Oral Spindle Cell Sarcoma: A Rare Case Report and Review of Literature
Sujatha S Reddy1, Shivani Sharma2, Vijaya Mysorekar3, Pushpanjali Sharma4, Aninditya Kaur5
1 Professor and Head, Department of Oral Medicine and Radiology, Faculty of Dental Science, M.S. Ramaiah University of Applied Sciences, Bengaluru, Karnataka, India.
2 Postgraduate Student, Department of Oral Medicine and Radiology, Faculty of Dental Science, M.S. Ramaiah University of Applied Sciences, Bengaluru, Karnataka, India.
3 Professor, Department of General Pathology, M S Ramaiah Medical College and Hospital, Bengaluru, Karnataka, India.
4 Postgraduate Student, Department of Oral Medicine and Radiology, Faculty of Dental Science, M.S. Ramaiah University of Applied Sciences, Bengaluru, Karnataka, India.
5 Postgraduate Student, Department of Oral Medicine and Radiology, Faculty of Dental Science, M.S. Ramaiah University of Applied Sciences, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sujatha S Reddy, Professor and Head, Department of Oral Medicine, Diagnosis and Radiology, Faculty of Dental Sciences, M.S. Ramaiah University of Applied Sciences, Bengaluru -560054, Karnataka, India.
E-mail: s_sujathajanardhan@yahoo.com
Spindle cell lesions of the head and neck region are diverse in nature by means of clinical and biological heterogeneity. Though few lesions are found to be malignant, several others are benign or merely reactive in nature. Although these lesions are fairly common occurring in other parts of the body, they are very rare in the oral cavity, accounting for less than 1% of all tumours in the oral region. Herein, a case of 48-year-old man who presented with a polypoid lesion of the maxilla has been reported. Histopathological examination and immunohistochemistry revealed spindle cell sarcoma of the left maxillary sinus. We present this rare tumour to contribute to the better understanding and awareness of this rare malignancy where diagnosis can be very challenging.
Cone beam computed tomography, Immunohistochemistry, Malignant, Maxilla, Sinus
Case Report
A 48-year-old male reported with a complaint of a swelling on the left side of the face since a month. Symptoms were progressive, with development of nasal congestion, dull aching left sided facial pain which aggravated on bending the head forward and difficulty in mouth opening. He also gave a history of concomitant use of cigarettes and smokeless tobacco for the last thirty years. Patient was a known Type II diabetic, on insulin therapy for the last three years. On extraoral examination, a well defined, non reducible, non fluctuant swelling was seen on the left cheek, measuring approximately 4×5 cm in size [Table/Fig-1]. It was fixed to the underlying structures, immobile with local rise in temperature. Intraorally in relation to teeth 26, 27, 28 a firm swelling was seen in the sulcus area measuring approximately 4x5.5 cm obliterating the buccal vestibule [Table/Fig-2], perforating the left maxillary buccal cortical plate [Table/Fig-3]. Systemic examination was unremarkable.
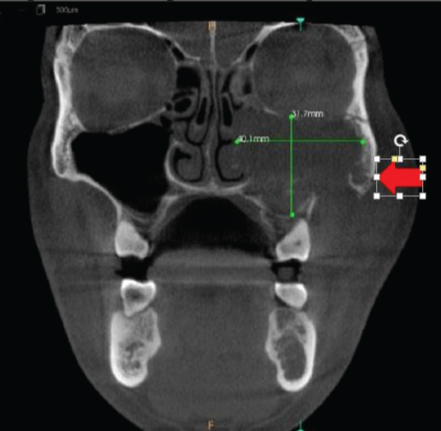
Panoramic radiograph and paranasal sinus view revealed haziness in relation to left maxillary sinus with erosion of lateral and medial sinus wall [Table/Fig-4,5]. CBCT revealed opacification of the left maxillary sinus measuring approximately 31.7 mm (superioinferiorly) x 40.1 mm (mediolaterally) x 37.8 mm (anterioposteriorly) with few areas of calcification. Destruction of left infraorbital margin superiorly, lateral wall of the nasal cavity and ethmoidal air cells medially and lateral and posterior wall of left maxilla was appreciated. The periphery of the lesion was irregular with ill defined non corticated borders [Table/Fig-6]. There was loss of supporting alveolar bone with destruction of lamina dura in relation to teeth 26,27,28. A radiographic diagnosis of malignant neoplasm originating in the left maxillary sinus was given.
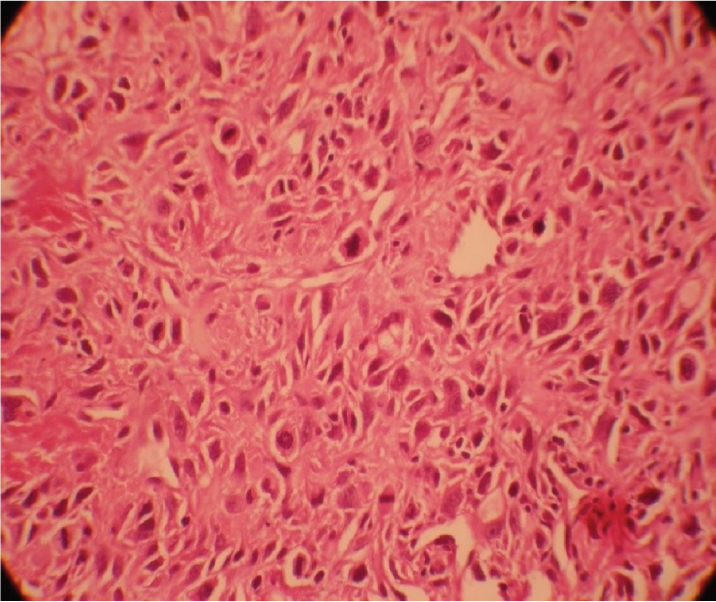
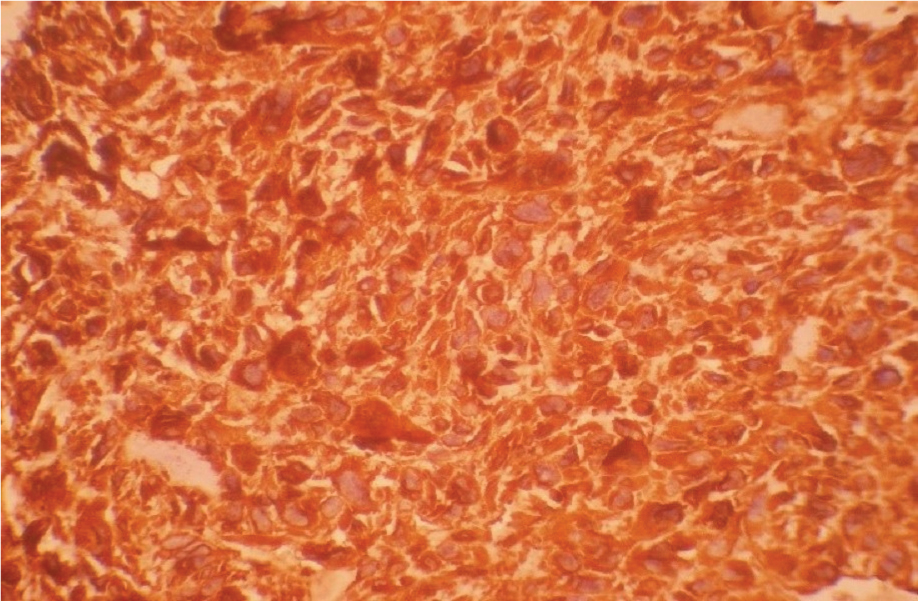
Histopathological examination of intraoral incisional biopsy revealed a highly cellular and vascular connective tissue lesion. Haphazard arrangement of few spindle to round shaped cells, marked cellular and nuclear pleomorphism and hyperchromatic nuclei, increased N:C ratio, multiple nucleoli, numerous abnormal mitotic figures and coarse chromatin were observed which were suggestive of dysplasia. Focal areas of hyalinisation were also noticed. Stroma showed numerous small to large endothelial lined blood vessels with red blood cells suggestive of a spindle cell lesion [Table/Fig-7].
IHC showed strong positivity for vimentin and negativity to pancytokeratin [Table/Fig-8,9]. The patient was diagnosed with spindle cell sarcoma of the left maxillary sinus stage IVA (T4aN0M0). Further IHC analysis with the panel of markers for identification of the type of spindle cell lesion could not be carried out because of the financial constraints. Following the investigations, neo adjuvant chemotherapy followed by left maxillectomy, lymph node dissection, radiotherapy and prosthetic reconstruction was planned. Despite the initiation of treatment, the disease further worsened and the patient died within few days.
Extraoral examination showing well defined swelling on left middle third of the face.

Intraoral examination showing diffused swelling in relation to left maxillary buccal vestibule.
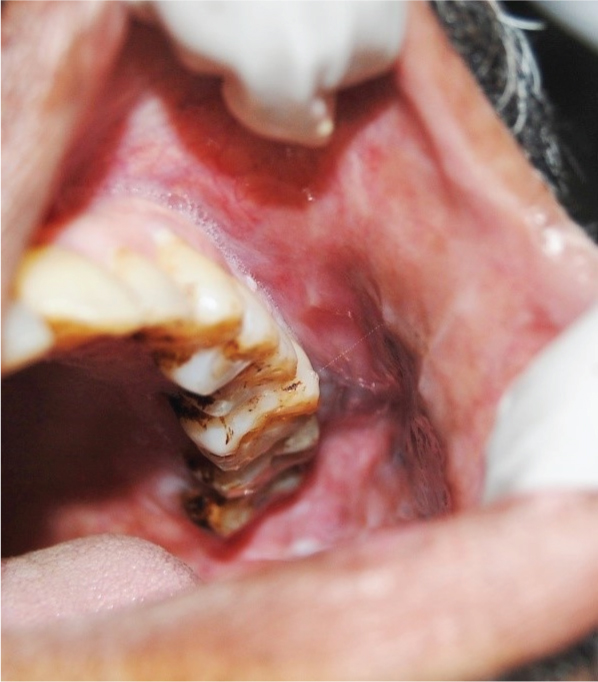
Intraoral examination showing firm, rubbery, and non-tender tissue mass perforating the left maxillary buccal cortical plate.

Panoramic radiograph showing destruction of medial and lateral wall of left maxillary sinus (arrow).

Paranasal sinus view showing haziness with erosion of lateral and medial sinus wall (arrow).

CBCT image showing opacification of the left maxillary sinus and calcifications within the lesion (arrow).
Histopathology revealed a highly cellular, vascular connective tissue lesion with haphazard arrangement of few spindle to round shaped cells (H&E 10 X).
Immunohistochemistry showing pancytokeratin negativity (IHC, 10 X).
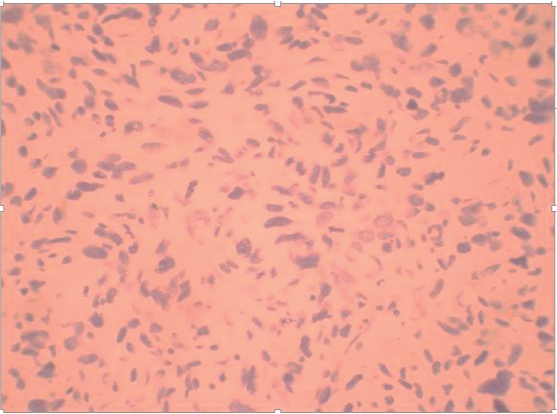
Immunohistochemistry showing vimentin positivity (IHC 40 X).
Discussion
Sarcomas are rare tumours usually heterogeneous by nature, largely originating from the embryonic mesoderm accounting for less than 1% of all head and neck primary cancers [1]. Numerous studies have reported that oral sarcomas represent 0.14%-27.7% of all head and neck cancers suggestive of rarity of the tumour [2-4]. Head and neck primary sarcomas represent about 5% to 15% of all sarcomas among adults and 35% among paediatric population [5].
Tumours of maxillary sinus have a propensity to spread through several routes of the head and neck region. Nasal cavity, ethmoid, orbit, infratemporal fossa, soft tissues of the cheek which erodes the anterior wall, palate, alveolar ridge through the dental foramina and buccal sulcus are the most affected structures of craniofacial region [2]. Oral manifestations of maxillary sinus tumours include diffuse pain in the maxillary teeth which cannot be localized by the patient, trismus, expansion relative to the palate or alveolar ridge, erosion of sinus wall with protrusion into the oral cavity, loose teeth, ill fitting dentures, persistent oroantral fistula, numbness over the hard palate, palsies of ninth and tenth cranial nerve and a palpable mass noticed either in the hard palate, buccal sulcus or anterior antrum. Nasal signs and symptoms include foul smelling nasal discharge, epistaxis, stuffiness and congestion. Ocular symptoms include diplopia, unilateral tearing, and fullness of lids, orbital pain and also exophthalmos. Facial symptoms include paraesthesia over the infraorbital nerve, swelling and pain over cheek and facial asymmetry as seen in our case [1,3]. This case is presented for its uniqueness of occurrence at a comparatively younger age, site and aggressive nature of presentation.
Soft tissue spindle cell neoplasms encompass a varied group of benign and malignant tumours, including those of neural, fibroblastic, vascular, myofibroblastic, myogenic, and epithelial origins. Head and neck tumours composed of predominantly spindle cells may exhibit the following histological patterns: monomorphic (‘fibrosarcoma-like’), biphasic, pleomorphic Malignant Fibrous Histiocytoma (MFH- like) or myxoid [6]. Histopathology is significant in categorising the differential diagnosis of this lesions allowing more targeted use of immunohistochemistry and molecular techniques. The immunohistochemical diagnosis is reported to narrow down by including a larger panel of antibodies, however; cost restraints bound the number of antibodies that can be subjected in each case [7].
Vimentin a type III Intermediate Filament (IF) protein is present in many different neoplasms but is particularly expressed in those originated from mesenchymal cells. Vimentin is often included in the primary panel along with CD45, cytokeratin, and S-100 protein. Intense staining reaction for vimentin without coexpression of other intermediate filament proteins is strongly suggestive of a mesenchymal tumour. In our patient, intense vimentin positivity was observed which is suggestive of a sarcoma [7].
Amongst these patients a relative five year survival rate is around 50% conferring to statistics from the National Cancer Institute [4]. All cases should be treated aggressively with surgical therapy has been the mainstay in the management (maxillectomy with lymph node dissection), and adjuvant (chemo) radiotherapy should be considered in patients with high risk behaviour. Whole tumour removal e.g., total maxillectomy may produce poor cosmetic and functional results due to its vicinity to vital structures [1]. Since spindle cell sarcomas of the head and neck region are a rare entity, evidence of optimal management is lacking. Head and neck sarcomas have poor prognosis as compared to other body sites [1,7]. However, despite efforts at early initiation of therapy our patient couldn’t survive because of the aggressive nature of the disease. Multidisciplinary approach of these cases is essential for proper treatment planning with minimal functional and cosmetic deficits as result of treatment. The advanced molecular biology studies are very promising for the future research which can have an influential role on early diagnosis and prognosis of maxillofacial sarcomas [8,9].
Conclusion
Oral spindle cell neoplasms are potentially aggressive with a tendency to recur and metastasize and have an unpredictable biological behaviour with poor prognosis. It can be fairly challenging to diagnose through routine histopathology and requires judicious use of immunostains which aid in reigning out specific neoplasms.
[1]. A Srivastava, A Ghosh, S Saha, VP Saha, D Chakraborty, Sarcomas of head and neck – A 10 yrs experienceIndian J Otolaryngol Head Neck Surg 2007 59:322-26. [Google Scholar]
[2]. M Gorsky, JB Epstein, Head and neck and intra-oral soft tissue sarcomasOral Oncol 1998 34:292-96. [Google Scholar]
[3]. CB Lajer, S Daugaard, HS Hansen, J Kirkegaard, S Holmgaard, ME Christensen, Soft tissue sarcomas of the head and neck: A single-centre experienceClin Otolaryngol 2005 30:176-82. [Google Scholar]
[4]. N Penel, C Van Haverbeke, E Lartigau, MO Vilain, J Ton Van, Y Mallet, Head and neck soft tissue sarcomas of adult: Prognostic value of surgery in multimodal therapeutic approachOral Oncol 2004 40:890-97. [Google Scholar]
[5]. G Lahat, A Lazar, D Lev, Sarcoma epidemiology and etiology: Potential environmental and genetic factorsSurg Clin N Am 2008 88:451-81. [Google Scholar]
[6]. T Shamim, The spindle cell neoplasms of the oral cavityIranian Journal of Pathology 2015 10(3):175-84. [Google Scholar]
[7]. MA Tejani, TJ Galloway, M Lango, JA Ridge, M von Mehren, Head and neck sarcomas: A comprehensive cancer center experienceCancers 2013 5:890-900. [Google Scholar]
[8]. MM Chidzonga, L Mahomva, Sarcoma of the oral and maxillofacial region: A review of 88 cases in ZimbabweBritish Journal of Oral and Maxillofacial Surgery 2007 45(4):317-18. [Google Scholar]
[9]. AS Aljabab, RW Nason, R Kazi, KA Pathak, Head and neck soft tissue carcinomaIndian J Surg Oncol 2011 2(4):286-90. [Google Scholar]