Leprosy in an Eight-Year-Old Child – An Exceptional Case with Unusual Oral Manifestation
Mayuri Jain1
1 Senior Lecturer, Department of Oral Medicine and Radiology, Maharana Pratap College of Dentistry and Research Centre, Gwalior, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mayuri Jain, D-38, Lotus villa, Ohadpur, Alkapuri, City Centre, Gwalior, Madhya Pradesh, India.
E-mail: dr.mayurijain@gmail.com
Leprosy is a contagious and granulomatous disease which is caused by Mycobacterium leprae. The incubation period for leprosy is five to seven years and it can take as long as about 30 years before signs and symptoms of leprosy develop in some patients. It is a chronic systemic disease which mostly affects the skin and peripheral nerves. It has been seen that indeterminate leprosy is the most common type seen in childhood followed by tuberculoid variant. Borderline lepromatous and lepromatous leprosy are only occasionally encountered in children and rarely affects the oral cavity. Here, we report a rare case of an eight-year-old female child patient who presented primarily with oral manifestations and was subsequently diagnosed as having lepromatous leprosy
Lepromatous leprosy, Mycobacterium leprae, Skin biopsy
Case Report
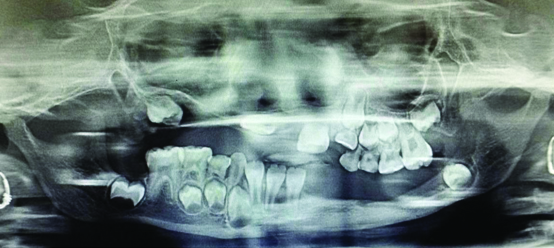
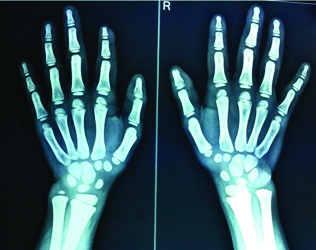
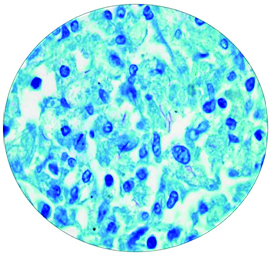
An eight-year-old female child patient reported to the Department of Oral Medicine and Radiology with a chief complaint of missing teeth in upper and lower jaws since 5 years. Patient also reported difficulty in chewing. Patient complained of slight tingling sensation in the lower extremities. Patient had not taken any treatment for the condition. There was known family contact history, in which the patient’s grandmother and others siblings suffered from leprosy, all these relatives were still alive and staying under the same roof. On general physical examination, the patient had frontal bossing with thick everted lips [Table/Fig-1]. Hair was fine and brittle, no changes were found in the body hair. Her skin was dry, pale and sclerotic. Nails were hypoplastic and bulbous. All vital signs were within normal limits. Extra oral examination revealed a single hypo pigmented skin coloured macular lesion on the forehead [Table/Fig-1] and single asymptomatic lesion at the tip of first finger of left hand [Table/Fig-2]. There was evidence of facial asymmetry due to deviation on left side, saddle nose, and corneal opacity [Table/Fig-1]. Right submandibular lymph nodes were palpable which was about 1 cm to 2 cm in size, firm in consistency, mobile & non tender. There was sensory loss and motor weakness present in the lower right limb. Intra oral examination revealed non scrapable white patch on dorsal surface of tongue, size approximately 1 cm x1 cm [Table/Fig-3]. Her dental health was very poor and revealed multiple carious and missing teeth [Table/Fig-4]. After clinical examination patient was advised for Mantoux and Lepromin skin test which were negative. Based on history and clinical appearance of the lesion, a provisional diagnosis of granulomatous disease (tuberculosis/leprosy) was hypothesized. Differential diagnosis of the lesion included ectodermal dysplasia, syphilis, sarcoidosis and systemic lupus erythematosus. Heamogram of the patient revealed mild anemia (Hb =8.3 gm%), red blood cells series shows mild to moderate microcyte, hypochromic and severe anisocytosis cells, white blood cells shows eosinophilia (19%) and raised erythrocyte sedimentation rate (ESR = 55 mm in the first hour). In radiological investigation, orthopantomogram revealed multiple missing primary teeth (52,53,54,55,72,73,74.75) and permanent tooth buds (12,13,14,15,17,32,33,34,35,36) in maxillary and mandibular arches [Table/Fig-5]. Lateral cephalogram revealed atrophy of nasal septum leading to flatness of nasal cartilage and curvature of cervical spine [Table/Fig-6]. Hand wrist radiograph showed bone erosion at the tip of first finger of left hand and on the tip of thumb region of right hand [Table/Fig-7]. Chest X-ray did not reveal any significant finding. Smear from the lesion (dorsal surface of the tongue) revealed bacteriological index of 4+ along with morphological index of 10%. An incisional biopsy of the lesion (dorsal surface of the tongue) revealed numerous acid fast bacilli. Fite-Faraco staining showed the numerous leprosy bacilli appearing as a slender rod, within the macrophages and confirmed the diagnosis of leprosy [Table/Fig-8]. The patient was referred to the dermatologist where she was started on multidrug therapy which included 50 mg of dapsone daily and 300 mg of rifampicin monthly along with 50 mg of clofazimine daily. The lesions subsided in six to eight weeks time, with no evidence of recurrence on follow up. The patient is under multidrug therapy from past 11 months.
Extraoral photograph showing frontal boosing, hypopigmented macule on the fore head, saddle nose, corneal opacity and thick everted lips.

Photograph showing single asymptomatic lesion at the fingertip.

Intraoral photograph showing white patch (size 1 cm x1 cm) on dorsum surface of tongue.

Intraoral photograph showing upper right central incisor impinging on upper labial mucosa.

Orthopantomogram showing missing of primary teeth and permanent tooth bud in maxillary right and mandibular left quadrant.
Lateral cephalogram showing atrophy of nasal septum which may leads to flatness of nasal cartilage and curvature of cervical spine.

Hand wrist radiograph showing bone erosion at the tip of first finger in left side and on the tip of thumb region on right side.
Photomicrograph of the lesion showing numerous acid fast bacilli within macrophages (Fite-Faraco stain; magnification X 40).
Discussion
Leprosy is a foremost health problem in India. According to National Leprosy Eradication Programme (NLEP), the proportion of new childhood cases has been around 9% - 13,387 (9.6%) in 2012- 2013 to 12043 (9.4%) in the year 2013-2014 [1]. It is an indolent chronic infectious diseases caused by Mycobacterium leprae (Hansen’s bacillus). It is a granulomatous disease of peripheral nerves, skin and sometimes other tissues. The upper airways are the most important point of entry for bacillus and a chief source for bacillary elimination in leprosy. It affects all age groups from infancy to old age. It has a long incubation period and is transmitted from one person to other. The disease presents polar clinical forms, the first, tuberculoid leprosy (paucibacillary) that is characterized by high immune reaction to the organism. The second, lepromatous leprosy (multibacillary; LL), that usually develops in patients with reduced cell mediated response. Within this spectrum there are borderline and less common variations with intermediate lesions [2]. However, it has generally been observed that lepromatous leprosy is only occasionally encountered in childhood [3]. The main clinical features of leprosy are erythematous or hypopigmented macules on the skin surface with reduced sensation, distinct sensory loss with peripheral nerve involvements and muscle weakness. Diagnosis is fundamentally based on clinical suspicion and epidemiological findings, obtained by a detailed patient’s history, living conditions and skin and neurological examination. If not diagnosed early, leprosy can lead to severe disfigurement and disability [4]. The clinical signs and symptoms of leprosy are often not easy to recognize in children, but due to the high probability of physical deformity, social and psychological issues, it entails cannot be neglected [5]. Common sites of involvement include face, back, abdomen, buttocks, and extremities [6]. The children present with asymptomatic or hypoaesthetic cutaneous lesions and, less often, with neural manifestations. But in our case, neural manifestation was there. Involvement of oral mucosa may have a key role in leprosy transmission from adults to children [7]. The oral manifestations are usually rare in leprosy patients but in present case along with cutaneous lesion, oral manifestations were also present. Prabhu SR and Daftary DK in an excellent review of 700 leprosy patients reported that the prevalence of oral involvement in leprosy was 11.5% [8]. Other authors such as Motta AC et al., Soni NK and Palaskar S reported that the oral lesions usually appear in the advanced stage of leprosy [9-11]. From the clinical point of view, the larger evidence of the pathology appears in the nasal bones or nasal spine. There may be destruction of the premaxilla and loss of teeth as we seen in present case. In recent studies, it has been seen that nasal mucosa becomes more affected than oral mucosa and may be a site of M. leprae infection and transmission [12,13]. Definitive diagnosis of leprosy can be confirmed by histopathological examination. This case is unique because after analysing history, clinical appearance and oral manifestations diagnosis of lesion was considered a leprosy which is one of the rarest diagnoses in children.
Conclusion
In conclusion, examination of leprosy patients should be extended to the oral mucosa because oral mucosa may be a secondary source of M. leprae transmission and infection. This case is being reported to create awareness and to highlights the rarity or unusual clinical presentation of leprosy.
[1]. AJ Asia, V Tapre, U Joge, Profile of childhood leprosy cases attending a tertiary care centreIndian J Lepr 2016 88:111-16. [Google Scholar]
[2]. H Ahmad, Oral manifestation of leprosy: a reviewJournal of dental and medical sciences 2015 14(6):77-79. [Google Scholar]
[3]. VN Sehgal, A Chaudhary, Leprosy in children: a prospective studyInt J Dermatol 1993 32:194-97. [Google Scholar]
[4]. MP Amador, VR Barros, PJ Albuquerque, MI Buna, JM Campos, Childhood leprosy in the Curionopolis district – South-eastern Para state – a case reportHansen Int 2001 26:121-25. [Google Scholar]
[5]. IN Ferreira, RR Alvarez, Leprosy in patients under fifteen years of age in the city of Paracatu - MG (1994 to 2001)Rev Bras Epidemiol 2005 8:41-49. [Google Scholar]
[6]. VN Sehgal, G Srivastava, Histoid leprosy A reviewInt J Dermatol 1985 24(1):286-92. [Google Scholar]
[7]. AK Boggild, JD Correia, JS Keystone, KC Kain, Leprosy in Toronto: an analysis of 184 imported casesCMAJ 2004 170:55-59. [Google Scholar]
[8]. SR Prabhu, DK Daftary, Clinical evaluation of oro-facial lesions of leprosyOdontostomatol Trop 1981 4:83-95. [Google Scholar]
[9]. AC Motta, MC Komesu, CH Silva, D Arruda, JC Simao, EM Zenha, Leprosyspecific oral lesions: a report of three casesMed Oral Patol Oral Cir Bucal 2008 13:E479-82. [Google Scholar]
[10]. NK Soni, Leprosy of the tongueIndian J Lepr 1992 64:325-30. [Google Scholar]
[11]. S Palaskar, Histopathological study of apparently normal oral mucosa in lepromatous leprosyIndian J Dent Res 2005 16:12-14. [Google Scholar]
[12]. TS Martinez, MM Figueira, AV Costa, MA Gonçalves, LR Goulart, IM Goulart, Oral mucosa as a source of Mycobacterium leprae infection and transmission, and implications of bacterial DNA detection and the immunological statusClin Microbiol Infect 2011 17:1653-58. [Google Scholar]
[13]. MA De Abreu, NS Michalany, LL Weckx, DR Neto Pimentel, CH Hirata, MM de Avelar Alchorne, The oral mucosa in leprosy: a clinical and histopathological studyBraz J Otorhinolaryngol 2006 72:312-16. [Google Scholar]