Preinguinal Splitting and Reunion of Femoral Nerve Entrapping the Fleshy Fibres of Iliacus Muscle - A Case Report
LS Ashwini1, S Nagabhooshana Somayaji2, Mohandas Rao3, Sapna Marpalli4
1 Senior Grade Lecturer, Department of Anatomy, Melaka Manipal Medical College, Manipal Campus, Manipal, Karnataka, India.
2 Professor, Department of Anatomy, Melaka Manipal Medical College, Manipal Campus, Manipal, Karnataka, India.
3 Professor and Head, Department of Anatomy, Melaka Manipal Medical College, Manipal Campus, Manipal, Karnataka, India.
4 Senior Grade Lecturer, Department of Anatomy, Melaka Manipal Medical College, Manipal Campus, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. LS Ashwini, Senior Grade Lecturer, Department of Anatomy, Melaka Manipal Medical College, Manipal Campus, Manipal-576104, Karnataka, India.
E-mail: ashunature@yahoo.co.in
Division of nerves close to their origin and muscular entrapments by nerves in the limbs is not very common. Femoral nerve is the largest branch of the lumbar plexus and arises from dorsal divisions of ventral rami of L2 to L4 spinal nerves. During routine cadaveric dissection for first year medical students at Melaka Manipal Medical College (Manipal Campus), Karnataka, India, we observed a variation in the division and course of left femoral nerve in about 65-year-old male cadaver. The femoral nerve was split into two divisions above the inguinal ligament after its origin from the lumbar plexus. The lower division of the nerve passed deep to the iliopsoas muscle fibres and the upper division ran superficial to iliacus muscle deep to fascia iliaca. Both the divisions joined just above the inguinal ligament to form the trunk of the femoral nerve. Further course and distribution of the nerve was normal. The reports have shown that compression neuropathies of femoral nerve in the limbs are caused by neoplastic masses, vascular abnormalities and also by different anomalous muscles. Such neuropathies may also result from indirect compression of femoral nerve between the fibres of psoas major muscle and lateral pelvic wall. The potential clinical importance of above mentioned variations in the division of femoral nerve would emphasize the surgeons to diagnose the neuromuscular entrapments and consequent alterations of sensation in the anterior and medial aspects of the thigh.
Inguinal ligament, Lumbar plexus, Neuromuscular entrapments
Case Report
A 65-year-old male cadaver of South Indian origin was dissected at the Department of Anatomy, Melaka Manipal Medical College (Manipal Campus). The body was preserved by formalin based preservative and was stored at 4°C. The dissection procedure for pelvis and lower limb was followed as per the guidance in Cunningham’s Manual of Practical Anatomy [1].
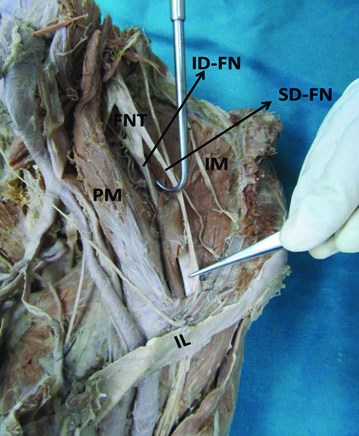
During dissection, we observed a rare variation in the division and course of femoral nerve on the left side. The femoral nerve was found to split into two divisions above the inguinal ligament after its origin from the lumbar plexus [Table/Fig-1]. The lower division of the nerve passed deep to the iliopsoas muscle fibres and the upper division ran superficial to iliacus muscle deep to fascia iliaca. Both the divisions joined after entrapping the iliacus muscle fleshy fibres just above the inguinal ligament to form the trunk of the femoral nerve. The trunk of the femoral nerve then entered the thigh deep to the inguinal ligament and was divided into anterior and posterior divisions by lateral circumflex femoral artery in the femoral triangle. The branches from both the divisions were supplying the muscles and skin over the front of the thigh. On right side, origin and course of the femoral nerve was normal.
Dissection of left iliac fossa showing the splitting of femoral nerve (FNT) in to a superior division (SD-FN) and an inferior division (ID-FN) entrapping the iliacus muscle fibers (IM) between them.
PM- Psoas Major, IL- Inguinal ligament
Discussion
Femoral nerve is the largest branch of the lumbar plexus and it arises from dorsal divisions of ventral rami of L2 to L4 spinal nerves [2]. It runs in the posterior abdominal wall and enters the front of the thigh deep to inguinal ligament to supply the muscles and skin over the front of thigh.
Neuropathies involving the femoral nerves are very rare when compared to other nerves in the lower limb [3]. Entrapment of branches of femoral nerve after the laparoscopic inguinal hernia repair in the pelvis can cause pain in the front of the thigh [3,4]. Femoral neuropathy may result from direct or indirect compression of the nerve between the psoas major muscle and the pelvic wall. Femoral nerve injury after abdominal hysterectomy or during pelvic surgery may also result from compromised blood supply to the nerve [4]. On the other hand, the iliopsoas, a key flexor of hip joint is very often injured during surgeries involving the hip joint and lower lumbar regions. Jelev L et al., reported a case of bilateral splitting of femoral nerve in the pelvis and variation in its course in a 67-year-old female cadaver [5]. They observed that, after its division, the medial part of femoral nerve was passing between psoas major and variant accessory psoas major muscles whereas, the lateral part of the femoral nerve was passing between the iliacus and accessory iliacus muscles. Such variations in the course of femoral nerve in close association with the accessory iliacus muscle can cause tension and compression of femoral nerve during iliacus compartment fasicotomy in the treatment of iliacus hematoma [5]. In the present case, we reported an entrapment of muscle fibres of iliacus by the femoral nerve. Such a case of muscle entrapments by the nerves are not reported in the literature as per our knowledge. The pain in the lower back and pelvis is usually attributed to iliopsoas muscle. A strain on this muscle can cause muscle spasms and create trigger points in the fascia covering it or in the muscle. Femoral nerve neuropathy, iliacus haematoma, pelvic and gynaecological surgeries are the most possible causes for such aggravated pain [5,6].
The embryological reason for such variation seen in our case might be due to interaction of developing femoral nerve into the L2, L3 and L4 muscular blastemal (myotome) during the intrauterine life [7].
Conclusion
Entrapment and compression neuropathies of peripheral nerves of the extremities are very common. Such variations are easily noticeable in MRI and CT scans. But, the muscular entrapments and compression by the splitting of nerves in the pelvis is not reported so far in the literature. Thus, present case might put some insight on persistent chronic pain in the pelvis and lower back. The present case may be important for the surgeons, gynaecologists, anesthesiologist, physiotherapist and clinician to conduct the surgical and radiological procedures involving the femoral nerve and the muscles of posterior abdominal wall and pelvis.
[1]. Romanes GJ, Cunningham’s Manual of Practical Anatomy 2000 15th edNew yorkOxford University Press [Google Scholar]
[2]. Standring S, Ellis H, Healy JC, Johnson D, Williams A, Collins P, et al, Gray’s Anatomy: The Anatomical Basis of Clinical Practice 2005 39th edLondonElsevier, Churchill Livingstone [Google Scholar]
[3]. De Burca N, Anterior thigh pain - A case reportManual Therapy 2011 16:291-95. [Google Scholar]
[4]. Chen SS, Lin AT, Chen KK, Chang LS, Femoral neuropathy after pelvic surgeryUrology 1995 46:575-76. [Google Scholar]
[5]. Jelev L, Shivarov V, Surchev L, Bilateral variations of the psoas major and the iliacus muscles and presence of an undescribed variant muscle – accessory iliopsoas muscleAnn Anat 2005 187(3):281-86. [Google Scholar]
[6]. Bohrer JC, Walters MD, Park A, Polston D, Barber MD, Pelvic nerve injury following gynaecologic surgery: a prospective cohort studyAm J Obstet Gynaecol 2009 201:531-37. [Google Scholar]
[7]. Sadler TW, Tosney K, Cheschier NC, Langman’s medical embryology 2011 12th edPhiladelphiaWolters Kluwer Health/Lippincott Williams & Wilkins [Google Scholar]