Successful Surgical Outcome for an Endodontic Failure using BiodentineTM as Retrograde Restoration in Conjunction with Platelet Rich Fibrin (PRF) for Progressive Healing
Ajinkya Mansing Pawar1, Suraj M. Pawar2, Bhagyashree Thakur3, Sharad Kokate4
1 Assistant Professor, Department of Conservative Dentistry and Endodontics, Nair Hospital Dental College, Mumbai, Maharashtra, India.
2 Oral Surgeon, Department of Dentistry, Sunny Medical Centre LLC, Shahba, Sharjah, United Arab Emirates.
3 Clinical Assistant, Department of Dentistry, Sir H N Reliance Foundation Hospital, Mumbai, Maharashtra, India.
4 Dean and Professor, Department of Conservative Dentistry and Endodontics, YMT Dental College and Hospital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ajinkya Mansing Pawar, Y-10/155, Government Colony, Bandra East, Mumbai-400051, Maharashtra, India.
E-mail: ajinkya@drpawars.com
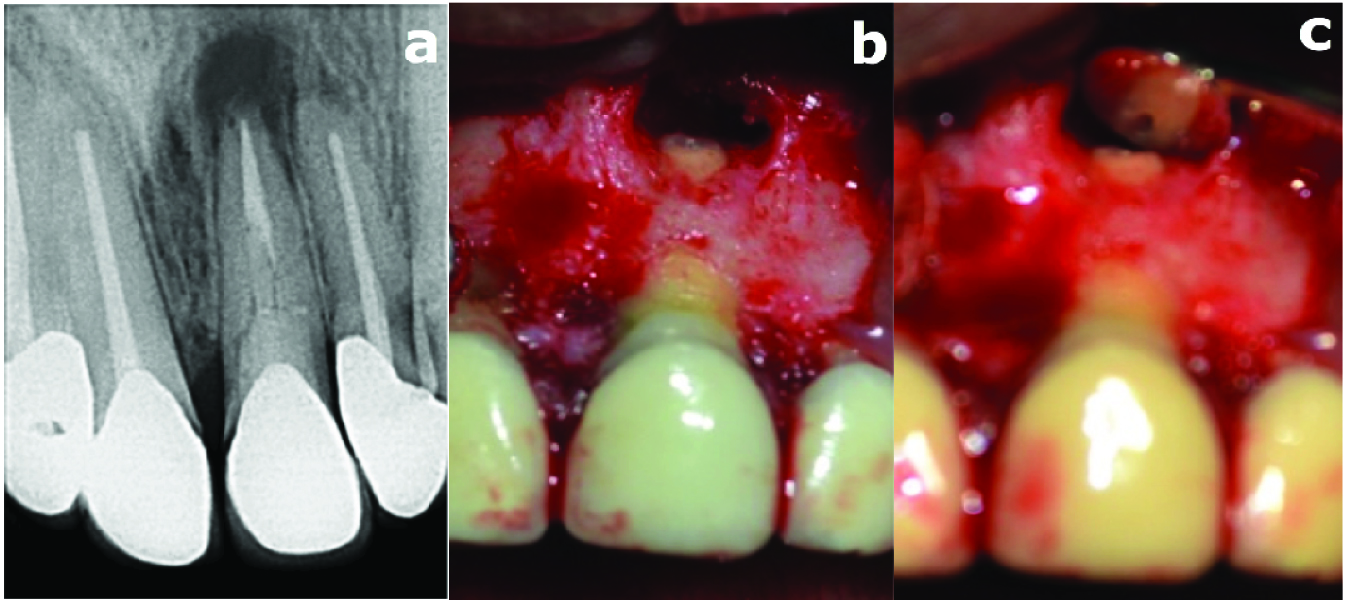
Apical surgery, Regeneration, Retreatment
A healthy 32-year-old male patient was referred to the Department of Conservative Dentistry and Endodontics with a chief complaint of pain in the previously treated anterior tooth. The patient gave a history of endodontic treatment for the anterior teeth three years back and experienced intermittent pain for the past three months. Medical history was non contributory and clinical examination revealed bilaterally restored maxillary central and lateral incisors with porcelain fused to metal crown. Radiographic examination revealed intracanal fillings/obturations with respect to the maxillary right and left (restored with a fiber post) central incisors and associated periapical radiolucency [Table/Fig-1a]. The patient was not willing to replace it and the patient being in merchant navy was time constrained, refused retreatment. The preoperative radiograph showed acceptable obturation with a bonded fiber post used as an intracanal restoration. It was difficult to retrieve, and the trial to retrieval may lead to other complications like perforation hence, a periapical surgery was scheduled.
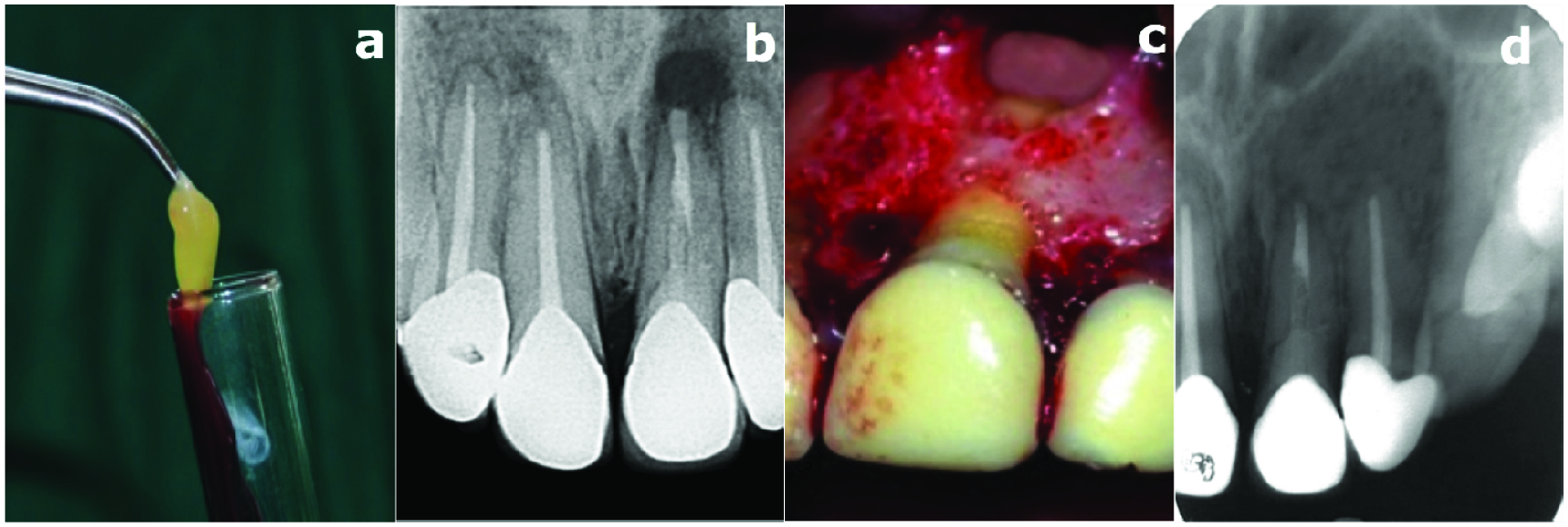
The periapical pathosis was enucleated raising a double vertical trapezoidal flap [1]. Maxillary left central incisor was apically resected 3 mm from the apex; retrograde cavity of 3 mm was prepared using ultrasonic retro tips [Table/Fig-1b,c]. Platelet Rich Fibrin (PRF) preparation was done by protocol developed by Choukroun J et al., (see below [Table/Fig-2a]) [2]. This was followed by placement of Biodentine™ retrograde plug of 3 mm, which was confirmed by a radiograph [Table/Fig-2b], and the placement of prepared PRF graft into the bone cavity [Table/Fig-2c]. The surgical site was then sutured and the enucleated lesion was sent for histopathological diagnosis. For suture removal and postsurgical assessment the patient was recalled after a week. The patient returned after eight months and the follow up X-ray taken at that time showed complete healing of the periapical lesion [Table/Fig-2d].
The failure of endodontic treatment occurs, when the protocol followed is insufficient acceptable standards. Scientific evidence indicates that some factors like; microbial (extraradicular and/or intraradicular infections), non-microbial (intrinsic/extrinsic), may be associated with the unsatisfactory outcome of well-treated cases [3]. The tooth in question being restored with a bonded fiber post, which is difficult to retrieve, and the patient being time constrained, the decision was taken for an apical surgery instead of retreatment.
After a peri radicular surgery, bone regeneration depends on primary closure, radicular angiogenesis, source of undifferentiated mesenchymal cells, space maintenance and stability (PASS) principle [4]. The present case report explains the advantageous clinical efficacy of PRF when used as a graft while treating an intra bony defect. The autologous PRF is embedded with good quantities of platelet and leukocyte cytokines as a result of centrifuging the patient’s whole blood. These incorporated cytokines are released over a time period of 7-11 days, which has an added effect on wound healing [5,6].
While using PRF [1], the PRF membrane maintains and protects the grafted biomaterials and PRF fragments serve as biological connectors between bone particles [2]. The integration helps in cellular migration (specially endothelial cells), important for the neo-angiogenesis, vascularization and survival/success of the graft [3]. Platelet cytokines; PDGF, TGF- α, IGF-1, are slowly released as the fibrin matrix is resorbed, creating a steady progress in healing [4]. Presence of leukocytes and cytokines plays a vital role in the self regulation of inflammatory and infectious phenomena [7].
PRF membrane functions as a “biological connector” between the different elements of graft and acts as a matrix, which supports capture of stem cells and migration cells to center of the graft [7]. The clinical and radiographic criteria are the basis to conclude the success and failure of a periradicular surgery. Post periradicular surgery, the patient showed gradual healing and improved status of the supporting structures. The positive effect of PRF was clearly observed in the follow up radiograph taken just after eight months.
Biodentine is a substitute to the well-established root end retrograde filling material Mineral Trioxide Aggregate (MTA). Both the materials are similar in basic composition except for the addition of setting accelerator i.e., calcium chloride in the liquid component of Biodentine. Also, the initial setting time of Biodentine is 10-12 minutes whereas, for MTA its 2 hours 45 minutes. Kokate SR and Pawar AN have demonstrated bidentine to be an effective alternative to MTA as a root end filling material [8]. The elemental uptake into dentine was more prominent for biodentine than for MTA [1]. Hence, biodentine was used in the present case for its merits over MTA as a root end filling material.
From the presented case it can be concluded that PRF is efficacious clinically and radiographically in management of intrabony defect in an endodontically failed tooth surgically intervened in conjunction with biodentine when used as retrograde filling material.
a) Preoperative radiograph presenting periapical lesion with previously endodontically treated tooth #21 restored with bonded quartz fiber post; b) Apical 3mm resection and periapical curettage for removal of the periapical pathosis with tooth #21; c) Retrograde cavity of 3mm for placement of retrograde filling..
a) Platelet Rich Fibrin prepared; b) Radiograph confirming the placement of the retrograde filling of BiodentineTM of 3mm; c) Placement of PRF as a graft in the bone cavity; d) Eight month follow-up radiograph showing healed periapical lesion.
[1]. AM Pawar, SR Kokate, RA Shah, Management of a large periapical lesion using Biodentine TM as retrograde restoration with eighteen months evident follow upJ Conserv Dent 2013 16:573-75. [Google Scholar]
[2]. J Choukroun, A Diss, A Simonpieri, MO Girard, C Schoeffler, SL Dohan, Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part V: Histologic evaluations of PRF effects on bone allograft maturation in sinus liftOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101:299-303. [Google Scholar]
[3]. JF Siqueira, Aetiology of root canal treatment failure: why well-treated teeth can failInt Endod J 2001 34:01-10. [Google Scholar]
[4]. HL Wang, L Boyapati, “PASS” principles for predictable bone regenerationImplant Dent 2006 15(1):08-17. [Google Scholar]
[5]. A Simonpieri, M Del Corso, G Sammartino, DM Dohan Ehrenfest, The relevance of choukroun’s platelet-rich fibrin and metronidazole during complex maxillary rehabilitations using bone allograft. part I:M a new grafting protocolImplant Dent 2009 18:102-11. [Google Scholar]
[6]. RE Marx, ER Carlson, RM Eishstaed, SR Schimmele, JE Strauss, KR Georgeff, Platelet rich plasma; Growth factor enhancement for bone grafts.Oral Surg Oral Med Oral Path Oral Radiol Endod 1998 96:638-46. [Google Scholar]
[7]. A Simonpieri, M Del Corso, G Sammartino, DM DohanEhrenfest, The relevance of choukroun’s platelet-rich fibrin and metronidazole during complex maxillary rehabilitations using bone allograft. Part II: implant surgery, prosthodontics, and survivalImplant Dent 2009 18:220-29. [Google Scholar]
[8]. SR Kokate, AM Pawar, An in vitro comparative stereomicroscopic evaluation of marginal seal between MTA, glass inomer cement & biodentine as root end filling materials using 1% methylene blue as tracerEndod 2012 2:36-42. [Google Scholar]