In the human body, FBs may cause complications such as pain, swelling, inflammation and infection [8]. To prevent these complications, FBs should be detected and extracted promptly [7,9]. In contusion traumas, presence of FBs in the tissue must be suspected. Primary management of the wound and elimination of FBs are critical for successful recovery of patient. Blind search for FBs is futile and time consuming. Search for a tiny FB in an extensive area with important anatomical structures such as the infratemporal fossa, neck, sinuses and eyes is extremely difficult. Surgery without imaging guidance is associated with the risk of tissue injury and may damage important anatomical structures. Moreover, it is exhaustive and time consuming. Several methods can be used for accurate localization of FBs in the soft and hard tissues including conventional radiography, ultrasound, MRI, CBCT and Computed Tomography (CT) [9,10].
Considering the gap of information on the diagnostic sensitivity and accuracy of MRI, ultrasound and CBCT, this study was aimed to assess and compare the sensitivity of ultrasound, MRI and CBCT for detection of barium glass, typical glass, wood and pebble FBs to find the most efficient diagnostic modality for detection and accurate localization of FBs.
Materials and Methods
This diagnostic test experimental study has been accomplished in July 2015 and has been approved by the Ethical Committee of Hamadan University of Medical Sciences with code number: Res. Project: 9307063174. In this study, four types of FBs including pieces of wood, pebbles, normal glass and barium glass measuring 5 mm×5 mm×2 mm, three were placed in three areas at both sides of two sheep heads simultaneously (sheep heads were obtained from a slaughter house).
We considered an empty place in these areas as control that makes a sample of 60 subjects {5 (FBs and empty) x 3 (areas) x 2 (sides) x 2 (heads) = 60}. These 60 subjects were evaluated by three different imaging modalities including CBCT, MRI and ultrasound. That makes a total 180 images. These 180 images were scored by an experienced radiologist. At each time of imaging, one region was considered as control. Considering the fact that FB detection on images depends on the surrounding tissue, each FB was separately placed in three different areas in the head and face of two sheep heads:
Foreign body over the bone surface (between the body of mandible and facial muscles);
Foreign body within the soft tissue (upper lip);
Foreign body in an air-filled cavity (maxillary sinus).
First, the desired site for placement of FB was prepared by making incisions [Table/Fig-1]. To incorporate the FB between the body of mandible and facial muscles, a sectional incision was made in the muscles of the area using a scalpel [Table/Fig-1a]. To incorporate the FB in the maxillary sinus, first a full mucoperiosteal flap was elevated by a periosteal elevator and then a window was created in the anterior wall of the maxillary sinus by a sharp osteotome in order to directly place the FB into the maxillary sinus [Table/Fig-1b]. In the upper lip, a tunnel on the lip surface was created by use of a scalpel to horizontally place the FB [Table/Fig-1c].
Site preparation a. Mandibular body, b. Maxillary sinus, c. Upper lip.

The objects were randomly placed in both sides of each sheep head; by doing so, the possibility of the observer guessing the location of FB was eliminated (for each location, one site was considered as the control). Then, the sheep heads were subjected to MRI, ultrasound and CBCT. To obtain CBCT scans, the sheep heads were placed in NewTom 3G CBCT system (Verona, Italy) with the exposure settings of 110 kVp, 3.6 mA and 1.8 s [Table/Fig-2a]. The CBCT scans were assessed using NNT Viewer software (NewTom, Verona, Italy). The slice thickness was 0.5 mm and the slice interval was 1 mm. All CBCT scans were observed in coronal, axial and sagittal sections. The observers were allowed to change the contrast and brightness of images as desired to enhance their observation.
Sheep head position at a. CBCT machine, b. Sonography machine, c. MRI machine.

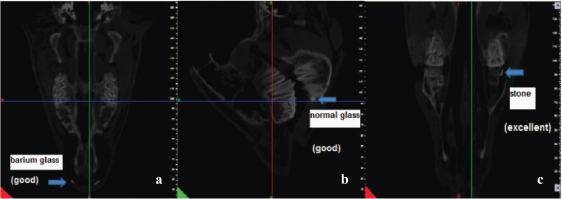
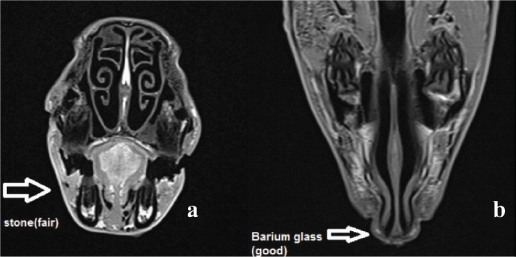
To obtain ultrasound images, sheep heads were placed in the respective location and the images were obtained using Medison (Samsung, Suwon, South Korea) ultrasound machine with 5 mHz probe [Table/Fig-2b]. The ultrasound images were assessed by a radiologist. To obtain MRI images, the sheep heads were placed in the MRI machine (Essenza, Siemens, Germany) and the images were captured with 1.5 Tesla in coronal and axial sections [Table/Fig-2c]. All images were assessed using Syngo software (NewTom, Verona, Italy). The slice thickness was 3 mm and the slice interval was zero. All images were evaluated by the observers in terms of presence/absence of FBs in the maxillary sinus, body of the mandible and upper lip in a checklist. Radiographic images were independently assessed by two observers namely a maxillofacial radiologist and a general radiologist [Table/Fig-3,4 and 5].
CBCT images. a. axial section, upper lip, b. Sagittal section, body of mandible, c. Axial section, maxillary sinus.
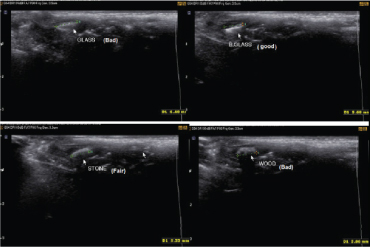
MRI images a. Sagittal section, b. Axial section.
All observers were aware of the presence of FBs but were blinded to the type and exact location of FBs. Visibility of the FBs on the images was rated by the observers using a four-point Likert scale [11,12]:
Score 0 (no image): No visibility.
Score 1 (bad image): Bad visibility (details were not visible and outlines of the FB were undetectable). Image reconstruction was poor.
Score 2 (fair image): The image had inadequate resolution and FB outlines were undetectable. Image reconstruction was inadequate.
Score 3 (good image): The image had good resolution and FB had a well-defined outline. Image reconstruction was clear.
Score 4 (excellent image): The image had excellent resolution and FB had a very well-defined outline. Image reconstruction was excellent (more sharpness).
The observers expressed their opinion regarding the visibility of FBs by allocating a score from 0 to 4 and recording it in the checklist.
Statistical Analysis
The data were analysed using Stata 11 software (by StataCorp) and chi-square test. To quantify the agreement between the imaging methods and the intra- and inter-observer measurements for each measurement type, with 95% limits of agreement extended by a 95% confidence interval for differences between the means (by using Kappa) were computed. (In the analysis, data for one of the two observers were lost and because the study was conducted a year ago, we do not have access to the data).
Results
[Table/Fig-6] shows sensitivity of the three imaging modalities for detection of foreign bodies and their sensitivity for each site. [Table/Fig-7] shows the sensitivity and specificity of the three imaging modalities for detection of FBs irrespective of their type and location. Based on the results, in general, the sensitivity of CBCT was higher than that of ultrasound and the sensitivity of ultrasound was higher than that of MRI. However, all three modalities had similar specificity equal to 100%. The sensitivity of MRI, ultrasound and CBCT was 20.83%, 33.33% and 79.17%, respectively. According to [Table/Fig-8], comparison of the sensitivity of the imaging modalities revealed significant differences only between wood and pebble, wood and barium glass and wood and normal glass in CBCT. According to [Table/Fig-9], comparison of sensitivity of the three imaging modalities for detection of FBs based on their type revealed no significant difference between MRI and ultrasound. But, comparison of MRI and CBCT for detection of pebble, normal glass and barium glass and also comparison of ultrasound and CBCT for detection of pebble, normal glass and barium glass revealed significant differences. As seen in [Table/Fig-10], comparison of sensitivity and accuracy of the three imaging modalities for detection of FBs based on their location and type revealed significant differences between MRI and ultrasound in the upper lip, between MRI and CBCT for FBs in the maxillary sinus and body of the mandible and between ultrasound and CBCT for the FBs in the maxillary sinus and body of the mandible.
Sensitivity of MRI, CBCT and ultrasound in detection of foreign body in different sites.
| Technique | Sensitivity% |
|---|
| Wood | Glass | Barium glass | Stone | Max L | Max R | Lip L | Lip R | Man L | Man R |
|---|
| MRI | 16.67 | 8.33 | 41.67 | 16.67 | 0.00 | 25.00 | 37.50 | 25.00 | 12.50 | 25.00 |
| Ultrasound | 33.33 | 33.33 | 33.33 | 33.33 | 0.00 | 0.00 | 100.00 | 100.00 | 0.00 | 0.00 |
| CBCT | 33.33 | 83.33 | 100.00 | 100.00 | 75.00 | 75.00 | 87.50 | 75.00 | 75.00 | 87.50 |
Max L= Left maxilla, Lip L= Left lip, Lip R= Right lip, Man L= Left mandible, Man R= Right mandible
Comparison of sensitivity, specificity of MRI, CBCT and ultrasound in detection of foreign body.
| Technique | Sensitivity % | Specificity % | Kappa % |
|---|
| MRI | 20.83 | 100.00 | 9.52 |
| Ultrasound | 33.33 | 100.00 | 16.67 |
| CBCT | 79.17 | 100.00 | 60.32 |
Comparison of sensitivity and specificity of the three imaging modalities based on the type of FB.
| p-value |
|---|
| Technique | S*-W | S-G** | S-BG*** | W****-G | W-BG | G-BG |
|---|
| MRI | 1.000 | 1.000 | 0.640 | 1.000 | 0.640 | 0.317 |
| Ultrasound | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| CBCT | 0.001 | 0.478 | 1.000 | 0.036 | 0.001 | 0.478 |
*stone **glass ***barium glass ****wood
Comparison of sensitivity of the three imaging modalities based on the type of foreign body.
| p-value |
|---|
| Technique | Stone | Wood | Glass | Barium Glass |
|---|
| MRI-ultrasound | 0.640 | 0.640 | 0.317 | 1.000 |
| MRI-CBCT | 0.001 | 0.640 | 0.001 | 0.001 |
| Ultrasound-CBCT | 0.001 | 1.000 | 0.036 | 0.001 |
Comparison of the accuracy of the three imaging modalities for detection of FBs based on their location.
| p-value |
|---|
| Technique | Max L* | Max R | Man L | Man R** | Lip L | Lip R*** |
|---|
| MRI-ultrasound | 1.000 | 0.467 | 1.000 | 0.467 | 0.026 | 0.007 |
| MRI-CBCT | 0.007 | 0.132 | 0.471 | 0.041 | 0.119 | 0.132 |
| Ultrasound-CBCT | 0.007 | 0.007 | 0.007 | 0.001 | 1.000 | 0.467 |
*maxillary sinus, **body of mandible, ***upper lip
Discussion
Several studies have assessed the detection of FBs by use of different imaging modalities [7,13,14]. However, studies on the use of CBCT for this purpose are scarce and to the best of authors’ knowledge, no previous study has compared MRI, ultrasound and CBCT for this purpose. This study sought to compare the sensitivity of ultrasound, MRI and CBCT for detection of wood, stone, normal glass and barium glass FBs. Detection of FB and its accurate localization are important to help surgeon safely remove it. Clinicians must choose the most efficient imaging modality for this purpose. Thus, determining the diagnostic sensitivity of different imaging modalities for this purpose can greatly help the clinician in this respect. Moreover, this study also highlights that there can be certain foreign bodies like wood which may go undetected by the X-ray imaging techniques and thus may lead to misdiagnosis and impaired treatment. In the current study, ultrasound, MRI and CBCT were compared and the results showed that the diagnostic sensitivity of CBCT (79.17%) was higher than that of ultrasound (33.33%) and MRI (20.83%). None of the imaging modalities could well detect woodpieces and the diagnostic sensitivity of MRI, ultrasound and CBCT for wooden FBs was 16.67, 33.33 and 33.33%, respectively. However, all three modalities, particularly CBCT, had good sensitivity for detection of stone and barium glass. The specificity of all three modalities was 100%. Diagnostic sensitivity of MRI and ultrasound for detection of FBs in the upper lip and CBCT for all areas was almost the same.
Our findings were somehow expected considering the high resolution of CBCT and the ability to evaluate desired sections of the tissue, the limitations of ultrasound in evaluation of air-filled cavities such as sinuses or objects next to hard tissues such as bone (due to its high density), inability of MRI to focus on the desired areas (due to the direction of sections of tissues) and the risk of missing the FBs between sections (due to their small size or their orientation in the tissue).
Moreover, size of the object and its position in the tissue as well as the direction of sections significantly affect the detection of FBs by use of MRI; in general, MRI is not efficient enough to be the first choice of imaging modality for detection of FBs (based on our study).
High accuracy of CBCT for detection of FBs compared to ultrasound and particularly MRI, its lower cost (compared to MRI) and lower patient radiation dose than CT suggest the use of CBCT as the first diagnostic modality in cases suspected for FBs.
Based on the results of previous studies and our current findings, MRI should not be used as the first imaging modality for detection of FBs especially when the nature of FB is not known because it generates high artifacts in presence of metal objects and it is costly and time consuming. Also, the possibility of different interpretations by the observers is higher in MRI [15].
Ultrasound is an affordable and applicable modality for detection of radiolucent FBs (wood, sand and plastic) in the superficial and deep soft tissues (as deep as 3 cm). However, it is not efficient for detection of FBs in air-filled cavities (such as the maxillary sinus) or at the bone-soft tissue interface (as in the body of mandible) [16]. Due to high prevalence of minor traumas and inability to visually observe the FB penetrated into the tissue (especially wood), undetected FBs can cause refractory infections since they provide an area for accumulation of microorganisms. Due to the absence of inflammation and swelling in presence of FBs in vitro and inability to use contrast radiography, the frequency of undetected FBs may be higher compared to in vivo [17]. On the other hand, CT and CBCT can be used as standard non-invasive modalities for detection and localization of FBs prior to surgery to determine their exact shape and size [16]. Our results showed that objects with higher density such as pebbles created higher quality images in all three modalities. Objects with lower density such as wood were not well visualized by any of the three modalities. Javadrashid R et al., showed that all FBs except for wood had best visibility on CT scans. Wood was only detectable by ultrasound when its size exceeded 0.5 mm. Conventional radiography and CT had equal accuracy for detection of graphite and metal FBs; MRI had the lowest efficacy and accuracy among all modalities [17].
Ranajit P et al., reported that radiopaque objects (stone) were well visualized by ultrasound while lucent objects (wood) were hardly detected. The same results were obtained for CT and MRI. Also, ultrasound had high accuracy for detection of FBs in the superficial and deep soft tissue (as in the lips) while CT was capable of accurately locating the FB in all areas [14].
Javadrashid R et al., compared the efficacy of CT and CBCT for detection of FBs and showed that CBCT was not suitable for detection of FBs with low density, which was in line with our results since our study showed that CBCT (as well as other modalities) had lower diagnostic accuracy for detection of low density materials such as wood and glass [13].
Aras M et al., showed that ultrasound was more efficient than conventional radiography and CT for detection and localization of FBs with low radiopacity; their finding was confirmed in our study since ultrasound detected 100% of FBs in the upper lip (which was relatively superficial) [7]. Blankenship RB et al., demonstrated that wooden objects in air-filled cavities (such as the maxillary sinus) or on the bone surface could not be detected by ultrasound. In addition they showed that ultrasound was a valuable modality for detection of FBs entrapped in the soft tissue and CT was the most efficient modality for detection of FBs entrapped in air-filled cavities [18]. Shrestha D et al., confirmed this finding and reported that ultrasound could be used for assessment of cases suspected for non-radiopaque FBs in the soft tissue [19]. Ober CP et al., assessed the diagnostic sensitivity of ultrasound, CT and MRI for detection of FBs in dog’s hand and revealed that CT was the most accurate diagnostic modality for visualization of wooden FBs followed by ultrasound and MRI [20]. Since CT and CBCT are relatively similar, their findings were in agreement with our results, showing 79.17, 33.79 and 20.83% sensitivity for CBCT, ultrasound and MRI, respectively. Lagalla R et al., showed that conventional radiography underestimated FBs in the eyes and could not visualize plastic or dry/wet wood; CT was capable of visualization and differentiation of intraocular FBs based on attenuation value. Severe artifacts prevented visualization of metal, glass and graphite FBs by MRI while plastic and wooden FBs had adequate visibility. In spite of this, conventional radiography was suggested as a prerequisite for MRI [21]. Zhonghua Y et al., concluded that MRI was superior to CT for detection and localization of non-magnetic intraocular FBs with low density and yielded high positive rates. However, MRI and CT were not reliable for detection of FBs in the orbit wall. They were not suitable for detection of non-magnetic intraocular FBs either [22].
Lue A et al., reported that the accuracy of CT for detection of woodsticks in dog’s hand was higher than that of ultrasound and the latter was more efficient than MRI [23]. The main difference between their study and ours was the location of FB. Dog’s hand has a complex anatomy and presence of small bones in this region complicates detection of radiolucent FBs. Due to the acoustic shadow of bones, detection of FBs by ultrasound is even more difficult; as the result, CT can better detect wooden FBs in this region than ultrasound. Another study demonstrated that ultrasound was a valuable modality for detection of FBs entrapped in the soft tissue while CT was the most efficient modality for detection of objects entrapped in air-filled cavities [19]. Inability to conduct studies on human was our limitation.
Conclusion
CBCT had the highest diagnostic sensitivity for detection of FBs in all areas except for the FBs in the upper lip, for which, ultrasound yielded the highest diagnostic sensitivity. On the other hand, MRI did not yield high sensitivity for detection of FBs in any of the tested locations (compared to ultrasound and CBCT). All three modalities had 100% specificity.
Overall, CBCT had the highest diagnostic sensitivity for detection of FBs. Thus, CBCT can be used as the first line imaging modality for detection of FBs in trauma patients.
Max L= Left maxilla, Lip L= Left lip, Lip R= Right lip, Man L= Left mandible, Man R= Right mandible
*stone **glass ***barium glass ****wood
*maxillary sinus, **body of mandible, ***upper lip