Bi-Pedicle Fixation of Affected Vertebra in Thoracolumbar Burst Fracture
Pravin Padalkar1, Varshil Mehta2
1 Associate Professor, Department of Orthopaedics, MGM Medical College, Navi Mumbai, Maharashta, India.
2 Intern, Department of Internal Medicine, MGM Medical College, Navi Mumbai, Maharashta, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Varshil Mehta, 103, Sky High Tower, Orlem, Tank Road, Malad West, Mumbai-400064, Maharashta, India.
E-mail: varshil91@gmail.com
Introduction
Burst fractures of the spine account for 14% of all spinal injuries and more than 50% of all thoracolumbar trauma. However, there is ambiguity while choosing the right treatment plan. Short Segment Pedicle screw Fixation (SSPF) has become an increasingly popular method of treatment of thoracolumbar burst fractures, providing the advantage of incorporating fewer motion segments in the fixation. Various biomechanical studies showed that the use of pedicle screws could achieve stable construct within short-segment fixation.
Aim
To evaluate the efficacy of SSPF using longest possible screws in both pedicles of fractured vertebra.
Materials and Methods
A retrospective chart review of 25 single burst thoracolumbar fracture patients, operated between May 2009 to 2015 in a tertiary care trauma center, was conducted. Preoperative and post-operative plain radiographs were evaluated for kyphotic angulations using the traditional Cobb method. Anterior Vertebral Height (AVH), Posteriors Vertebral Height (PVH) were measured preoperatively and immediate postoperatively. Average percentage loss of AVH and mid-sagittal height were calculated on preoperative and postoperative X-rays on follow up.
Results
Fourteen men and 11 women with an average age of 42.92 years comprised the study population. Mean age at the time of operation was 34.5±14.2 years. Mean operation time was 168±72 (minutes). Average hospitalization time was 9±7 (days). Mean blood loss was 515±485 (ml). There were two cases of postoperative infection and implant failure each. A mean of 15.2° of kyphosis correction was attained from pre-operation to post-operation (p<0.0001). Although, there was a 15° average improvement of kyphosis post-fixation, loss of correction over time was nearly 8°, resulting in a 7° mean correction of kyphosis. A mean loss of AVH on postoperative radiograph was 6.12% and maintained 12.4% at the time of review (p<0.001). Similarly, there was 32.8% mid-sagittal height loss at time of injury, which was improved to only 12.6% as compare to initial height loss (p<0.0001).
Conclusion
In this study, we propose SSPF using longest possible screws in both pedicle of fractured vertebra. Bi-pedicular fixation gives significant radiological corrections.
Kyphosis, Short segment pedicle-screw fixation, Thoracolumbar fracture
Introduction
In 1963, Holdsworth described burst fractures. Burst fractures of the spine account for 14% of all spinal injuries and greater than 50% of all thoracolumbar trauma [1]. Disagreement also exists regarding the choice of the surgical approach. The most important motive behind internal fixation is to minimize the number of vertebral levels which are involved in the fusion of a spine fracture. With the advent of SSPF, it is now possible to incorporate fewer motion segments during the fixation and has emerged as one of the most popular method for managing burst fracture of thoracolumbar vertebrae management method for treating burst fractures of thoracolumbar vertebra.
Various biomechanical studies showed that the use of pedicle screws could achieve stable construct within short-segment fixation [2]. Failure of SSPF attributed many factors; studies show that by inserting screws at the fracture level, the construct becomes biomechanically stronger [3]. Many of SSPF studies have used inconsistently unilateral or short pedicel screw in fractured vertebrae [4,5].
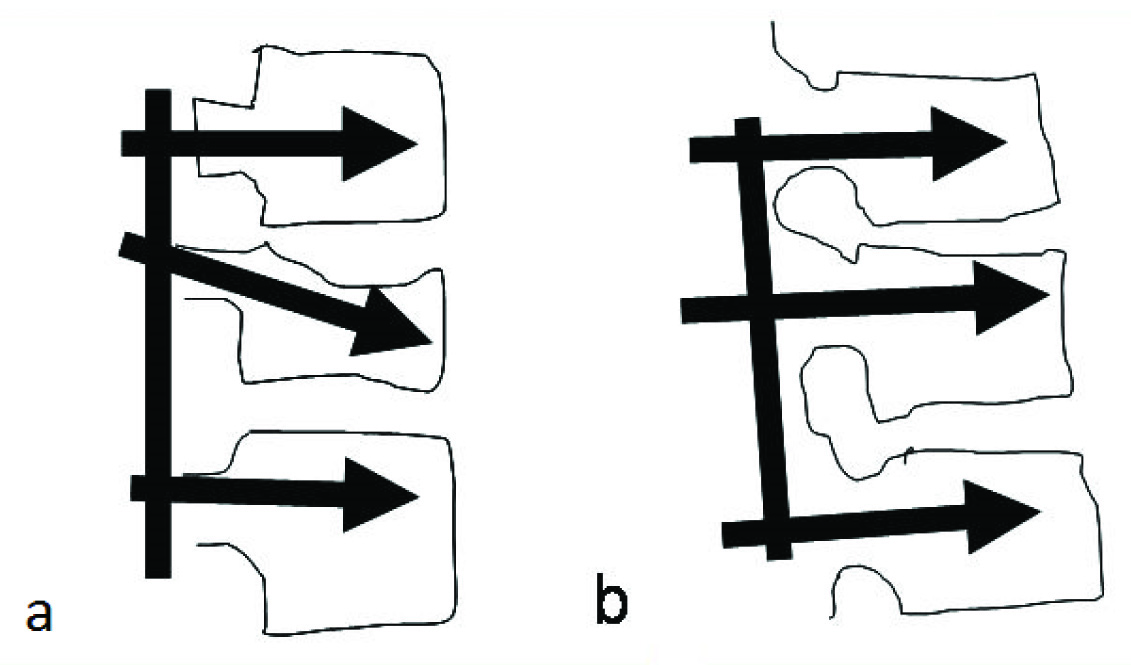
In this study, we propose SSPF using longest possible screws in both pedicles of the fractured vertebra. A long pedicle screw in the bilateral fractured vertebrae supports subchondral bone, superior endplate and allows more correction by cantilever forces created by distraction maneuver. This three point fixation also prevents collapse and loss of kyphosis achieved during correction manoeuvre as seen in [Table/Fig-1].
Correction of Kyphosis using distractive and cantilever forces: a) Before; b) After.
Materials and Methods
This study was conducted between the period of May 2009 to 2015. The study was approved by the ethical committee of the center. Inclusion criteria for cases in the study required confirmed thoracolumbar fracture by plain radiographs, computed tomography, and magnetic resonance imaging. Surgical indications included more than 50% loss of vertebral body height, kyphosis progressing 20% or more, more than 50% of canal involvement, posterior ligamentous complex injury.
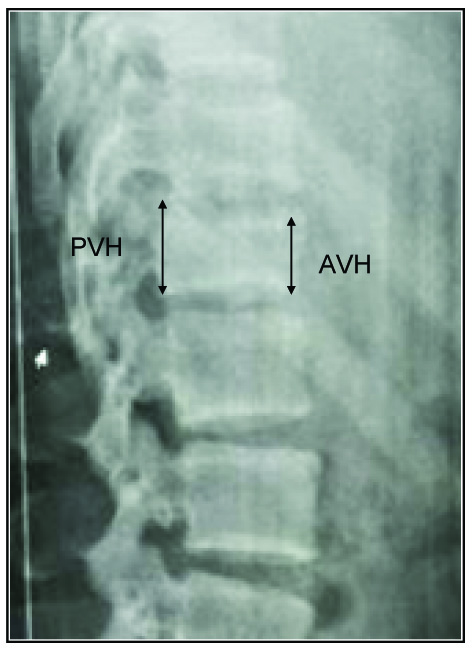
Twenty-five patients qualified and were reviewed retrospectively in this study. Patients were also graded preoperatively and postoperatively based on the Frankel scale [6]; Plain radiographs were evaluated preoperatively and postoperatively for kyphotic angulations using the traditional Cobb method [7]. [Table/Fig-2] shows how AVH and PVH were measured preoperatively, immediate postoperatively and at 18 months respectively (it was recommended to every patient to undergo removal at 18 month). Average percentage loss of AVH and mid-sagittal height were also calculated on preoperative and postoperative X-rays on follow up.
Demonstrates the measurement of PVH and AVH method.
Surgical Procedure
The first author performed all surgeries in this study. The posterior spinal approach was made one level above and below the fracture. Pedicle screws were placed at one level above and below the fracture site. Fracture level screws were inserted at the same time with the other screws prior to compression/distraction, and were included into the lordosing distracting manoeuvre. Both the fractured pedicles were inserted and care was taken to insert longest possible screws so that they can support subchondral bone and the superior end plate of fractured vertebrae. Kyphosis correction achieved by cantilever forces created by distraction and compression manoeuvre.
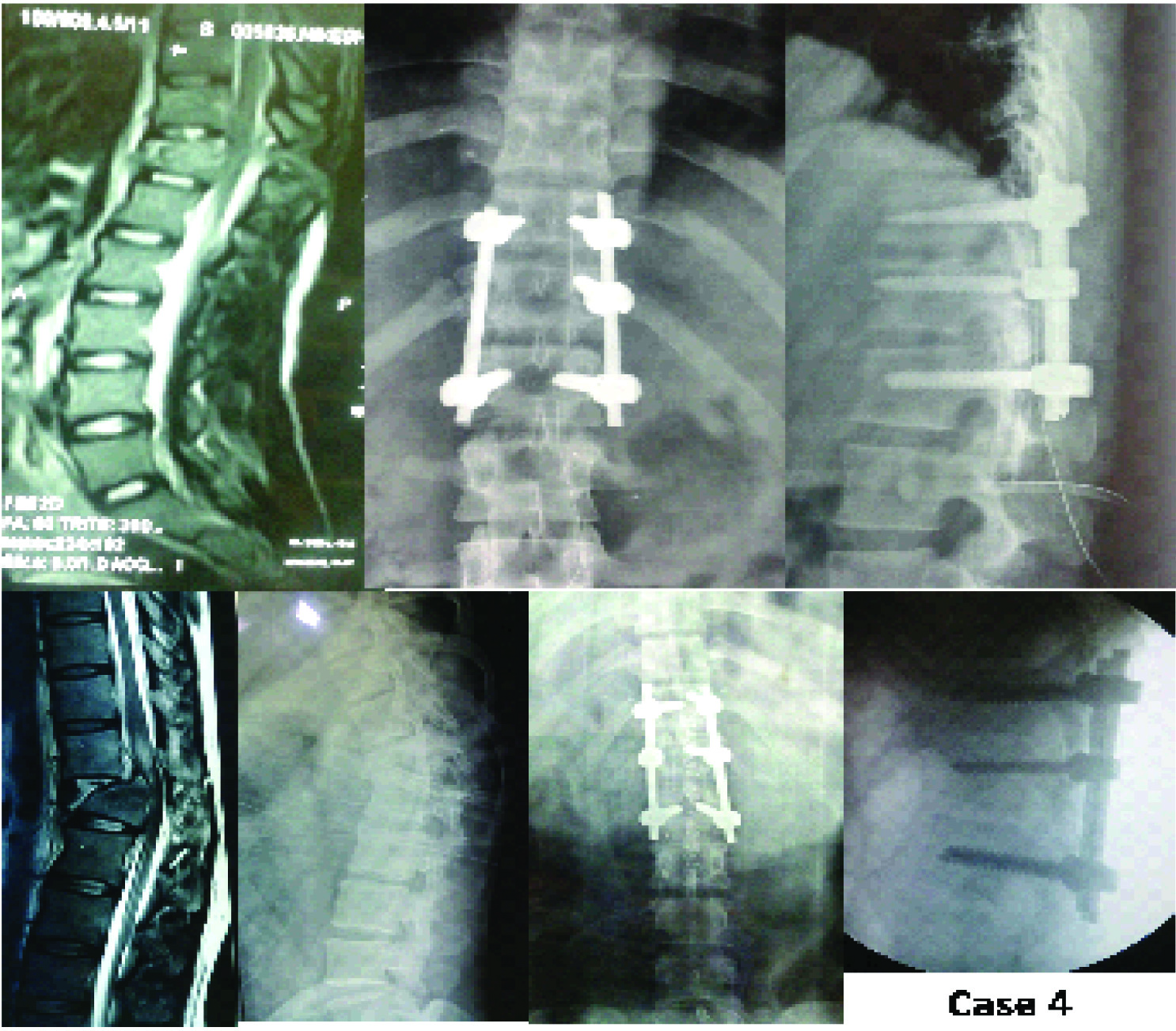
[Table/Fig-3] demonstrates an excellent correction done at one-month postoperative interval. Visualization laminectomy performed for confirmation of indirect decompression achieved by distraction manoeuvre when indicated by the presence of compression over neural tissue in MRI. No fusion was performed in all patients so that elective implant removal can be performed after 18 months when the fracture is healed.
Correction of kyphosis at one month postoperative period.

[Table/Fig-4] demonstrates one of the cases for which elective implant removal was performed at 18-months interval after fracture was healed.
An 18 month postoperative implant removal.
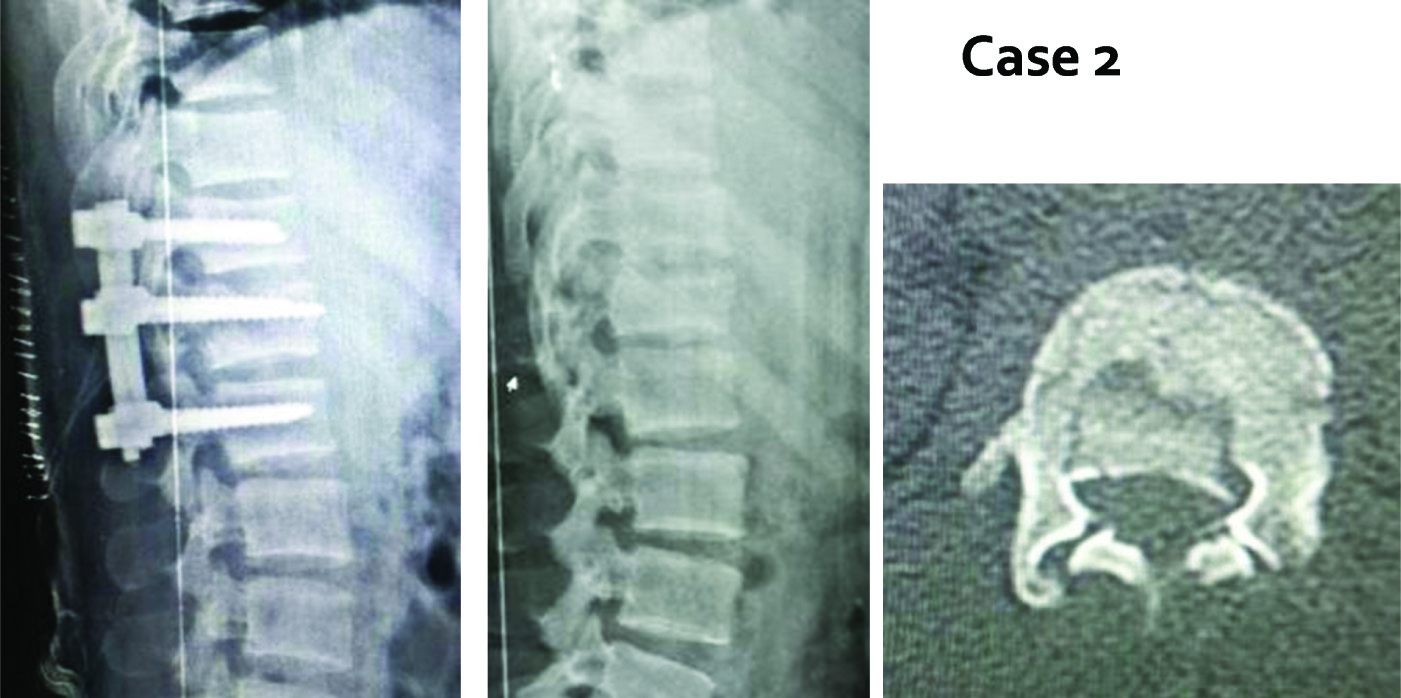
Some of the cases which had fractured pedicle or unsafe for insertion of pedicle screws were abandoned and excluded from the study. [Table/Fig-5] demonstrates such one case, in which only single screw was inserted and hence, was excluded from the study.
Postoperative follow up at 16 months of uni-pedicular fixation (Excluded case).
Results
Fourteen men and eleven women with an average age of 42.92 years (range 18 to 74 years) comprised the study. Mean age at the time of operation was 34.5±14.2 years (range 18–74). Male to female ratio of 1.27 the majority of fractures resulted due to fall from height (15 cases {60%}), the remaining cases resulted from car accidents (10 cases 40.0%). Preoperative Frankel grading of patients was done and has been shown in [Table/Fig-6]. Mean operation time was 168±72 (minutes). Average hospitalization time was 9±7 (days). Mean blood loss was 515±485 (ml). There were two cases of postoperative infection and implant failure each [Table/Fig-6].
Characteristics and demography.
| Short Segment Fixation | N = 25 |
| Gender: N (%) | Males: 14 (56%) |
| Females: 11 (44%) |
| Age (years) at the time of operation | 34.5±14.2 (Range 18-74) |
| Mean Operation Time (Minutes) | 168±72 |
| Mean Blood Loss (mL) | 515±485 |
| Fracture Level | T12 | 9 |
| L1 | 13 |
| L2 | 3 |
| Follow Up Duration (Months) | 21.64±11.32 |
| Frankle Grade | A | 1 |
| B | 1 |
| C | 9 |
| D | 6 |
| E | 8 |
A mean loss of AVH on postoperative radiograph was 6.12% and maintained 12.4% at the time of review (p<0.001). Similarly, there was 32.8% midsagittal height loss (calculated based on average midsagittal diameter at vertebrae above and below) at the time of injury, which was improved to only 12.6% as compare to initial height loss (p<0.001) [Table/Fig-7].
AVH loss and mid-sagittal height loss.
| Radiograph | Mean | ±SD | Minimum | Maximum |
|---|
| Anterior vertebral height (AVH) loss (%) |
| At injury | 38.00 | 14.2 | 8 | 72 |
| Post-Injury | 6.12 | 3.1 | 0 | 18 |
| 18 months | 12.4 | 18.7 | 0 | 22 |
| Loss of mid-sagittal height |
| At injury | 32.8 | 12.10 | 8 | 47 |
| Post-surgery | 12.6 | 4.1 | 0 | 14 |
A mean of 15.2° of kyphosis correction was attained from pre-operation to post-operation (p<0.001). Although there was a 15° average improvement of kyphosis post-fixation, loss of correction over time was nearly 8°, resulting in a 7° mean correction of kyphosis. The postoperative images are shown in [Table/Fig-3,4 and 5].
Discussion
Burst fractures are the most common type of fracture of the thoracolumbar spine, accounting for greater than 50% of all thoracolumbar trauma [1]. Burst fractures typically involve violation of the inferior and/or superior endplates, and therefore the deformity may progress by gradual settling of the discs into the fractured endplates and vertebral body. Farcy JP et al., proposed that if the sagittal index exceeds 15 degrees [8], the biomechanical environment favors the progression of kyphosis [9].
Traditional pedicle screw instrumentation allowed a correction of kyphosis and an indirect reduction of thoracolumbar burst by distraction and ligamentotaxis. However, due to frequent failure to support the anterior spinal column, there was often a loss of correction leading to a high rate of failure [10-14]. Failure to restore the anterior column support can lead to secondary kyphosis, instability, pain and late onset neurologic deficit, depending primarily on residual load transfer capacity of the fractured vertebral body [15,16].
SSPF is the use of pedicle screw instrumentation one level cephalad to and one level caudal to the fractured vertebra. It has become an increasingly popular method of treatment of thoracolumbar burst fractures, providing the advantage of incorporating fewer motion segments in the fixation [17]. A cadaveric study of short-segment posterior fixation with pedicle fixation at the level of the fracture (short same-segment fixation) showed that short same-segment fixation provides more biomechanical stability than traditional SSPF [3]. However, a review of literature demonstrated that SSPF led to 9%-54% incidence of implant failure and long term loss of kyphosis correction, and up to 50% of patients with implant failure had moderate to severe pain [10,13,18,19].
Failure of SSPF can be attributed to instrumentation failure (i.e., bending and/or breaking of the screws), vertebral factors (i.e., primary osseous collapse or secondary to osteoporosis), or a combination of both [8]. Other possible factors include inadequate fixation points on the vertebrae and insufficient anterior column support [20].
Limitation
Bi-pedicular fixation works on ligamatotaxis principle and due to which, only early presentations give good results postoperatively. Hence, they were only included. This study also did not compare the significance of using different lengths of the pedicle screws (amongst the longest ones) used during fixation and the sample size was small. Hence, more large scale and multi centric based studies should be conducted.
Conclusion
In this study, we propose SSPF using longest possible screws in both pedicle of fractured vertebra. Bi-pedicular fixation gives significant radiological corrections. A long pedicle screw in bilateral fractured vertebrae supports subchondral bone, superior endplate and allows more correction by cantilever forces created by distraction manoeuvre. This three point fixation also prevents collapse and loss of kyphosis achieved.
[1]. Dai LY, Jiang LS, Jiang SD, Posterior short-segment fixation with or without fusion for thoracolumbar burst fracturesJ Bone Joint Surg Am 2009 91(5):1033-41. [Google Scholar]
[2]. Kothe R, Panjabi MM, Liu W, Multidirectional instability of the thoracic spine due to iatrogenic pedicle injuries during transpedicular fixation: a biomechanical investigationSpine 1997 22(16):1836-42. [Google Scholar]
[3]. Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, Garfin S, Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fractureSpine 2007 32(14):1503-07. [Google Scholar]
[4]. Guven O, Kocaoglu B, Bezer M, Aydin N, Nalbantoglu U, The use of screw at the fracture level in the treatment of thoracolumbar burst fracturesClinical Spine Surgery 2009 22(6):417-21. [Google Scholar]
[5]. Korovessis P, Repantis T, George P, Treatment of acute thoracolumbar burst fractures with kyphoplasty and short pedicle screw fixation: transpedicular intracorporeal grafting with calcium phosphate: a prospective studyIndian Journal of Orthopaedics 2007 41(4):354 [Google Scholar]
[6]. Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, et al, The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegiaSpinal Cord 1969 7(3):179-92. [Google Scholar]
[7]. Cobb JR, Outline for the study of scoliosisInstr Course Lect 1948 5:261-75. [Google Scholar]
[8]. Farcy JP, Weidenbaum M, Glassman SD, Sagittal index in management of thoracolumbar burst fracturesSpine 1990 15(9):958-65. [Google Scholar]
[9]. Patrick T, Russel CH, Christian AL, Dominique GP, Rene PL, Functional and radiologic outcome of thoracolumbar and burst fractures managed by closed orthopedic reduction and castingSpine 2003 28:2459-65. [Google Scholar]
[10]. Kramer DL, Rodgers WB, Mansfield FL, Transpedicular instrumentation and short-segment fusion of thoracolumbar fractures: a prospective study using a single instrumentation systemJournal of Orthopaedic Trauma 1995 9(6):499-506. [Google Scholar]
[11]. Parker JW, Lane JR, Karaikovic EE, Gaines RW, Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 4½-year seriesSpine 2000 25(9):1157-70. [Google Scholar]
[12]. Speth MJ, Oner FC, Kadic MA, de Klerk LW, Verbout AJ, Recurrent kyphosis after posterior stabilization of thoracolumbar fractures: 24 cases treated with a Dick internal fixator followed for 1.5-4 yearsActa Orthopaedica Scandinavica 1995 66(5):406-10. [Google Scholar]
[13]. Benson DR, Burkus JK, Montesano PX, Sutherland TB, McLain RF, Unstable thoracolumbar and lumbar burst fractures treated with the AO fixateur interneClinical Spine Surgery 1992 5(3):335-43. [Google Scholar]
[14]. Müller U, Berlemann U, Sledge J, Schwarzenbach O, Treatment of thoracolumbar burst fractures without neurologic deficit by indirect reduction and posterior instrumentation: bisegmental stabilization with monosegmental fusionEuropean Spine Journal 1999 8(4):284-89. [Google Scholar]
[15]. Kim KS, Oh SH, Huh JS, Noh JS, Chung BS, Dorsal short-segment fixation for unstable thoracolumbar junction fracturesJ Korean Neurosurg Soc 2006 40:249-55. [Google Scholar]
[16]. McCormack T, Karaikovic E, Gaines RW, The load sharing classification of spine fracturesSpine 1994 19(15):1741-44. [Google Scholar]
[17]. Alanay A, Acaroglu E, Yazici M, Oznur A, Surat A, Short-segment pedicle instrumentation of thoracolumbar burst fractures: does transpedicular intracorporeal grafting prevent early failure?Spine 2001 26(2):213-17. [Google Scholar]
[18]. Altay M, Ozkurt B, Aktekin CN, Ozturk AM, Dogan Ö, Tabak AY, Treatment of unstable thoracolumbar junction burst fractures with short-or long-segment posterior fixation in magerl type a fracturesEuropean Spine Journal 2007 16(8):1145-55. [Google Scholar]
[19]. Mclain RF, Sparling E, Benson DR, Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary reportJ Bone Joint Surg Am 1993 75(2):162-67. [Google Scholar]
[20]. Esses SI, Botsford DJ, Wright T, Bednar D, Bailey S, Operative treatment of spinal fractures with the AO internal fixatorSpine 1991 16(3):S146-50. [Google Scholar]