Dentistry is a profession where performance is restricted to an area covering only a few tens of millimetres of the mouth requiring repeated and precise force applications [1]. These situations strictly demand a fixed posture that can create debilitating upper extremity musculoskeletal disorders among dentists with a prevalence rate of 64% to 93% [2,3]. A healthy dentist is a pre-requisite for a successful dental practice and ergonomics is its core principle [4]. It is one of the most effective tools by which the workplace can be optimized where in several factors like environment, equipment, positioning, performance and instrument design synergize to eliminate the risk of cumulative injury [5,6].
Pinch is a type of prehension pattern that uses two or three fingers to manipulate items in coordination with thumb movements, without the contact of the palm [7]. The finger pinches include pulp pinch, lateral pinch, tripod pinch, and five-finger pinch. Tripod pinch occurs when the thumb, index, and middle fingers surround the object [8]. PS is the measurable ability to exert force with fingers [9] and is commonly measured in hand and finger function evaluations using Manual Muscle Strength Testing (MMST) [10,11]. In addition to MMST, grip and PS measurements with dynamometers have been used to measure the outcome of peripheral nerve function [12-16]. However, quantitative measurements that can specifically measure the intrinsic muscle strength are required. This can be achieved with the help of a Jamar® Hydraulic Pinch Gauge.
Periodontal SRP is one of the most routinely performed task that requires a high level of pinch force and results in finger fatigue, as gaining access to some areas of the oral cavity is tedious. The average pinch force exerted during SRP is 11% to 20% of the maximum PS [17]. If done incorrectly, SRP causes sustained non-neutral positions resulting in drastically decreased pinch force.
No one would consider performing strenuous exercises without stretching and doing strengthening manoeuvres first. However, oral care providers subject their muscles to arduous activity daily without properly preparing their bodies for the workplace. Dong H et al., compared the peak pinch force patterns during SRP between experienced dentists and dental students and found that the dental students applied greater mean peak pinch force, while a higher magnitude of force was recorded among dentists that could pose a risk for carpal tunnel syndrome and other hand and wrist disorders [17]. To reduce the risk of these injuries, various hand and finger stretches may be performed prior to commencement of SRP which may amplify the efficacy of the scaling strokes and also reduce excessive strain and fatigue of the finger muscles [18].
However, to the best of our knowledge, there is no published data regarding the effects of hand and finger stretches, performed prior to SRP, on PS in dental professionals. Hence, the aim of this pilot study was to comparatively evaluate the PS of the finger muscles, prior to and after SRP, amongst dental cohort performing additional chair-side hand and finger stretches to those not performing the same.
Materials and Methods
Study Sample
The study was conducted at Mahatma Gandhi Mission’s Dental College and Hospital, Navi Mumbai, India, by Department of Periodontology in conjunction with Mahatma Gandhi Mission’s College of Physiotherapy, Navi Mumbai, India. A purposive sample size of 40 dental professionals (since this was a pilot study, a purposive sampling of 40 subjects was done), willing to participate in the study, with sound knowledge of the principles of instrumentation were recruited for the study aged between 18-30 years from January 2015 to March 2015. None of the subjects reported having had injuries or previous surgeries in the hand and wrist area. Subjects with physician diagnosed upper-extremity musculoskeletal disorders and rheumatoid arthritis were excluded; and the subjects currently on sedative or muscle relaxant therapy or with a dominant left hand. For SRP, patients with moderate to heavy calculus exhibiting signs of periodontal disease were recruited from the outpatient department of the same institution. The nature and purpose of the study was explained in detail to the providers and the patients and an informed consent was obtained from both, prior to commencement of the study. The study was approved by the Institutional Ethics Committee allied to Maharashtra University of Health Sciences Nashik, India.
Study Design and Procedure
The research design chosen for this study was a parallel, quantitative with an interventional approach. All the dental professionals were instructed to perform SRP, while adhering to the principles of instrumentation, on selected patients, for a period of 30 minutes. A set of supragingival scalers and Gracey curettes #1-2 to #17-18 (Hu-Friedy, Chicago, IL, USA) were used on each patient for SRP.
A single investigator recorded PS in pounds (lbs), prior to and after SRP, using a Jamar® Hydraulic pinch gauge (Patterson Medical, Warrenville, IL, USA) with a three jaw chuck grip. To test the validity, examiners placed known weights on the bridge of the pinch gauge. It was proven to be most valid with an accuracy of ±0.5 lbs.
During the PS evaluation, the participants were seated upright with shoulders adducted and neutrally rotated, elbows flexed at 90o and the forearm and wrist in neutral position with feet flat on the floor. Wrist positions upto 30o extension was permissible [19]. This position was checked with a goniometer and maintained throughout the testing process.
To ensure the safety of participants and the pinch gauge, the operator mounted the Jamar® hydraulic pinch meter on a table such that it was immobile during the testing process. The participants were instructed to grasp the pinch gauge with the thumb, index finger, and middle finger, such that the pulp of the thumb was positioned over the pinch gauge, the index and middle finger positioned below it. Each participant was then asked to apply maximum voluntary pinch force thrice, prior to and after SRP and the highest reading was considered. The operator encouraged the participants to squeeze as hard as possible during each trial by saying “go, go, stop” as use of consistent instructions is important for standardization of test protocol [9]. The contraction time was no more than two seconds.
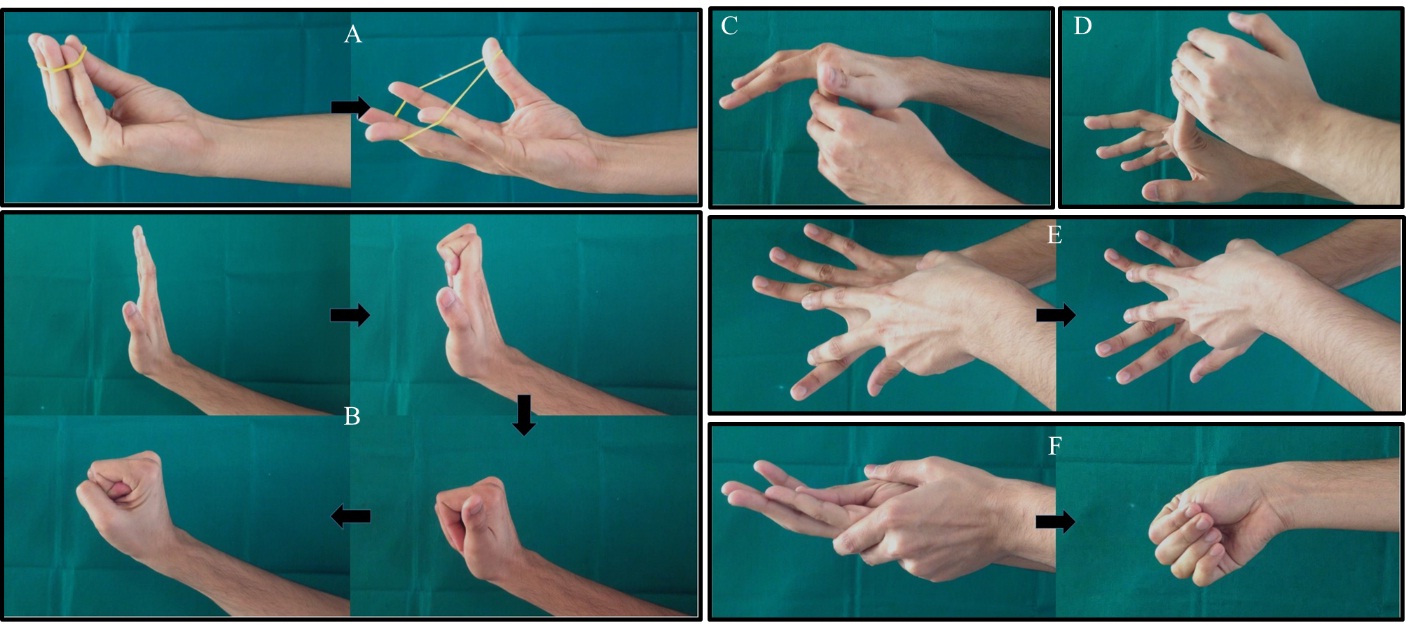
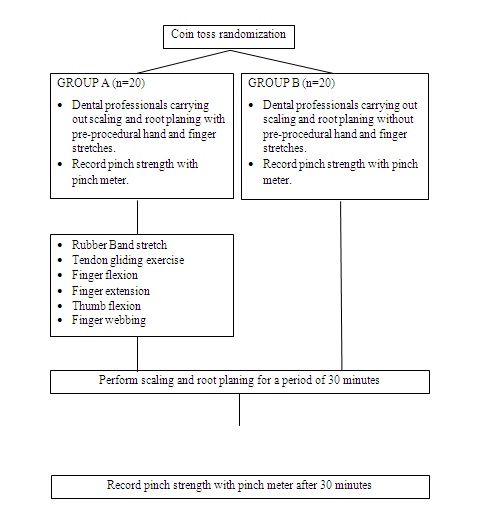
Subjects were randomly divided into two groups using a coin toss method, where Group A comprised of subjects performing hand and finger stretches prior to SRP and Group B comprised of subjects who did not perform the stretches and served as controls. Under the supervision of the investigator, subjects in Group A performed the stretches as described and shown in [Table/Fig-1,2] [18,20].
Techniques of finger stretches.
| Stretches | Technique |
|---|
| Rubber band finger stretch | A rubber band was extended between the fingers of hand and gently stretched till resistance was felt. This position was held for three seconds and then fingers relaxed back to rest position [18]. |
| Tendon glide | Keeping the right hand wrist relaxed and following the line of the fingers and thumb, fingers were pointed straight up. The fingers were curled so that the top two joints in them were bent and wrapped with the fingertips touching the base of the fingers. Then, the fingers were advanced to making a fist by bending the knuckles and finally relaxed so that the fingertips touched the base of the palm [18]. |
| Finger flexion and extension | The left thumb was used to extend the fingers of right hand while keeping the fingers of left hand cupped behind them over the dorsum to flex them [20]. |
| Thumb flexion | The fingers of left hand were cupped around the radial border of the thenar eminence of the right thumb and the left thumb was placed along the palmar surface of the right thumb to extend it. To flex and oppose the thumb, the left hand was cupped around the dorsal surface of the right hand that pushed the thumb towards the little finger [20]. |
| Finger webbing | The right hand was positioned flat on a hard surface. The fingers were fully extended such that they touched each other. The fingers were then spread apart as far as possible with the help of two digits of the left hand. This position was held for two seconds and then released [20]. |
a) Rubber band finger stretch; b) Tendon glide; c) Finger extension; d) Finger flexion; e) Finger webbing; f) Thumb flexion.
Subjects of group A repeated all of these stretches five times. PS was again recorded for all subjects 30 minutes after SRP using the Jamar® Hydraulic Pinch Gauge.
Statistical Analysis
Data analysis was done using Windows PC based software “MedCalc Statistical Software” version 13.3.1. (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2014). All testing was done at alpha 0.05 (95% confidence limits). The data for PS measurement was expressed as means with Standard Deviation (SD). Change from baseline values was calculated. Inter-group difference was analysed for variability at baseline and 30 minutes after SRP using unpaired t-test. Intra-group comparison of PS measurement was done using paired t-test.
Results
The present study was a parallel design interventional study with the purpose of biomechanically assessing the effect of finger stretches on PS before and after performing SRP. The mean age of subjects selected for Group A and B was 20.15 and 20.35 years respectively with no statistical difference. [Table/Fig-3] presents the flowchart of the study. The study sample consisted of 40 dental professionals randomly divided by coin toss method into two groups.
[Table/Fig-4] represents the mean±SD of PS recorded for both groups. A sharp decline in PS post SRP was noted for Group B (10.675±2.478 lbs; difference of mean was -2.975 lbs) while a slight change was noted for Group A (13.725±2.557 lbs; difference of mean was -0.7 lbs [Table/Fig-5]).
Results of paired t-test comparing mean±standard deviation pre-SRP PS with post-SRP PS for Group A and Group B.
| Groups | Pre-SRP (lbs) | Post-SRP (lbs) | p-value |
|---|
| Group A | 14.425±2.577 | 13.725±2.557 | p<0.001 |
| Group B | 13.65±2.636 | 10.675±2.478 | p<0.001 |
PS = Pinch Strength, SRP = Scaling and root planing, lbs = pounds
Results of unpaired t-test comparing the difference of mean±standard deviation in PS between Group A and Group B.
| Groups | Difference of means in PS | p-value |
|---|
| Group A | -0.7±0.6366 lbs | p=0.05 |
| Group B | -2.975±1.292 lbs |
PS = Pinch Strength, lbs = pounds
Intergroup comparison of difference of mean post SRP PS values using unpaired t-test revealed a statistically significant difference (p-value=0.05). Intragroup comparison of the PS values pre and post SRP revealed a statistically significant difference (p-value <0.001) within groups A and B).
Discussion
The smaller muscles of the hand and fingers not only aid in grasping the dental instruments with a modified pen grip, but also provide precision and finesse during dental procedures [21]. The alarming nature of upper extremity injuries related to dentistry is on the rise. The outlook towards the same has shifted from surgical and palliative care to prevention. Well-conditioned muscles have better control and endurance that allow for free wrist movement, and reduce the likelihood of repetitive strain injuries, carpal tunnel syndrome, De Quervain’s tenosynovitis, trigger finger, amongst a few [22].
A survey conducted by the American Dental Association showed that 62% of dentists in private practice stated that they received insufficient training on the applications of ergonomics when attending dental school [23]. This may result in constant fatigue of the fingers which poses a risk for Carpal Tunnel syndrome and other hand and wrist disorders amongst dental professionals.
To add to this, instrument design and weight are important ergonomic factors that are most often neglected. This was demonstrated in a study by Dong H et al., where it was reported, through the use of custom-designed dental scaling instruments with different handle diameters and weight, that the instrument with a large diameter and a light weight required the least amount of muscle load and pinch force [24].
PS is an objective measurement of overall hand strength that provides evidence for determining functional improvements and designing appropriate interventions, the decrease in the PS of finger muscles can be directly correlated to finger muscle fatigue during SRP. This in-turn may affect the quality and output of dental procedures and also increase the time required for SRP [24]. The current researchers hoped to determine whether a few easy to perform pre-procedural chair side finger stretches could positively affect PS of the finger muscles. Since PS is easily quantified and has a well-developed standardized assessment tool available to measure it, a parallel design study was undertaken to negate carry-over effects. A set of five finger stretches were performed by the test subjects without wearing gloves so as to prevent the resistance provided by them during finger movements. These stretches helped warming up the finger muscles and also increased their range of motion which could in turn increase the efficacy of SRP.
A Jamar® hydraulic pinch gauge was used in this study, as it not only measured the PS, but also indicated overall hand function within a biomechanical frame of reference, inclusive of strength, range of motion and endurance [25]. The validation of pinch gauge was done so as to consistently and accurately provide measurements for the entire sample size. There was no need to calibrate the pinch gauge as it had a correlation of 0.99 reported by the manufacturers [26]. Performance bias was eliminated by training all subjects to maintain the forearm and wrist in neutral position which was checked with goniometer and maintained throughout the testing process.
Dong H et al., evaluated thumb pinch force during SRP using a mounted pinch force censor on the handle of a Gracey no. 11 curette and concluded that a mean pinch force of 35.7±3.8 N was applied by dental students which was greater than the force exerted by the dentist group (24.5±4.1N, p=0.001) [21]. This meant that the students were unable to capably alter pinch force to the useful forces at the instrument tip.
Our study demonstrated that pre procedural finger stretches help in maintaining adequate PS values even after 30 minutes of SRP procedure. A sharp decline in PS was noted for the group that did not perform any finger stretches, which resulted in easy fatiguing of the finger muscles.
A purposive sample of volunteers was used as a study population which resulted in a small sample size. Due to this, the intragroup difference of PS measurements in the Group A achieved statistical significance, although the reduction in PS was bare minimal as compared to the control group, signifying sustenance of PS values.
Further studies with a larger sample size that would increase the statistical power and be representative of age, gender, ethnicity and race more realistically should be undertaken. Also, a qualitative component involving participant’s perception may aid in understanding the effect of pre-procedural finger stretches on PS measurements or lack thereof.
The finger force outputs of older adults tend to have significantly more power at low frequencies and/or are more regular than those of young adults [27]. Thus, a longitudinal study with a larger sample size stratified according to the age of the test subjects would have accurately specified the age related finger muscle fatigue in dental professionals after SRP.
Teaching the biomechanical principles of instrumentation, followed by practical application of the principles at the clinical level, may help lessen the risk for developing musculoskeletal symptoms among dental and dental hygiene students. These may include specific training on reducing peak pinch force during SRP and relaxing the pinch grip between tooth areas. Risk of developing work-related musculoskeletal disorders can be reduced by performing a few simple, non-invasive chair-side stretches coupled with selection of appropriate instruments and modifying work practice by carefully scheduling patients with heavy calculus and taking suitable breaks should be undertaken.
Future Prospects and Author Recommendations
Longitudinal studies with larger sample size stratified according to age would have accurately demonstrated the age related finger muscle fatigue in dental professionals. Output of efficiency of SRP may be evaluated before and after performing finger stretches using debris and calculus indices. Sensitive techniques such as use of a pressure sensor on the instrument grip to evaluate the pinch force can be undertaken. Comparison of pinch strength output by B&L Engineering® pinch gauge (B&L Engineering, Santa Ana, CA, USA) and Jama® hydraulic gauge can be done as B&L Engineering® pinch gauge is the instrument with highest inter-examiner reliability [28].
Conclusion
Thus, within the scope of this study, it can be concluded that the finger muscle fatigue can be decreased by performing a few simple, chair-side finger stretches, preventing the risk of developing musculoskeletal disorders.
PS = Pinch Strength, SRP = Scaling and root planing, lbs = pounds
PS = Pinch Strength, lbs = pounds