A Custom Made Skeletal Class II Corrector Appliance in Late Adolescent Phase
Navneet Singh1, Tulika Tripathi2, Priyank Rai3, Shilpa Kalra4, Neha5
1 Senior Research Associate, Department of Orthodontics and Dentofacial Orthopedics, Maulana Azad Institute of Dental Sciences, Delhi, India.
2 Senior Professor and Head, Department of Orthodontics and Dentofacial Orthopedics, Maulana Azad Institute of Dental Sciences, Delhi, India.
3 Professor, Department of Orthodontics and Dentofacial Orthopedics, Maulana Azad Institute of Dental Sciences, Delhi, India.
4 Senior Resident, Department of Orthodonticsand Dentofacial Orthopedics, Maulana Azad Institute of Dental Sciences, Delhi, India.
5 Senior Research Associate, Department of Orthodontics and Dentofacial Orthopedics, Maulana Azad Institute of Dental Sciences, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Navneet Singh, C 43, Street 3, Kanti Nagar Extension, Delhi-110051, India.
E-mail: dr.navneetgujjar@gmail.com
Skeletal Class II correction in deceleration phase of growth is both a challenge and dilemma with choice between extraction and myofunctional therapy. With marginal growth remaining the convenient choice is extraction for camouflage of the skeletal discrepancy. On the other hand, the treatment with Fixed Functional Appliances (FFAs) helps in resolution of the problem without sacrificing the dentition. However, the conventional FFAs requires a phase of alignment which results in further loss of time to utilize any remaining growth. The present report proposes the use of a novel custom made functional appliance for Class II skeletal correction which is simple to fabricate and convenient to use.
Deceleration, Functional Appliance, Growth, Retrognathic Mandible
Case Report
Diagnosis and Aetiology
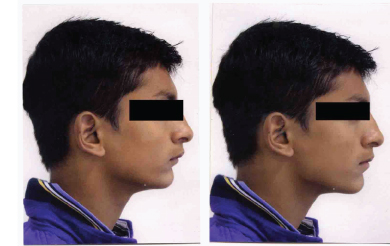
A 16-year-old male reported to the Department of Orthodontics with a chief complaint of forwardly placed upper front teeth. On extraoral examination, the patient had a convex profile, incompetent lips, acute nasolabial angle, retrognathic mandible and deep mentolabial sulcus [Table/Fig-1]. Intraoral examination revealed a Class II canine relation present bilaterally and the molar was in Class II relation on right side. The lower left first molar was missing as it was extracted three years back due to caries. The patient had an overjet of 11 mm, spacing in the upper arch and coincident upper and lower midlines [Table/Fig-1]. The cephalometric analysis revealed a Class II skeletal pattern (ANB 5°, angle of covexity 8° and Wits value +3 mm) with retrognathic mandible (SNB 73°) and proclination of maxillary anteriors (upper 1 to SN 120°) [Table/Fig-2]. The patient had an average growth pattern (FMA 26°) and was in CVMI deceleration stage. Clinically, patient showed positive Visual Treatment Objective (VTO) [Table/Fig-3].
Treatment Objectives
To correct skeletal Class II relation and achieve normal overjet and overbite thereby improving soft tissue profile and lip competence.
Treatment Plan
Although, the patient was in deceleration stage of Cervical Vertebrae Maturation Index(CVMI), a positive VTO favoured myofunctional therapy for skeletal class II correction; also the patient was not willing for extraction treatment. One of the major indication of FFAs who report at the fag end of the facial growth for treatment [1]. Hence, FFAs were chosen for better results. Conventional FFAs warranted fixed orthodontic therapy but this would require time for alignment and leveling resulting loss of remaining growth potential of the patient. Hence, it was decided to fabricate an appliance, which would be able to bring the mandible forward and did not require a prior phase of fixed orthodontic treatment for alignment.
Fabrication of Appliance
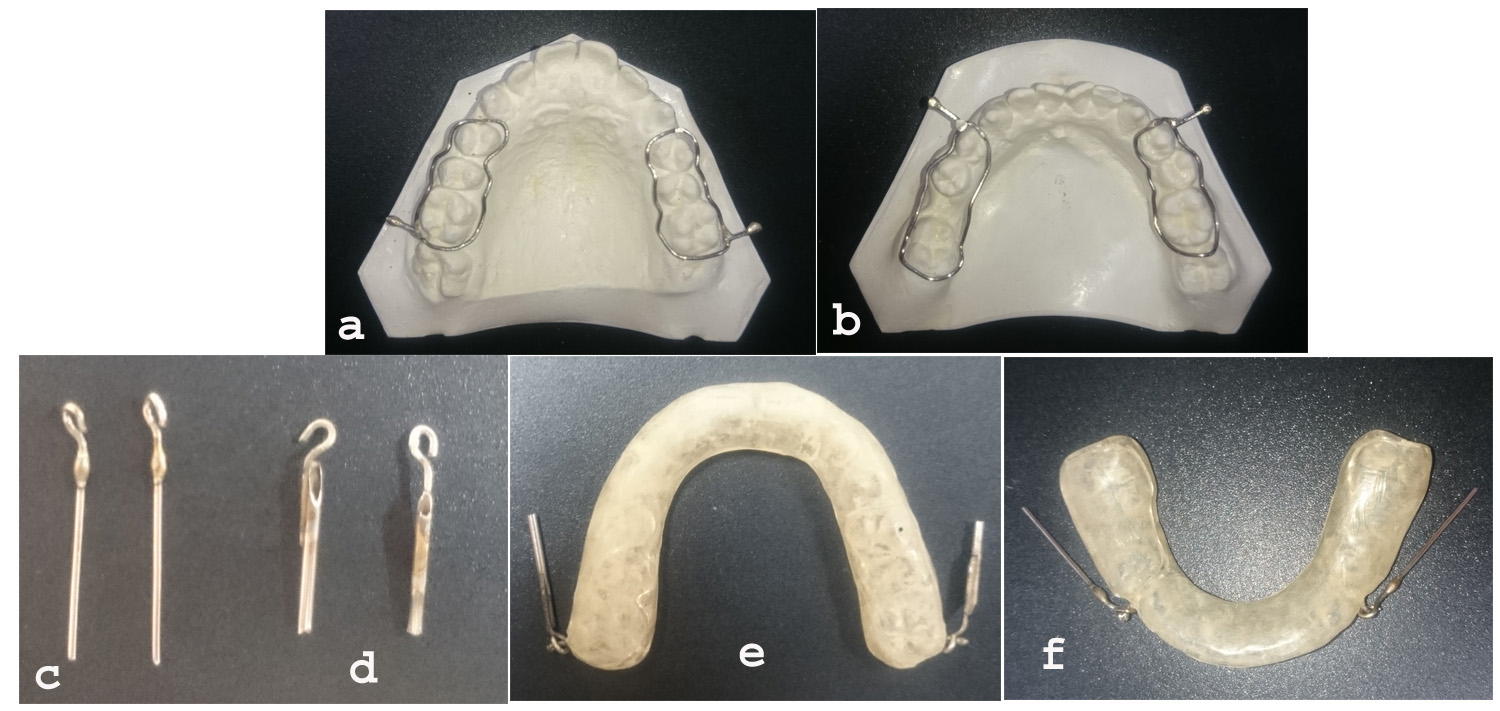
The appliance components comprised of the following component:
Metallic component which included wire framework, tube, pin and NiTi coil spring
Wire framework was adapted over the buccal and lingual surfaces of upper and lowers posterior teeth which reinforced the retention of the appliance. Also, a wire extension was soldered distal to upper first molar and distal to lower canine region with a ball end for the purpose of attachment of tube and pin assembly respectively [Table/Fig-4a,b].
A pin component was made with a 20-gauge wire with hook made at one end and just distal to the hook, a stopper was made with blob of solder material to avoid slippage of coil spring mesially [Table/Fig-4c].
A tube was made by cutting a 16-gauge needle to an appropriate length and a hook was soldered on the one end [Table/Fig-4d].
Coil Spring: NiTi open coil spring of dimension 0.010”X 0.036” was used between tube and pin assembly.
Acrylic splint covering entire dentition was fabricated for upper and lower arches. The wire framework was embedded in the acrylic splint [Table/Fig-4e,f].
Appliance Assembly
The components of the appliance were assembled so that the soldered hook on the tube was engaged onto the ball end at the distal aspect of upper first molar in the upper splint and the soldered hook on the pin engaged onto the ball end distal to lower canine in the lower splint.
The tube and pin components were cut accordingly to the bite registered for the patient, which was 7 mm of horizontal advancement.
Open coil spring was then inserted between tube and pin to keep the appliance in active state so as to bring the mandible in desired protruded position.
Treatment Progress
A custom made appliance was fabricated for the patient and was inserted in the patient mouth [Table/Fig-5]. After wearing the appliance for eight months, significant improvement was noticed in profile and lip competency. The correction of molar and the canine relationship was achieved along with significant reduction in overjet and overbite [Table/Fig-6]. Final detailing was done with 0.022” preadjusted edgewise MBT (McLaughlin, Bennett and Trevisi) appliances. In the mandibular arch, right second molar was protracted to attain a Class I molar relationship. After completion of fixed orthodontic treatment, treatment objectives were fulfilled with good intercuspation [Table/Fig-7]. Hawley’s retainers in upper and lower arches were given for retention. [Table/Fig-2] compares the cephalometric measurements of pretreatment, post functional and post-treatment results.
Pretreatment extraoral and intraoral photographs.

Comparative cephalometric measurement.
| Parameters | Pretreatment | Post Functional | Post-Treatment |
|---|
| SNA | 78° | 78° | 78° |
| Maxillary length | 94 mm | 94 mm | 94 mm |
| SNB | 73° | 76° | 76° |
| Mandibular length | 115 mm | 118 mm | 118 mm |
| ANB | 5° | 2° | 2° |
| SNA | 78° | 78° | 78° |
| SN-GoGn | 27° | 28° | 28° |
| Upper 1 to NA | 40° | 37° | 29° |
| Lower 1 to NB | 17° | 19° | 19° |
| IMPA | 91° | 93° | 93° |
Patients profile and VTO photographs.
a,b) Maxillary and mandibular cast with wire framework; c,d) Tube and pin component of appliance; e,f) Maxillary and mandibular appliance.
Intraoral photographs of appliance assembly.

Post functional extraoral and intraoral photographs.

Post-treatment extraoral and intraoral photographs.

Superimposition of pretreatment, post functional and post-treatment cephalometric tracing (SN plane at Sella).

Discussion
Management of Class II malocclusion in patients who have surpassed the peak of growth period is a major challenge to orthodontists [2]. Optimal timing for functional appliance therapy is the beginning of CVMI 3(transition) stage [3]. However, growth modification has been attempted even in deceleration and maturation stage by various authors with FFAs therapy [4-7].
The first drawback with FFAs is that another 6-8 month of remaining growth period is wasted for the purpose of aligning both the arches before attachment of FFAs. Another drawback is that the treatment results with FFAs have shown more dental effects, than skeletal effects.
In this case report, considering patient’s age, and CVMI stage, our main objective was to utilize the remaining growth potential and to minimize the dentoalveolar effects as seen with FFAs.
Hence, a custom made appliance was fabricated which consisted of upper and lower acrylic splint type of appliance which covered the entire dental arch, so as make it into a rigid unit. This works on the principle of telescopic mechanism. The forward thrust exerted on the lower splint was transmitted to the mandible with minimum dentoalveolar effects due to restraining effects of the lower acrylic splint, which covered the labial surface of lower incisors.
On cephalometric analysis, significant change in skeletal, dental and soft tissue parameters was observed at the end of treatment. Post myofunctional, cephalometric values showed significant forward movement of the mandible. However, no change in sagittal position of maxilla was observed. No change in SNA angle (78°) was observed all throughout the treatment. A mandibular advancement was clearly evident as SNB angle increased from 73° to 76° with 3° reduction in ANB angle. There was an increase in mandibular length by 3 mm. The mandibular incisors were proclined by 2° after functional appliance therapy [Table/Fig-2]. Cepalometric superimposition was done using Steiner’s superimposition method (SN Plane at Sella) [Table/Fig-8]
The custom appliance has several advantages over other FFAs, which are as follows:
It is a removable appliance and hence patient was able to maintain good oral hygiene and was able to eat comfortably after removing the appliance;
It is quick and easy to wear;
The appliance was fabricated using low cost armamentarium readily available in dental office and didn’t require special expensive assembly for its fabrication. Hence, it was very cost effective.
Major drawback of this appliance is dependency on patient compliance which can be overcome by cementation of this appliance.
Conclusion
A case of skeletal Class II malocclusion with retrognathic mandible in CVMI deceleration stage was successfully treated with this custom made functional appliance, which offered more of skeletal changes than dental changes. Since the appliance could be easily fabricated with armamentarium readily available in a dental office, it proved to be very cost-effective, as compared to commercially available FFAs.
[1]. OP Kharbanda, Orthodontics diagnosis and management of malocclusion and dentofacial deformities 2013 IndiaElsevier Publisher:499-500.Chapter 40; Interception and treatment of mandibular retrusion with non-compliant fixed functional Appliances [Google Scholar]
[2]. CD Adams, MC Meikle, KW Norwick, DL Turpin, Dentofacial remodelling produced by intermaxillary forces in MacacamulattaArchives of Oral Biology 1972 17(11):1519-35. [Google Scholar]
[3]. T Baccetti, L Franchi, JA McNamara Jr, The Cervical Vertebral Maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedicsSem Orthod 2005 11(3):119-29. [Google Scholar]
[4]. W Vogt, The Forsus fatigue resistant deviceJ Clin Orthod 2006 40:368-77. [Google Scholar]
[5]. MM El-Sheikh, K Godfrey, M Manosudprasit, N Viwattanatipa, Force deflection characteristics of the fatigue-resistant device spring: An in vitro studyWorld J Orthod 2007 8:30-36. [Google Scholar]
[6]. S Karacay, E Akin, H Olmez, AU Gurton, D Sagdic, Forsus nitinol flat spring and jasper jumper corrections of class ii division 1 malocclusionsAngle Orthodontist 2006 76(4):666-72. [Google Scholar]
[7]. J Paulose, PJ Antony, B Suresh kumar, SM George, MM Mathew, J Sebastian, Power Scope a Class II corrector–A case reportContemp Clin Dent 2016 7:221-25. [Google Scholar]