Gallstone disease is one of the most common gastrointestinal conditions that we come across in our surgical practice. The occurrence of hepatocellular damage in patients with gallstone disease has been the subject of debate for many years [1]. Evidence has presented that structural and functional changes of liver were observed in patients of cholangitis due to any cause which leads to partial extra-hepatic large bile duct obstruction [2,3]. These changes may subside by removal of the obstruction, which restores flow of bile within the biliary ductal system and resolution of the inflammatory process. This suggests a direct relationship between the degree of inflammation in the liver and obstruction in biliary tree [3]. Previous studies reported minor degree of fibrosis in portal tracts, but the presence of cholestasis were not emphasized and correlating the presence of gall stones with changes in liver histology had given conflicting results [2,3]. Therefore, this study was taken up to determine the liver changes associated with gallstone disease in detail and correlate these findings with position of gallstone in biliary tree.
Materials and Methods
This cross-sectional study was conducted on 60 patients who were admitted with clinical signs and symptoms of gallstone disease and underwent operative procedure in the Department of Surgery, Regional Institute of Medical Sciences, Imphal, Manipur, India from October 2013 to September 2015. The sample size was calculated using n= (z/m)2 P(1-P) where m is the standard error=5%, z is 1.28 for a precision level of 95% and 5% allowable error, P is 19% (proportion of post cholecystectomy individuals having chronic inflammatory changes in liver by George RK et al., [3]).
Inclusion Criteria
All patients presenting with signs and symptoms of gallstone diseases and diagnosed for the same with the help of imaging modality.
Exclusion Criteria
Patients with alcoholic liver disease, known cirrhotic patients, viral hepatitis, carcinoma of biliary tree and where there arose any contraindications to the intervention i.e., liver biopsy, like congenital coagulopathy, thrombocytopenia, raised prothrombin time.
Approval of the Institutional Ethical Committee and informed consent was taken from all the participants.
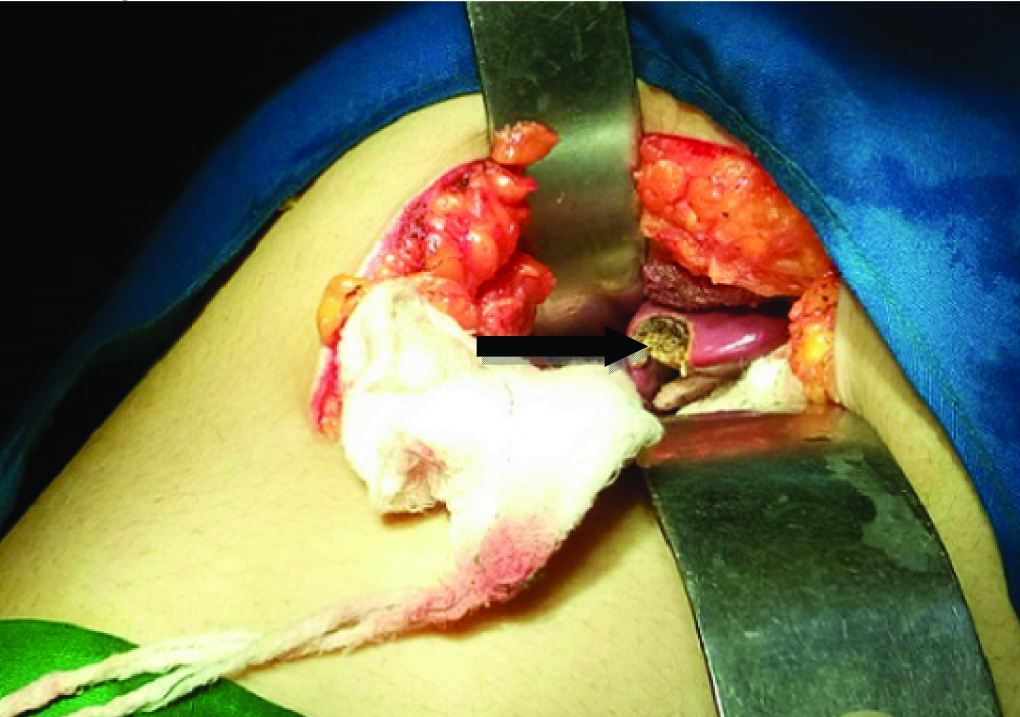
All patients were evaluated with biliary scan (USG and or MRCP) as required. LFT was done preoperatively and one month postoperatively on follow up. Liver biopsy (>0.8 cm) taken intraoperatively immediately after laparotomy before proceeding with definitive surgery [Table/Fig-1]. Histopathological examination was done by a pathologist, blinded to the clinical findings.
Intraoperative picture of liver showing biopsy region.
Statistical Analysis
The result of the study was interpreted using IBM SPSS software version 20.0 (SPSS, Inc., Chicago, IL). Categorical variables were analysed using a chi-square test. A p-value <0.05 was taken as significant.
Results
Patient’s age ranged from 26 to 60 years with a mean age of 43.3 years. The maximum number of patients was in the age group 41-50 years (38.3%). The majority of patients were females 47 (78.33%). The male to female ratio was 1:4.6. Out of 60 patients, 44 (73.33%) had cholelithiasis and 16 (26.6%) had choledocholithiasis.
LFT and Gallstone Disease
Out of the 44 patients of cholelithiasis, 8 of them had elevated LFT, in which 6 (13.6%) had raised alkaline phosphatase >290 IU, 4 (9.1%) had raised total bilirubin level and 2 (4.54%) had raised Alanine transferase >40 U. Out of the 16 choledocholithiasis patients, 14 had elevated LFT, in which 8 (50%) had raised total bilirubin level, 8 (50%) had raised alkaline phosphatase >290 IU, 6 (37.5%) had raised alanine transferase >40 U and gamma-glutamyl transferase >50 U [Table/Fig-2].
LFT changes in gallstone disease.
| LFT* | Cholelithiasis | Choledocholithiasis |
|---|
| Total bilirubin > 1 mg/dl | 4 (9.1%) | 8 (50%) |
| Alkaline phosphatase >290 IU | 6 (13.6%) | 8 (50%) |
| Alanine transferase >40 U | 2 (4.54%) | 6 (37.5%) |
| GGT>50 U | 0 | 6 (37.5%) |
*LFT in few patients more than one parameter was increased.
LFT-Liver function test, GGT- Gamma-glutamyl transferase
Elevated LFT had a significant correlation (p<0.001) in patients of choledocholithiasis compared to cholelithisis [Table/Fig-3]. Postoperative LFT following one month of operation were normal in all the patients.
Correlation of elevated LFT in patients with cholelithiasis and choledocholithiasis.
| STONE | LFT | p-value* |
|---|
| Normal | Elevated |
|---|
| Cholelithiasis | 36 | 8 | <0.001 |
| Choledocholithiasis | 2 | 14 |
*Chi-square test, LFT-Liver function test
Liver Histology and Gallstone Disease
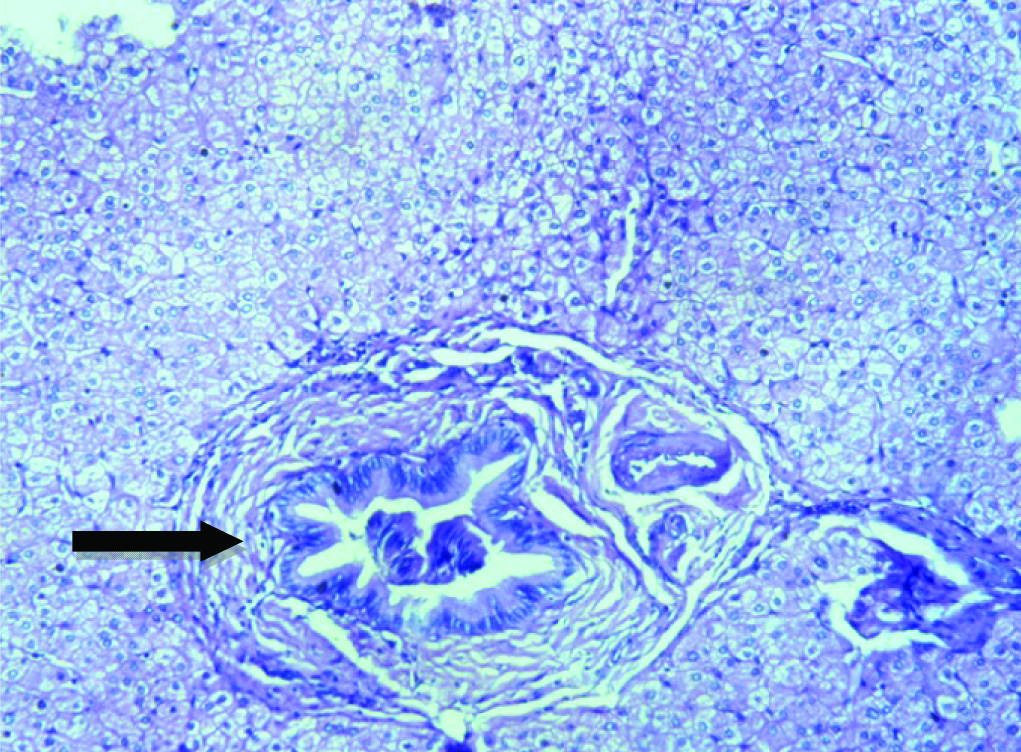
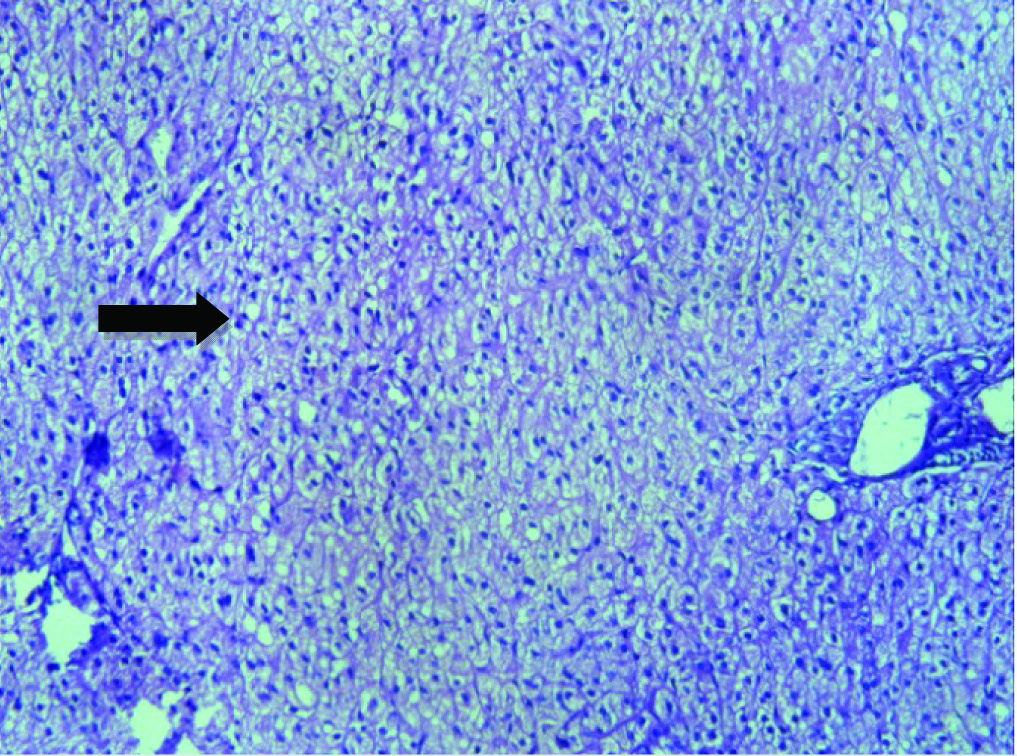
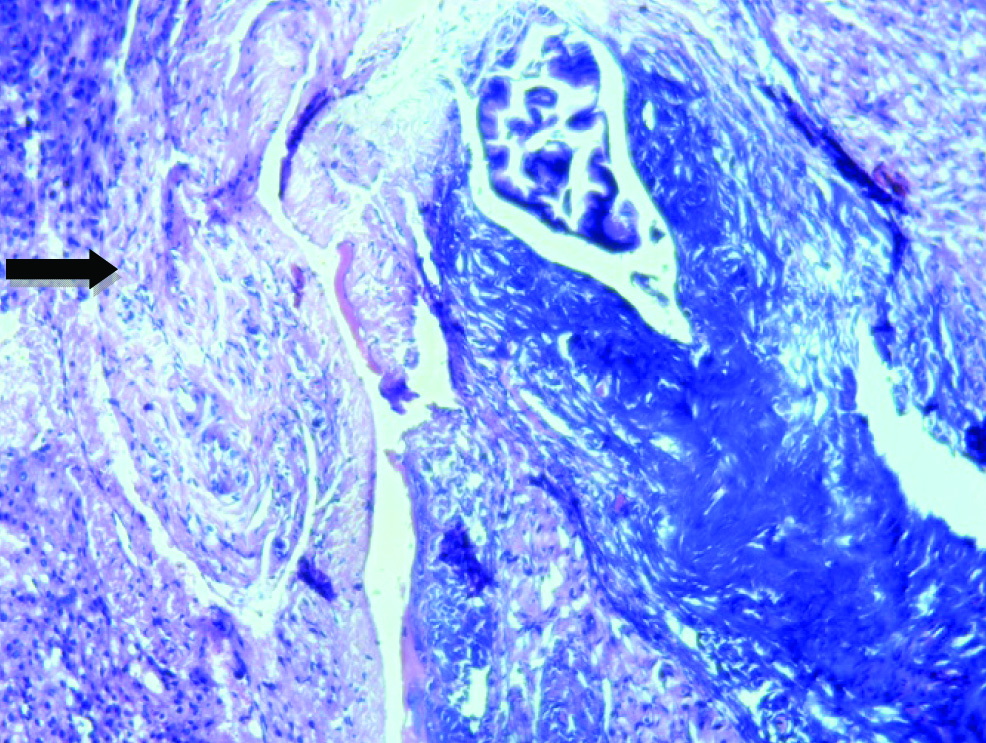
Out of the 44 patients of cholelithiasis, liver histology [Table/Fig-4] showed normal study in 12 (27.35%), non specific reactive hepatitis in 22 (46.9%), fatty metamorphosis in 6 (13.7%) and 4 (9.1%) patients had acute cholestasis. In choledocholithiasis patients, 8 (50%) showed chronic cholestasis [Table/Fig-5], 4 (25%) showed acute cholestasis [Table/Fig-6] and another 4 (25%) showed sclerosing cholangitis [Table/Fig-7]. Histopathological changes of liver has significant correlation (p<0.001) in patients of choledocholithiasis compared to cholelithiasis [Table/Fig-8].
Histopathology (HPE) changes in gallstone disease.
| HPE | Cholelithiasis | Choledocholithiasis |
|---|
| Normal study | 12 (27.35%) | 0 |
| Non specific reactive hepatitis | 22 (46.9%) | 0 |
| Fatty metamorphosis | 6 (13.7%) | 0 |
| Acute cholestasis | 4 (9.1%) | 4 (25%) |
| Chronic cholestasis | 0 | 8 (50%) |
| Sclerosing cholangitis | 0 | 4 (25%) |
| Secondary biliary cirrhosis | 0 | 0 |
| Total | 44 (73.33%) | 16 (26.7%) |
HPE of liver showing abundant lymphocyte both intraepithelial and intraluminal suggestive of chronic cholestasis (H&E stain, 40X).
HPE of liver showing abundant polymorph nuclear cells suggestive of acute cholestasis (H&E stain, 40X).
HPE of liver showing infiltration by mononuclear cells together with mild portal tract fibrosis suggestive of sclerosing cholangitis (H&E stain, 40X).
Correlation of histopathology changes of liver in patients with cholelithiasis and choledocholithiasis.
| STONE | Histopathology | p-value* |
|---|
| Normal | Abnormal |
|---|
| Cholelithiasis | 40 | 4 | <0.001 |
| Choledocholithiasis | 0 | 16 |
*Chi-square test.
Discussion
The study was designed to provide information on liver changes and severity of liver damage in patients of gallstone disease and to study their correlation with the site of biliary calculus. The age of the patients in this study ranged from 26 to 60 years. The maximum numbers of patients are in age group 41-50 years (38.33%) similar to Mohan H et al., [4]. A study in Taiwan confirmed that increasing age had a direct relationship with the development of gallstones simply due to the long-term exposure to other risk factors irrespective of locality or standard of living [5].
LFT in Gallstone Disease
LFT has been used as a routine preoperative evaluation for gallbladder surgery as a tool to check for functional status of the liver. In our study, out of 44 patients of cholelithiasis, raised alkaline phosphatase >290 IU was seen in 6 (13.6%) patients, raised total bilirubin level > 1 mg/dl seen in 4 (9.1%) patients, which was similar to study done by Habib L et al., [6]. Out of the 16 patients of choledocholithiasis, 8 (50%) patients had raised total bilirubin level, 8 (50%) patients had raised alkaline phosphatase >290 IU, 6 (37.5%) patients had raised alanine transferase >40 U and gamma-glutamyl transferase >50 U each [Table/Fig-2]. In our study, the serum alkaline phosphatase was significantly elevated in 50% of patients with choledocholithiasis. This correlated with a study done by Thapa PB et al., [7]. He stated that, the serum level of alkaline phosphatase was raised in patients with choledocholithiasis by 1.69±0.118 fold with significant statistical difference. However, alkaline phosphatase is a non-specific indicator of cholestatic liver disease because of its multiple sources like bone, placenta besides its production from the biliary canalicular membrane. In study done by Yang MH et al., gamma glutamyl transferase, alkaline phosphatase, and total bilirubin were independent predictors of liver damage and gammaglutamyl transferase appeared to be the most powerful predictor (odds ratio 3.20) [8].
Abnormal LFT due to hepatocellular injury in patients with gallstone disease is usually attributed to injury related to CBD stones. Higher biliary tree pressures can lead to impaired bile secretion, retention of bile acids and consequent apoptosis or necrosis of hepatocytes. In our study, patients with choledocholithiasis had significantly raised liver function compared to patient with cholelithiasis (p=0.001) [Table/Fig-3]. Even though insignificant, 18% of cholelithiasis patients had mild raise in LFT. However, the exact mechanism of hepatocellular damage in cholelithiasis without choledocholithiasis is not fully understood. Presumably such patients have normal biliary pressure. Free radical reactions in the human gall bladder have been demonstrated to occur in chronic cholecystitis with cholelithiasis, suggesting that oxidative stress may partially account for liver injury. It is also postulated that inflammation in the gallbladder induces inflammation in the closely apposed neighbouring liver tissue [9]. This hepatocellular injury in cholelithiasis patients appeared to be a transient, reactive phenomenon secondary to previous attack of cholecystitis associated with cholelithiasis. In our study, post operative LFT following one month of operation were normal in all the patients. Similar findings were observed in the study done by Schirmer BD et al., in which they noted resolved functional abnormalities of liver within a few weeks in patients who underwent operation, compared to patients treated conservatively [10].
Liver Histopathological Changes with Gallstone Disease
Liver histological changes in patients with gall stones is thought to be the result of chronic extra hepatic large bile duct obstruction with or without repeated episodes of cholangitis [2,3]. Zuegel NP et al., had advocated liver biopsy as an important procedure, in open or laparoscopic surgery performed for gallstone disease, as 52% of patients in their study show morphological histology changes with prognostic and therapeutic relevance [11]. In our study 28 (60.6%) cholelithiasis patients had early non specific morphological changes, compared to 66% in Geraghty JN et al., study [2]. These changes were considered insignificant, as this can occur in febrile illnesses, venous outflow obstruction and intestinal infections [12]. In a study, Wang CH et al., noted acute cholestasis in 22% of cases who underwent operation for cholelithiasis [13]. But in our study only 4 (9%) of them had acute cholestasis. The presence of acute cholestasis alone in four patients is most likely related to previous small choledocholithiasis with expulsion of the stone before surgery. This is supported by the obstructive pattern of LFTs present in two of our cases. None of these patients had extensive fibrosis.
Hepatic histological changes are most severe when common bile duct obstruction is present. In our study, all 16 choledocholithiasis patients had abnormal liver histology compared to 86% in Geraghty JM et al., study [2]. Majority of them had chronic cholestasis 8 (50%), followed by acute cholestasis in 4 (25%) and sclerosing cholangitis in 4 (25%) patients. But in the study by Isogai M et al., acute cholestasis (65.4%) is noted as the most common change [14]. Kakar S et al., observed extensive fibrosis with portal-portal linking in patients of choledocholithiasis [15], this was shown to be the result of chronic cholestasis in each case. This observation is important because the fibrosis could ultimately leads to irreversible secondary biliary cirrhosis [15]. If obstruction is relieved; considerable resolution is still possible at chronic cholestasis stages, which emphasize the importance of early surgery.
In a study, Vial Gallardo M et al., attempted to determine the frequency and severity of histopathology changes and to correlate these changes with liver function [16]. They noted pathological alterations in the liver to be relatively infrequent in their series. In our study patients with acute cholestatic changes had more abnormal LFT followed by chronic cholestasis and sclerosing cholangitis patients. Histopathological changes of liver has significant correlation (p<0.001) in choledocholithiasis patients compared to cholelithiasis. Similar results were given by Lageron A et al., and they have attributed that these acute inflammatory changes found in association with gallstone disease are directly related to impairment of the flow of bile within the biliary ductal system leading to intermittent increase in biliary pressure [17].
Limitation
Limitation of the study is, we did not include a control group, as fatty metamorphosis and non specific reactive hepatitis is still possible in healthy person due to hypoxia and anaesthesia drugs [12]. Ours was a single center study with less sample size, multicenter study with larger series helps in analysing data more accurately.
Conclusion
There is a direct relationship between development of hepatic damage and patients with gallstone disease. The level of functional as well as structural changes is more severe in patients with choledocholithiasis when compared with cholelithiasis patients. Morbidity faced by patients either objective or subjective is significant and it cannot be neglected. We recommend early surgical intervention in patients of gallstone diseases irrespective of site of biliary calculus.