Membranous Basal Cell Adenoma – A Rare Entity in an Unusual Location
Nadeem Jeddy1, Lakshmipathy Prasannamoorthy2, Rooban Thavarajah3, T Radhika4, Aarthi Ramachandran5
1 Professor and Head, Department of Oral Pathology and Microbiology, Thai Moogambigai Dental College and Hospital, Chennai, Tamil Nadu, India.
2 Professor, Department of Orthodontics, Tagore Dental College, Chennai, Tamil Nadu, India.
3 Professor, Department of Oral Pathology and Microbiology, Ragas Dental College, Chennai, Tamil Nadu, India.
4 Reader, Department of Oral Pathology and Microbiology, Thai Moogambigai Dental College and Hospital, Chennai, Tamil Nadu, India.
5 Postgraduate Student, Department of Oral Pathology and Microbiology, Thai Moogambigai Dental College and Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Aarthi Ramachandran, 1857, 17th Street, I-Block, Thiruvalluvar Kudiyirupu, Anna Nagar, Chennai-600040, Tamil Nadu, India.
E-mail: artiramvi@yahoo.co.uk
Basal cell adenoma is a rare benign salivary gland neoplasm exhibiting an isomorphic basaloid tumour cell pattern, commonly occurring in the parotid. Membranous variant warrants separate consideration because of its recurrence and rate of malignant transformation. We report a case of membranous type basal cell adenoma occurring in minor salivary gland in a 61-year-old female patient. The histopathological diagnosis was supported by immunohistochemical analysis and serum Carcinoembryonic antigen level.
Buccal mucosa, Minor salivary gland neoplasm, Monomorphic adenoma
Case Report
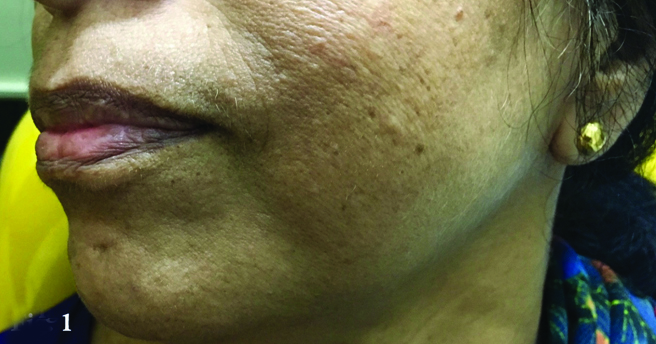
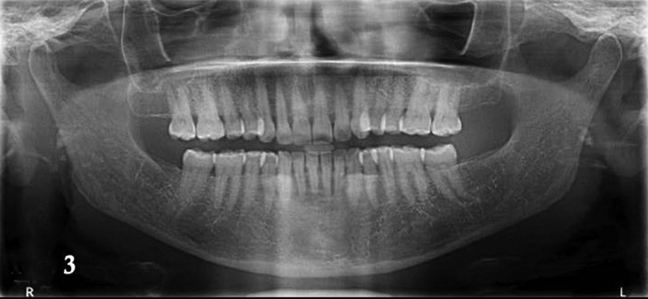
A 61-year-old female patient presented to a private dental clinic with a painless growth on the left buccal mucosa. The swelling was insidious in onset and gradually attained the present size of 3x2 cm in its largest dimension in a duration of six months. Clinical examination did not reveal any extraoral swelling or lymphadenopathy [Table/Fig-1]. A smooth surfaced, ovoid mass which did not show any colour change was appreciated intraorally on the left posterior buccal mucosa in relation to teeth #37 and 38; extending anteroposteriorly from the distal aspect of tooth #37 to the retromolar area and superoinferiorly from mandibular buccal sulcus to a level of 4 mm above the line of occlusion. The swelling was firm, non tender and mobile on palpation [Table/Fig-2]. Orthopantomogram ruled out bony involvement suggestive of a non invasive soft tissue lesion [Table/Fig-3]. Negative pressure was elicited on aspiration, which was suggestive of a solid lesion. Based on the clinical features, a provisional diagnosis of benign salivary gland neoplasm was made. While mesenchymal tumour of vascular, smooth muscle or neural origin was considered as differential diagnosis.
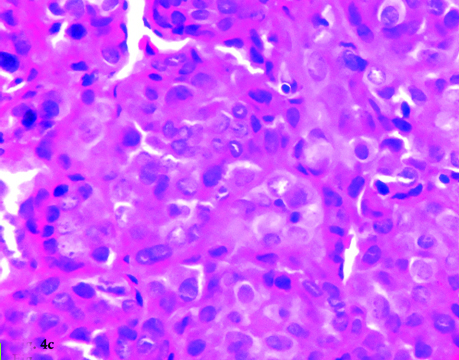
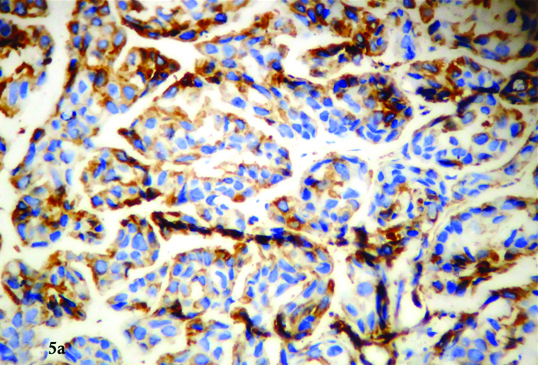
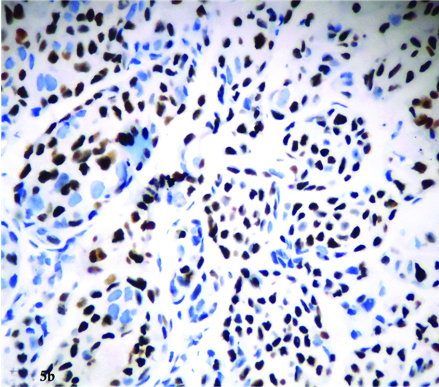
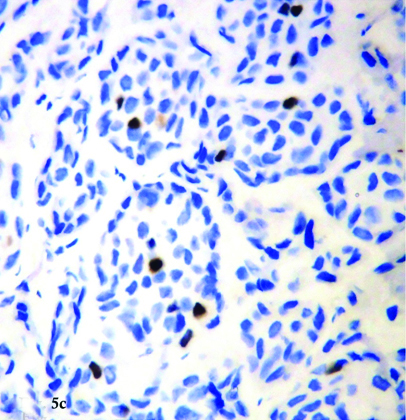
Incisional biopsy was done under local anaesthesia and the specimen was subjected to histopathological examination. The haematoxylin and eosin stained sections revealed nests of basaloid cells surrounded by thick, eosinophilic hyaline layer [Table/Fig-4a,b]. The cell nests consisted of peripheral small, hyperchromatic cuboidal basal cells with central large, round and pale staining nuclei [Table/Fig-4c]. The microscopic features were suggestive of basal cell adenoma- membranous type. To further substantiate our diagnosis, the sections were subjected to Immunohistochemical analysis (IHC), which revealed strong positivity for vimentin and p63. Ki-67 index was low (3%) indicating a non malignant lesion [Table/Fig-5a,b,c]. Further, the blood level of Carcinoembryonic antigen was also investigated and found to be 1.6 ng/ml, confirming the benign nature of the tumour. Based on these findings a final diagnosis of basal cell adenoma was made. Wide surgical excision of the tumour was planned, however, the patient was lost to follow up.
Extraoral photograph of the patient.
Intraoral photograph showing swelling on the left buccal mucosa.

Orthopantamograph indicating absence of bone involvement.
Islands of basaloid cells separated by basement membrane (Haematoxylin and eosin, 10X).
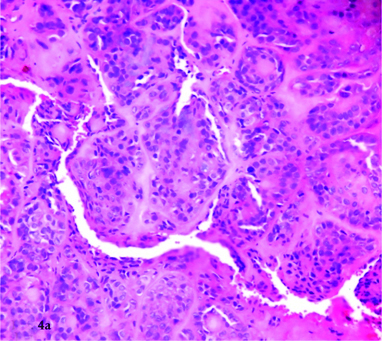
Islands of basaloid cells separated by basement membrane (Haematoxylin and eosin, 20X).
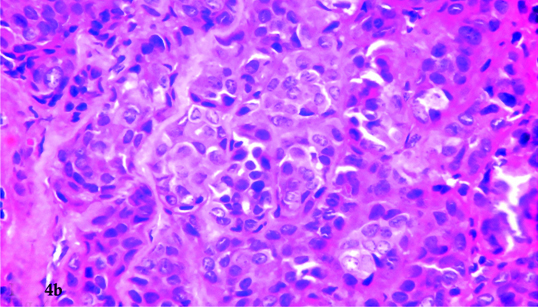
Peripheral hyperchromatic basal cells and central large, pale staining nuclei (Haematoxylin and eosin, 40X).
Photomicrograph exhibiting IHC positivity for vimentin.
Photomicrograph exhibiting IHC positivity for p63.
Photomicrograph exhibiting Ki-67 labelling index - 3%.
Discussion
Salivary gland tumours are a complex, heterogenous group of neoplasms constituting 2-6% of head and neck tumours, majority of which occurs in the major salivary glands [1]. Basal Cell Adenoma (BCA) is an uncommon benign salivary gland neoplasm accounting for just 1-2% of salivary gland tumours. It has an incidence of 9-23% in minor salivary glands [2]. The nomenclature has been inconsistent in history. This tumour was classified under Monomorphic adenomas because of its uniform basaloid appearance. It was only in 1967, that Kleinsasser and Klein suggested the use of the term “Basal cell adenoma” and described it as a separate entity. The first case of BCA in literature was reported by Batsakis in 1972 [3]. Parotid gland is the most common site of occurrence (75%) followed by upper lip, palate and buccal mucosa [4].
Basal Cell Adenoma has been defined by the World Health Organization as a benign epithelial neoplasm of isomorphic basaloid cells arranged with a noticeable basal cell layer and a distinct basement membrane like structure. Myxochondroid stromal component that is characteristic of mixed tumour is absent [4].
Histologically, four subtypes have been identified and described by Ellis and Gnepp-solid, tubular, trabecular and membranous [4]. Membranous type is a rare hereditary variant and was designated as “Dermal analogue tumour” by Batsaki and Brannon, exhibiting characteristic clinical and histologic features and a high recurrence rate thereby warranting special consideration. The membranous BCA has been frequently found associated with dermal cylindromas and with trichoepitheliomas in one third of cases [5]. Multiple cutaneous adnexal tumours with synchronous salivary gland BCA are a feature of Brooke-Spiegler syndrome. It is an autosomal dominant condition caused by mutation of tumour suppressor gene which encodes for CYLD protein [5]. No dermal lesions were evident in our case.
The membranous variant has shown male preponderance in various studies, especially in the study by Luna MA et al., [6]. In contrast to the reviews, our patient was a 61-year-old female. This tumour can arise at any age but shows peak incidence in the sixth decade of life, as in our case [5]. The lesion was unilateral, ovoid and smooth surfaced and presented on the buccal mucosa with only 5.5% incidence quoted in literature in that location [7].
Microscopic findings of BCA reveals fairly uniform and regular appearing basal cells of two morphologic types: small cells with rounded basophilic nucleus and scanty cytoplasm and large cells with ovoid, pale staining nucleus and abundant cytoplasm. The membranous variant is distinct from other subtypes: it is un-encapsulated, multilobulated with jigsaw arrangement of epithelial islands surrounded by thick, eosinophilic hyaline layer. The neoplastic cells are sharply demarcated from the surrounding stroma. Ultrastructural studies by Hemachandran M et al., revealed that the hyaline layer represents reduplicated basement membrane [8]. It is important to rule out other tumours which are clinically and histopathologically similar to BCA as they are prognostically distinct. The lack of chondromyxoid stroma and the presence of distinctive basal membrane in BCA help to rule out pleomorphic adenoma [4]. The absence of infiltrative growth pattern, perineural invasion and mitotic activity aids in differentiating BCA from adenoid cystic carcinoma and basal cell adenocarcinoma.
Although histopathological examination has been acknowledged as a gold standard, IHC has been used as an adjunct in diagnosis. Intense expression of p63 suggests the predominance of basal/ stem cells of stratified epithelium and myoepithelial cells. This finding is consistent with the findings reported by Edward PC et al., [9]. The presence of focal staining of Ki-67 (<3%) confirms the benign nature of the lesion [9].
Management of the lesion can be achieved by local excision exhibiting negative surgical margin. Although recurrence is rare in BCA, the membranous variant shows a recurrence rate of 25-37%, which may largely be attributed to its multifocal nature rather than a true recurrence. Malignant transformation rate of 4.3% has been reported for membranous basal cell adenoma [10]. With a wide excision and periodic follow up, the prognosis is good.
Conclusion
There have been very few cases of membranous basal cell adenoma reported in literature. Majority of monomorphic adenomas exhibit a non aggressive behaviour and can be adequately treated with simple excision. Membranous variant is a rare subtype with increased propensity for recurrence and malignant transformation. Early and prompt diagnosis, appropriate treatment and long term follow up is essential for good prognosis.
[1]. AB Karim, L Sumarriva, A Sharabi, T Kasahara, Basal cell adenoma of the upper lip: A case reportJ Dent Health Oral Disord Ther 2015 2(4):00058 [Google Scholar]
[2]. SP Sodhi, RS Brar, HP Singh, T Kaur, R Dhawan, A rare occurrence of basal cell adenoma of palate: A case report with comprehensive immunohistochemical analysisJ Can Res Ther 2015 11:1023 [Google Scholar]
[3]. JG Batsakis, Basal cell adenoma of the parotid glandCancer 1972 29(1):226-30. [Google Scholar]
[4]. AB Yadav, A Narwal, A Devi, S Kumar, SK Yadav, Basal cell adenoma of palate, a rare occurrence with review of literatureJ Dent Shiraz Univ Med Sci 2015 16(3):291-95. [Google Scholar]
[5]. GL Ellis, PL Auclair, DR Gnepp, Textbook of Surgical Pathology of the Salivary Glands 1991 25:202-23. [Google Scholar]
[6]. MA Luna, JG Batsakis, E Tortoledo, GW del Junco, Carcinoma ex monomorphic adenoma of salivary glandsJ Laryngol Otol 1989 103(1):756-59. [Google Scholar]
[7]. ADB Singh, S Majumdar, A Ghosh, L Gandi, Basal cell adenomaclinicopathological, immunohistochemical analysis and surgical considerations of a rare salivary gland tumour with review of literatureNiger J Surg 2015 21(1):31-34. [Google Scholar]
[8]. M Hemachandran, A Lal, F Vaiphei, Basal cell adenoma- an unusual presentationAnn Diag Pathol 2003 7(5):292-95. [Google Scholar]
[9]. PC Edward, T Bhuiya, RD Kelsch, Assessment of p63 expression in the salivary gland neoplasms adenoid cystic carcinoma, polymorphous low-grade adenocarcinoma, and basal cell and canalicular adenomasOral Surg Oral Med Oral Pathol Oral Radiol Endod 2004 97(5):613-19. [Google Scholar]
[10]. PA Bhagde, SR Barpande, JD Bhavthankar, JG Humbe, Basal cell adenoma of maxillary sinus mimicking ameloblastomaJ Oral Maxillofac Pathol 2016 20:142-46. [Google Scholar]