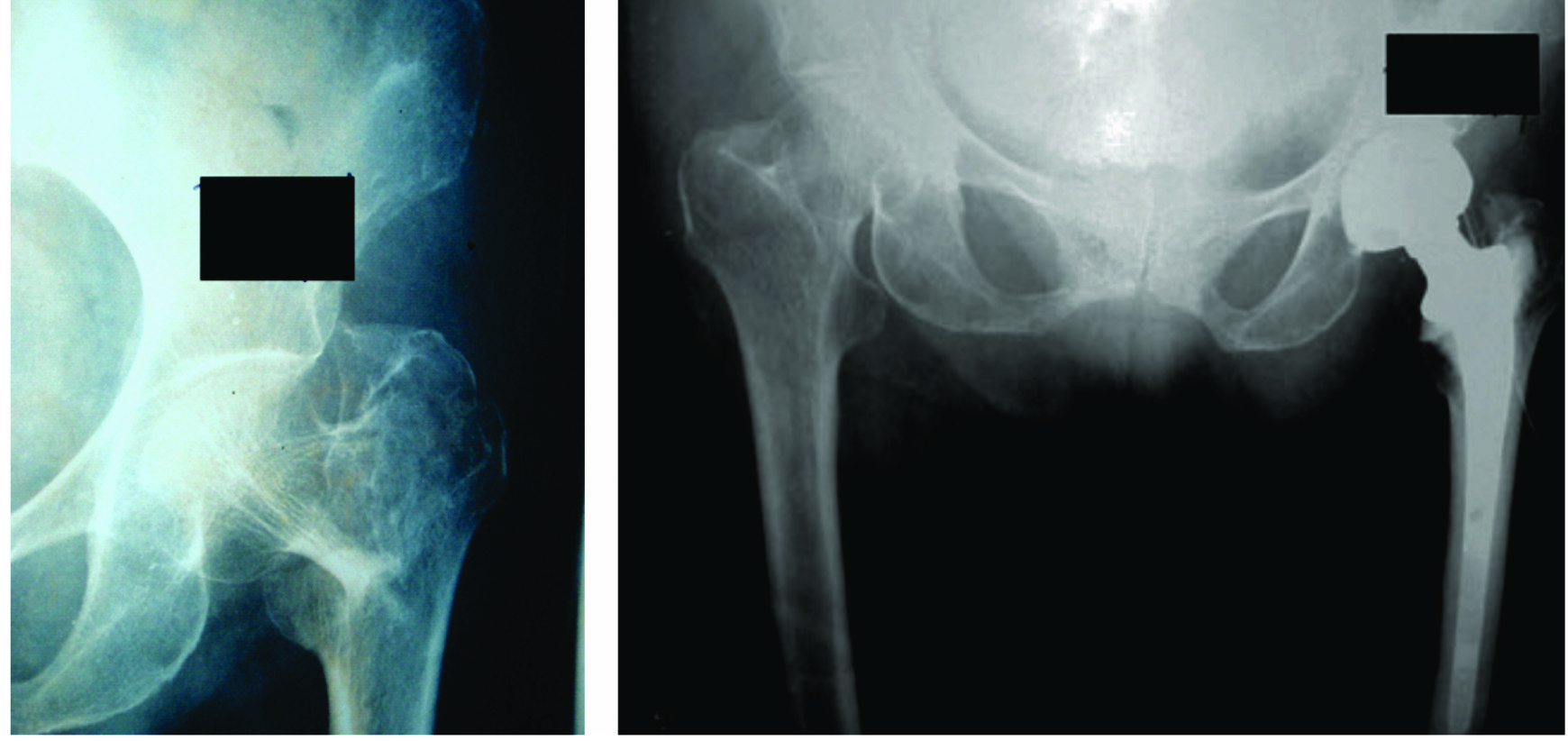
Case 1 - Preoperative X-ray (Type IV Evans fracture)
Case 1- Postoperative X-ray day 1 AP view and lateral view.
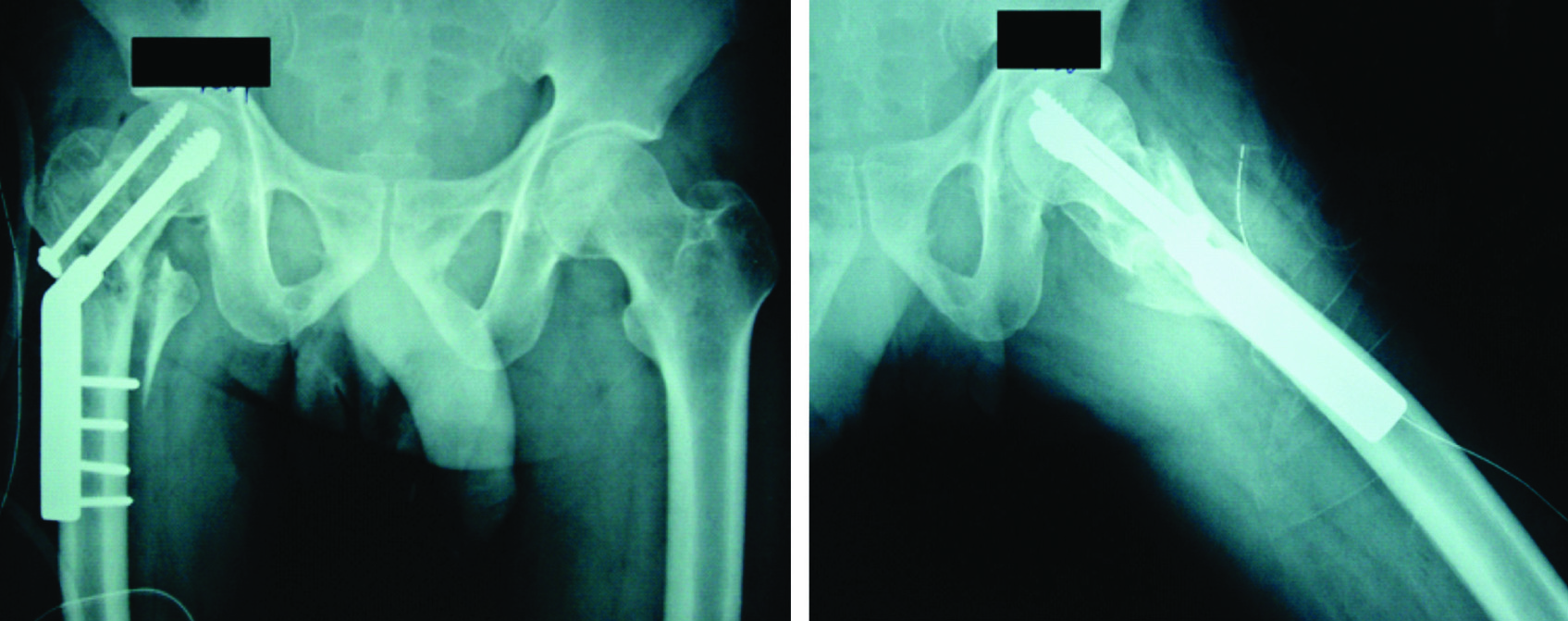
Case 1- Postoperative X-ray day 90 AP view and lateral view.
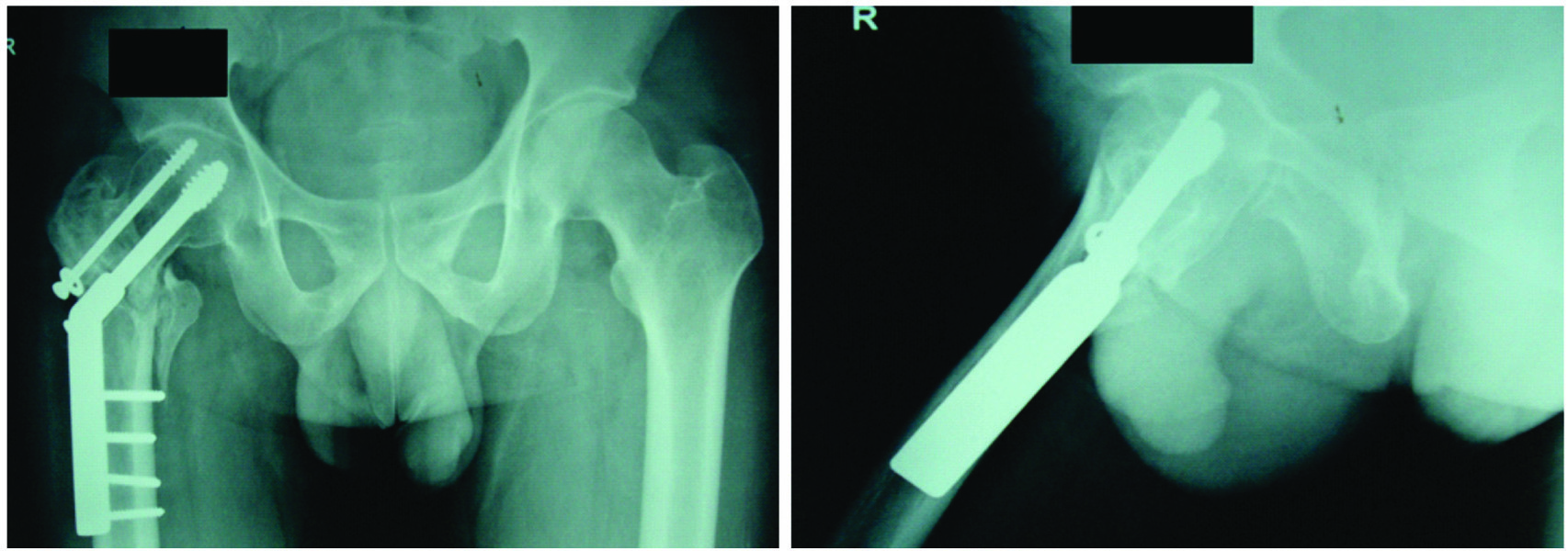
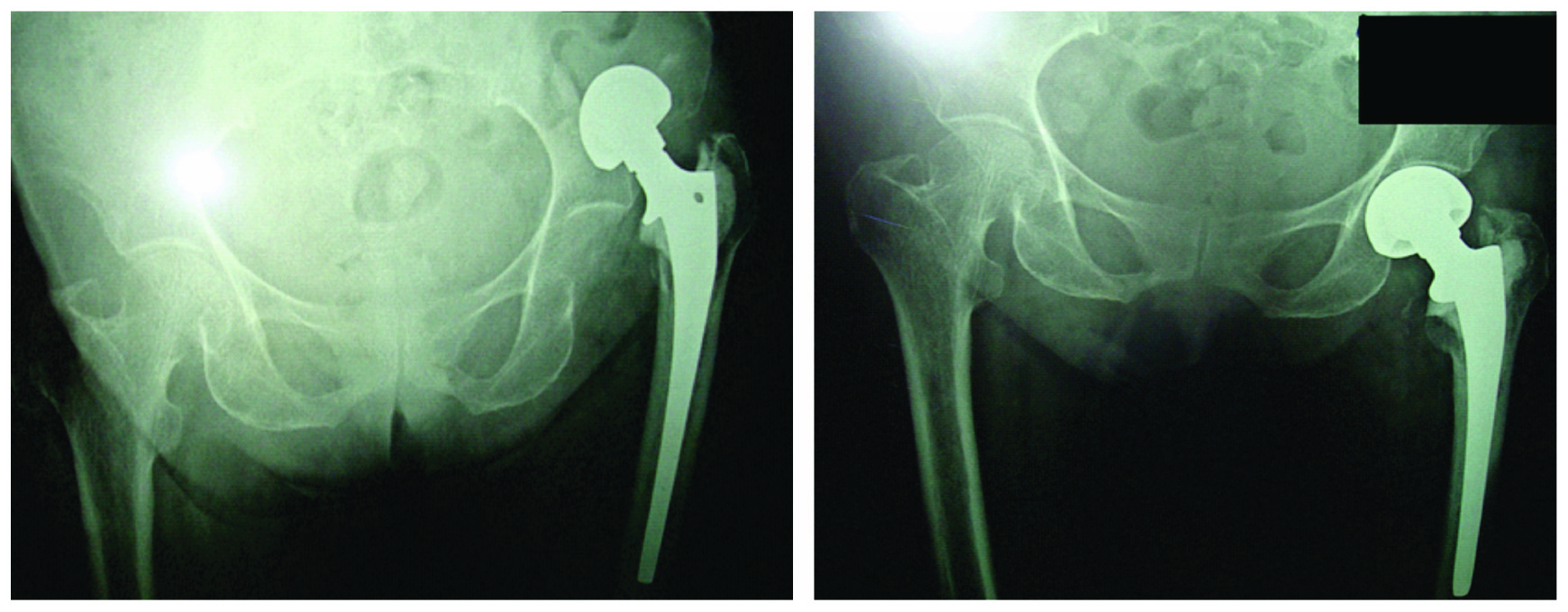
Case 2 - Preoperative X-ray (Type III Evans fracture) and postoperative X-ray.
Case 3-Preoperative X-ray (Type III Evans fracture) and postoperative X-ray.
Case 3; Complication-Dislocation; prereduction X-ray (type-IV Evans fracture).
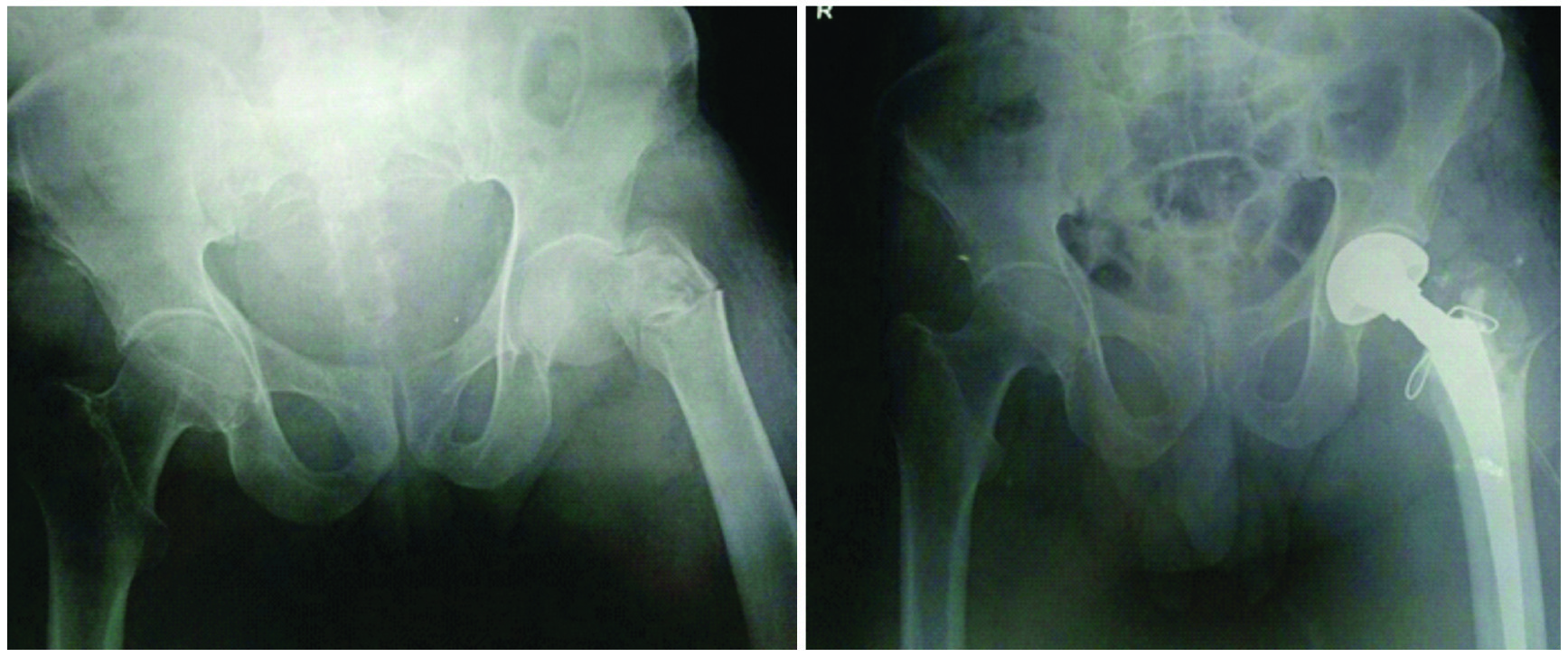
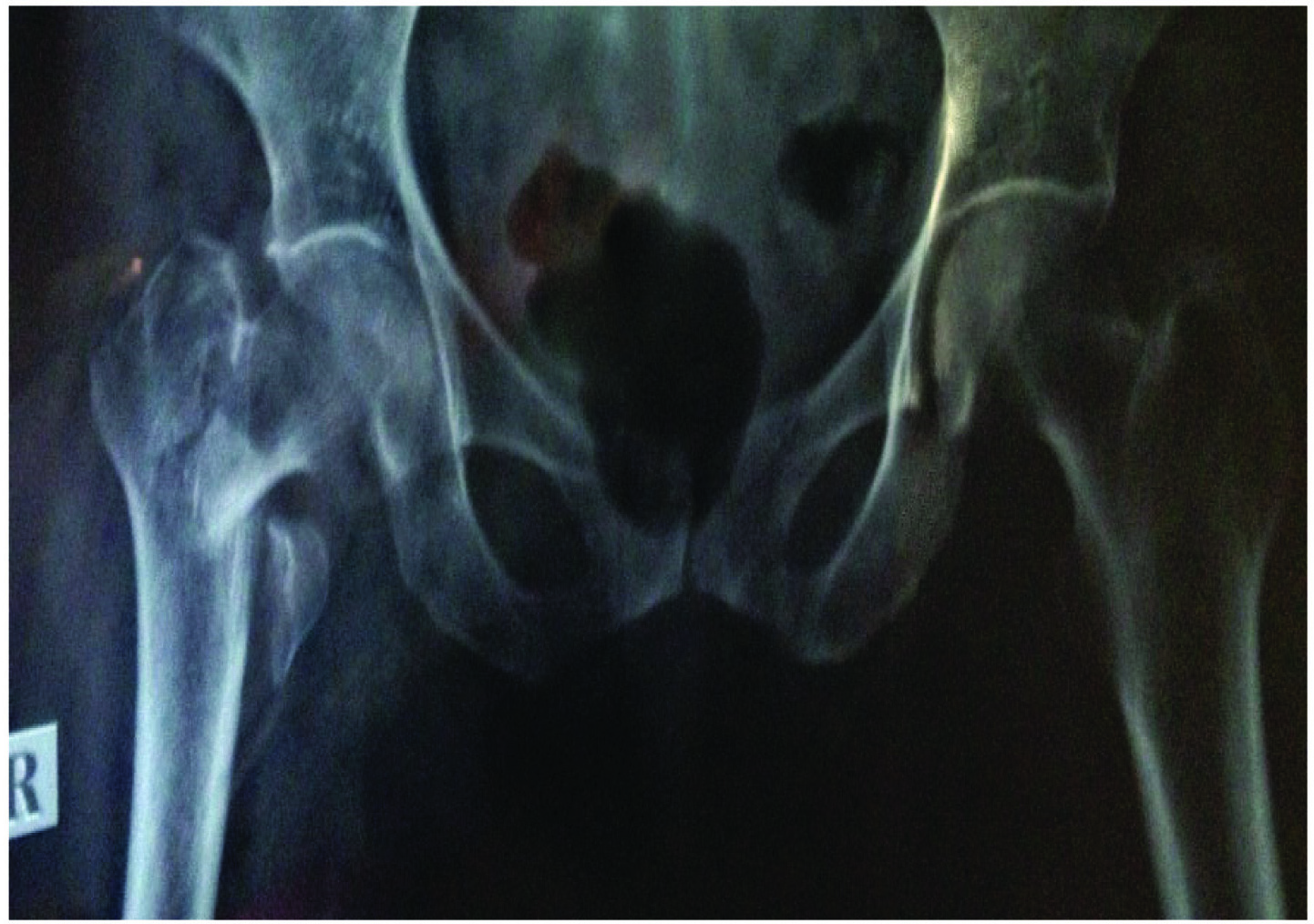
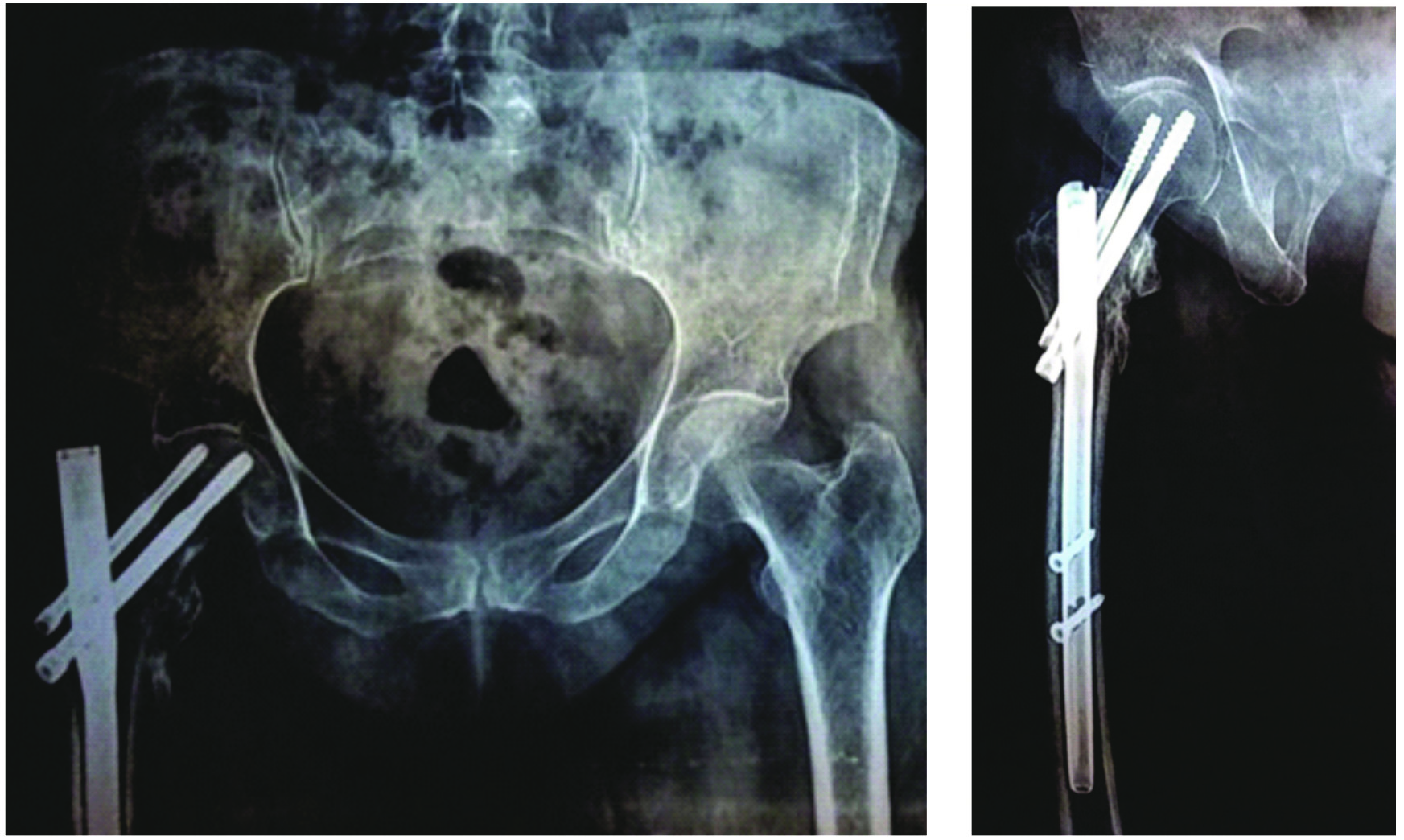
Case-4 Preoperative X-ray (Type IV Evans fracture).
Case 4 - Postoperative X-ray day 1 AP view and lateral view.
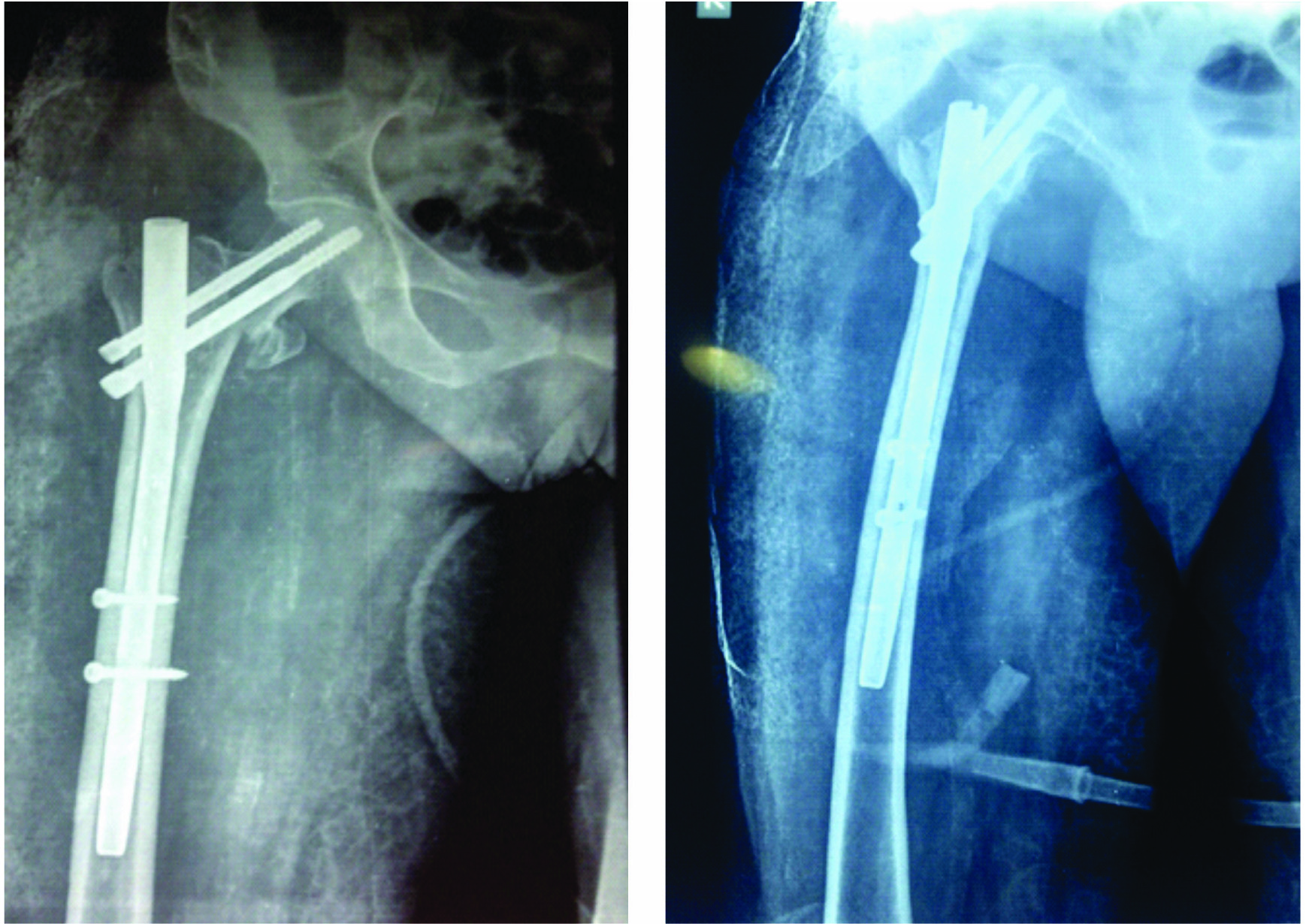
Case 4- Postoperative X-ray Day 90 AP view and lateral view.
Statistical Analysis
The data was analysed using Pearson’s Chi-Square test and One-way Analysis Of Variance (ANOVA). In order to compare multiple variables, post-hoc test was used. All complications among the three variables were analysed using Fisher’s-Exact test as the sample size was too small to apply Pearson’s Chi-Square test. A p-value < 0.05 was considered statistically significant.
Results
The study included 29 males and 21 females with a mean age of 73.03 years (61-82 years) and 77.9 years (60-92 years) respectively, and all had a fall at home.
The mean follow up for Group 1 was 19 months (12-30 months), for Group 2 was 19.3 months (12-30 months) and for Group 3 was 18.8 months (12-28 months). No patient was lost to follow up. All patients in the three groups were comparable to each other in terms of their demographics [Table/Fig-10]. The intraoperative data is depicted in [Table/Fig-11]. The mean duration of surgical time in Group 3 (86.7 minute) was much lower, in comparison to Group 1 (104.2 minute) and group 2 (106.2 minute) (p-value 0.098).
Demographic and preoperative data.
| Parameter | DHS (n=19) | Bipolar (n=13) | PFN (n=18) | p-value |
|---|
| Mean age (range) | 71.74 (61–91) | 74.38 (61–92) | 74 (60–92) | 0.947+ |
| Sex - M:F | 12:7 | 5:8 | 12:6 | 0.247+ |
| Side–right: left | 10:9 | 8:5 | 10:8 | 0.882+ |
| Type of injury |
| Low velocity:High velocity | 19:0 | 13:0 | 18:0 | _ |
| Fracture type (Evans Classification) |
| III | 7(36.8 %) | 3 (23.1%) | 8 (44.4%) | 0.742+ |
| IV | 8 (42.1%) | 7 (53.6%) | 8 (44.4%) |
| V | 4 (21.1%) | 3 (23.1%) | 2 (11.1%) |
| Singhs index |
| V | 1 (5.3%) | 0 | 1(5.6%) | 0.791+ |
| IV | 4 (21.1%) | 1 (7.7%) | 3 (16.7%) |
| III | 7 (36.8%) | 6 (46.2%) | 8 (44.4%) |
| II | 7 (36.8%) | 5 (38.5%) | 6(33.3%) |
| I | 0 | 1 (7.7%) | 0 |
| ASA Grading |
| 1 | 7 | 3 | 7 | 0.889+ |
| 2 | 6 | 6 | 5 |
| 3 | 6 | 4 | 6 |
| Mean±S.D | 1.95±0.85 | 2.08±0.76 | 1.94±0.87 | |
| Pre op Mobilty Score of Parker and Palmer±S.D* | 7.3±1.7 | 7±1.76 | 7.6±1.5 | 0.489+ |
| Trauma-surgery interval+S.D | 2.95±1.93 | 2.69±1.32 | 3.0±1.68 | 0.873+ |
*The data included is of patients who were available at 12 months.
+ = not significant; One-way Analysis of Variance (ANOVA) was the statistical test done to compare the data.
| Parameter | DHS (n=19) | Bipolar (n=13) | PFN (n=18) | p-value |
|---|
| Mean intraoperative time (minutes) ± S.D | 104.2±33.72 | 106.2±26.31 | 86.7±22.7 | 0.098 + |
| Mean blood loss (ml) ±S.D | 484.2±183.4 | 573±152.2 | 252±146.0 | ≥0.001 # |
| Mean blood transfusion units±S.D | 1.27±0.47 | 1.6±0.52 | 1.14±0.38 | 0.124 + |
| Mean hospitalization time (days) ±S.D | 17.5±3.24 | 18.27±4.43 | 17.72±4.14 | 0.873 + |
+ = not significant, # = significant (p<0.05); One-way Analysis of Variance (ANOVA) was the statistical test done to compare the data.
There were no intraoperative complications observed. One female patient developed septicaemia in Group 1 and expired on the fifth postoperative day. Two female patients expired due to pulmonary embolism on the second postoperative day in Group 2. Two patients in Group 2 suffered hip dislocation, one at eighth week spontaneously and the second at 12th week during an attempt to squat. Both were closed reduced. However, the second patient expired while hospitalized due to associated comorbid conditions. Patients with early postoperative complications [Table/Fig-12] were treated appropriately prior to discharge. One patient followed up at 12th week in Group 3 with proximal screw migration. He initially refused any further treatment and on on subsequent follow up, had developed Avascular Necrosis (AVN) of femoral head. He was revised with a Total Hip Replacement (THR) surgery [13]. Another patient in Group 3 followed directly at 22nd week from the date of discharge with screw migration and AVN of femoral head and was revised with a THR surgery. Two patients in Group 3 expired in the fourth and fifth postoperative month due to associated comorbid conditions.
| Complications | DHS (n = 19) | Bipolar (n = 13) | PFN (n = 18) | p-value (comparison between DHS and Bipolar) | p-value (comparison between DHS and PFN) | p-value (comparison between Bipolar and PFN) |
|---|
| A) EARLY |
| 1. Bed sore | 3 (15.7%) | 1 (7.6%) | 0 | 0.629+ | 0.230+ | 0.419+ |
| 2. UTI | 2 (10.5%) | 1 (7.6%) | 2 (11.1%) | 1.000+ | 1.000+ | 1.000+ |
| 3. Thrombophlebitis | 3 (15.7%) | 1 (7.6%) | 2 (11.1%) | 0.629+ | 1.000+ | 1.000+ |
| 4. Superficial infection | 2 (10.5%) | 0 | 2 (11.1%) | 0.502+ | 1.000+ | 0.497+ |
| 5. Pulmonary embolism | 0 | 2 (15.3%) | 0 | 0.157+ | - | 0.168+ |
| 6. Septicaemia | 1 (5.2%) | 0 | 0 | 1.000+ | 1.000+ | - |
| 7. Deep infection | 0 | 0 | 1 (5.5%) | - | 0.486+ | 1.000+ |
| B) LATE * |
| 1. Hip dislocation | 0 | 2 (18.2%) | 0 | 0.157± | - | 0.168+ |
| 2. Femoral head AVN | 0 | 0 | 2 (12.5%) | - | 0.230+ | 0.497+ |
| 3. Implant cut out | 0 | 0 | 2 (12.5%) | - | 0.230+ | 0.497+ |
| C) MORTALITY (at 12 months) | 1 (5.3%) | 3 (23.1%) | 2 (11.1%) | 0.279+ | 0.604+ | 0.625+ |
| D) REOPERATION (at 12 months) | 0 | 0 | 2 (12.5%) | - | 0.230+ | 0.497+ |
*Late complications were considered after the death of four patients.
+ = not singnificant; Fisher’s-Exact test was used to compare complications as the sample size was too small in individual groups.
The time to FWB [Table/Fig-13] was earlier (p-value>0.001) in Group 2 and Group 3 as compared to Group 1. No significant difference (p-value=0.959) was observed in the mean postoperative mobility score amongst the three groups at the end of 12 months. The Harris hip score at the end of 12 months was excellent for 16 patients, good for 18 patients, fair for five patients and poor for five patients (p-value=0.960). At the end of the study, 34 patients were able to do their daily activities and 10 were unable to do so.
| DHS (n = 19) | Bipolar (n = 13) | PFN (n = 18) | p-value |
|---|
| 1. Walks unaided FWB(weeks) ± S.D | 8.62 ± 0.65 | 6.29 ± 0.76 | 6.17 ± 0.72 | >0.001# |
| 2. Pain (at 12 months) (%) | | | | 0.860+ |
| No | 11 (61.1%) | 5 (50%) | 9 (56.3%) | |
| Slight | 5 (27.8%) | 4 (40%) | 3 (18.8%) | |
| Mild | 1 (5.6%) | 1 (10%) | 2 (12.5%) | |
| Moderate | 1 (5.6%) | 0 | 1(6.3%) | |
| Severe | 0 | 0 | 1 (6.3%) | |
| 3. Mean shortening (cm)(at 12 months) ± S.D | 0.84 ± 1.03 | 0.95 ± 1.12 | 0.69 ± 0.68 | 0.774+ |
| 4. Time to union(weeks) ± S.D | 15.67 ± 2.77 | N.A | 14.71 ± 2.79 | 0.343+ |
| 5. Able to do daily activities | | | | 0.696+ |
| Yes (%) | 15 (83.3%) | 7 (70%) | 12 (75%) | |
| No (%) | 3 (16.7%) | 3 (30%) | 4 (25%) | |
| 6. Post op mobility score of Parker and Palmer. (at 12 months) ± S.D | 6.78 ± 2.3 | 6.5 ± 2.2 | 6.75 ± 2.3 | 0.959+ |
| 7. Harris hip score (at 12 months) (%) | | | | 0.960+ |
| Excellent | 7 (38.9%) | 3 (30%) | 6 (37.5%) | |
| Good | 8 (44%) | 4 (40%) | 6 (37.5%) | |
| Fair | 1 (5.6%) | 2 (20%) | 2 (12.5%) | |
| Poor | 2 (11.1%) | 1 (10%) | 2 (12.5%) | |
| 8. Patients who regained their preoperative ability. | 11 (61%) | 6 (60%) | 9 (56%) | 0.957+ |
+ = not significant and # = significant (p<0.05); Pearson Chi-Square test and One-way Analysis Of Variance (ANOVA) were used to assess data.
Discussion
Our study included 50 patients randomized for the three modalities and were followed up for an average of 19 months (12-30 months), with the total duration of the study being 30 months. Total number of 19 patients were operated by DHS, 13 by BH and 18 by PFN.
We found that the mean blood loss during PFN surgery (Group 3) {252 ml (100 – 600)} was significantly lower (p-value>0.001) than the mean blood loss in the other two groups.
The time to FWB in weeks was significantly higher (p-value>0.001) in the DHS Group as compared to patients in the other two groups [Table/Fig-13]. This is because PFN surgeries in the present study were performed closed except in one patient, where open reduction was performed.
The mean duration of surgery in the DHS (104 minute) and BH Groups (106 minute) was much more than that in the PFN Group (86.7 minute) but not significant (p-value 0.098). Mortality in the BH Group {3(23%) patients} was much higher when compared to the other two groups, though was not significant [Table/Fig-12]. Two patients died in the immediate postoperative period due to pulmonary embolism and one died of associated comorbid conditions. This trend of increased mortality in the BH Group was also noted in other studies as shown in [Table/Fig-14] [6,14-17]. At the end of 12 months, 16 (36.4%) patients had excellent (seven in DHS Group, three in BH Group and six in PFN Group), 18 (40.9%) patients had good (eight in DHS Group, four in BH Group and six in PFN Group), 5 (11.4%) had fair (one in DHS Group and two each in BH and PFN Group), and 5 (11.4%) had poor (two each in DHS and PFN Group and one in BH Group) Harris hip score (p-value=0.960) [12].
Comparison of mortality with other studies [6,14-17].
| Our study | Haentjens P et al., [6] | Kesmezacar H et al., [14] | Kayali C et al., [15] | Park SY et al., [16] | Schipper IB et al., [17] |
|---|
| DHS | N = 19 | N = 42 | N = 38 | N = 45 | N.A | N.A |
| Mortality | 1 (5.3%) | 10 (24%) | 13 (34%) | 7 (16%) | | |
| Complications |
| a) Bed sore | 3 (15.7%) | 8 (19%) | 3 (8%) | 5 (11.4%) | | |
| b) Superficial infection | 2 (10.5%) | 0 | 1 (2.6%) | 1 (2.8%) | | |
| c) Implant cut out | 0 | 6 (14%) | 1 (2.6%) | 6 (13.7%) | | |
| BH | N = 13 | N = 37 | N = 43 | N = 42 | N.A | N.A |
| Mortality | 3 (23%) | 11 (30%) | 21 (49%) | 10 (24%) | | |
| Complications |
| a) Bed sore | 1 (7.6%) | 1 (3%) | 0 | 4 (9.6%) | | |
| b) Pulmonary embolism | 2 (15.3%) | 0 | 4 (9.3%) | 0 | | |
| c) Hip dislocation | 2 (18.5%) | 2 (5%) | 1 (2.3%) | 0 | | |
| PFN | N = 18 | N.A | N.A | N.A | N = 25 | N = 211 |
| Mortality | 2 (11.1%) | | | | 0 | 46 (24.5%) |
| Complications |
| a) Superficial infection | 2 (11%) | | | | 0 | 8 (4%) |
| b) Implant cut out | 2 (11%) | | | | 4 (16%) | 11 (7%) |
| c) Fracture at nail tip | 0 | | | | 0 | 4 (2%) |
N.A = Data is not applicable for that study.
In the study conducted by Haentjens P et al., the mean blood loss in DHS Group was 780 ml and in the BH Group was 680 ml with the duration of surgery being 82 minutes and 102 minutes respectively [6]. Whereas, in the study conducted by Pajarinen J et al., the mean blood loss in the DHS Group was 357 ml and in the PFN Group was 320 ml [18]; the mean duration of surgery being 45 minutes and 55 minutes respectively. Patil SS and Panghate A in their study showed that the mean blood loss in the DHS Group was 450 ml and in the BH Group was 420 ml with the mean duration of surgery being 102 minutes and 110 minutes respectively [19]. While Xu YZ et al., in their study showed that the blood loss was significantly lower in the Proximal Femoral Nail Antirotation Device (PFNA) group than in the DHS Group while the surgical time was significantly higher in the PFNA Group as compared to the DHS Group [20]. This was attributed probably due to the longer learning curves associated with PFNA.
In patients with osteoporotic fractures, maintenance of reduction can be a major problem during the healing period. To reduce the healing time, dynamic devices are replaced with more static ones. Biomechanical studies show that dynamic implants have more weight bearing capacity than static implants. Furthermore, partial weight bearing creates a micromovement in the dynamic systems, which increases the union rate. However, cut out is the main complication of internal fixation. Central positioning of the screw in the femoral neck has been recommended, which yields cut out rate of about 13%. The strength of fixation depends on screw positioning and bone quality [19]. In the present study, no cases of cut out were noted in the DHS Group whereas in 2 (12.5%) patients of PFN Group, proximal migration was noted which was found to be insignificant (p-value=0.242). These two patients were subsequently treated with THR surgery [13]. In the study conducted by Pajarinen J et al., two patients each in the DHS and PFN Groups had an implant failure, which were subsequently revised [18]. Six patients each in the study conducted by Haentjens P et al., and Kayali C et al., and four patients in Patil SS and Panghate A, seven patients in the study conducted by Kim et al., study had cut out in the DHS group [6,15,19,21]. Whereas in the studies conducted by Park SY et al., and Schipper IB et al., there were 11 and four patients respectively with PFN cut-outs [16,17]. In the study by Xu YZ et al., there were three cases of fixation failure (two in the PFNA Group and one in the DHS Group) were noted; though not statistically significant [20].
Wang CJ et al., in their experimental study of comparing the efficacy of a single against two femoral neck screws in an intramedullary nail concluded that the two lag screw configuration should be avoided in patients who have a high risk of osteoporotic cut out [22]. Their recommendation for IT fractures in elderly patients with poor bone quality was the single screw design. Fracture at the femoral diaphysis at the tip of the nail is a known complication associated with the use of intramedullary nails in the treatment of proximal femoral fracture. There were none seen in this study. However, the follow up period of this study was relatively short.
In this study, two patients followed up with hip dislocation, which was closed reduced, one patient subsequently expired during hospitalization due to associated comorbid conditions. Two patients in the study conducted by Haentjens P et al., and one in the study conducted by Kesmezacar H et al., followed with hip dislocation [6,14]. They were also closed reduced. There were no cases of hip dislocation in the study conducted by Kayali C et al., Patil SS et al., and by Abdelkhalek M et al., [15,19,23].
Early mobilization is well known with BH and PFN and that is what was followed in this study. In the current study, patients operated by DHS were made to start non weight bearing as early as fifth to seventh postoperative day and at six weeks of follow up, when some signs of radiological union were seen; they were allowed partial weight bearing with a walking aid. If at next follow up, healing process continued and no complications were noted, patients were allowed to bear full weight on the affected limb. This is why the average weeks to FWB was higher in the DHS Group as compared to the other groups. This also served as an advantage and hence, there was no implant cut out in the DHS Group. In the study by Xu YZ et al., the mean time to mobilization with a frame was significantly shorter in the PFNA group than in the DHS Group [20]. While Kayali C et al., in their study showed that time to FWB was significantly earlier in the hemiarthroplasty group as compared to the DHS Group [15].
Parker MJ and Handoll HH compared extramedullary to intramedullary devices in a meta-analysis of more than 3500 patients and found the sliding hip screw devices superior to intramedullary devices for treatment of extracapsular hip fractures in adults [24]. The literature within the last decade has demonstrated a change of practice in the treatment of IT fractures, with a dramatic increase in the number of intramedullary devices being used. The increase has not been backed up by scientific evidence but has been driven by other factors, including marketing by industry, surgeon preference, and reimbursement [25]. The trend towards more frequent intramedullary fixation rate of IT fractures in medicare patients across the United States have been reported recently, but it cannot be explained by patient related factors [26]. In a study of candidates taking the Part II American Board of Orthopedic Surgery examination, the intramedullary fixation rate for IT fractures increased from 3% to 67% between 1999 to 2006 [27]. This increase occurred without a significant improvement in terms of functional outcome or patient satisfaction in comparison with the sliding hip screw.
Saudan M et al., found that even though the mean pre and postoperative scores of function and mobility did not differ significantly between the DHS and PFN treatment Groups; the score for mobility was decreased more in the patients treated with PFN [28]. In contrast, patients treated by PFN in the study by Pajarinen J et al., regained their preoperative walking ability at four months significantly more often than those treated with a DHS [18]. However, in the current study, no significant difference (p-value= 0.957) in the ability of patients to regain their preoperative walking ability in any of the three groups was noted.
Although, it is a common opinion that both arthroplasty and PFN allow early mobilization, in the current study it was found that early mobilization was also related to the patient’s general health condition. No significant difference was found in the three groups in terms of postoperative mobility score of Parker and Palmer [10] and the Harris hip score [12]. It was also observed that, decreased quality of life and probable complications were due to systemic problems, which were commonly seen in this age group.
Even though, the mean blood loss and the mean time to FWB walking were significantly higher in the DHS Group, the functional results were objectively better in the DHS Group as compared to the other two groups.
Limitation
The limitation of this study was that, the sample size was not large enough and the follow up period was short. There is no study about mid or long term results of the hemiarthroplasty and proximal femoral nailing procedure in literature. We recommend a study that evaluates long term results of cemented BH and PFN in unstable IT fractures.
Conclusion
At early follow up, no significant advantage of the PFN and the BH to the DHS procedure was found. We recommend when the DHS procedure is used as a treatment modality, early non weight bearing with regular follow up for clinical and radiological assessment for subsequent complications/partial/FWB. Also, when a cemented arthroplasty is chosen as the treatment modality, we recommend retaining of the posteromedial fragment and greater trochanteric tension band wiring. Treatment of unstable IT fracture of femur is a matter open to debate. IT fractures of elderly must be treated with considering the age of the patient, mental status, bone quality, and the type of fracture. It is certain that the main objective is to prevent the possible complications by early mobilization and to help the patient to return to their daily life.
*The data included is of patients who were available at 12 months.
+ = not significant; One-way Analysis of Variance (ANOVA) was the statistical test done to compare the data.
+ = not significant, # = significant (p<0.05); One-way Analysis of Variance (ANOVA) was the statistical test done to compare the data.
*Late complications were considered after the death of four patients.
+ = not singnificant; Fisher’s-Exact test was used to compare complications as the sample size was too small in individual groups.
+ = not significant and # = significant (p<0.05); Pearson Chi-Square test and One-way Analysis Of Variance (ANOVA) were used to assess data.
N.A = Data is not applicable for that study.