Central Variant of Posterior Reversible Encephalopathy Syndrome – A Rare Case Report
KG Srinivasan1, Padhmini Balasubramanian2, KR Mayilvaganan3, Usha Nandhini Kannan4, Mohamed Bilal5
1 Director and Senior Consultant, Department of Radiodiagnosis, KGS Advanced MR and CT Scans, Madurai, Tamil Nadu, India.
2 Consultant, Department of Radiodiagnosis, KGS Advanced MR and CT Scans, Madurai, Tamil Nadu, India.
3 Consultant, Department of Radiodiagnosis, KGS Advanced MR and CT Scans, Madurai, Tamil Nadu, India.
4 Consultant, Department of Radiodiagnosis, KGS Advanced MR and CT Scans, Madurai, Tamil Nadu, India.
5 Consultant, Department of Radiodiagnosis, KGS Advanced MR and CT Scans, Madurai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. KR Mayilvaganan, 785, Annanagar, Madurai-625020, Tamil Nadu, India.
E-mail: kamalret2@gmail.com
Posterior Reversible Encephalopathy Syndrome (PRES) is a clinicoradiological condition associated with headache, altered mental status, dizziness and white matter vasogenic oedema in parieto-occipital region. It is often associated with hypertension but can also occur in diverse clinical settings like immunosuppression, eclampsia, etc. It is due to failure of autoregulatory mechanism of posterior circulation in response to change in blood pressure. We hereby report a rare case of central variant of PRES secondary to severe hypertension diagnosed with 3T MRI. Objective of reporting this case was to describe the imaging findings of typical and rare atypical patterns of PRES. A 71-year-old male hypertensive patient was referred for brain imaging with history of short period of loss of consciousness, headache and dizziness. MRI brain showed central variant pattern of PRES with preferential involvement of brainstem, thalami and periventricular white matter with sparing of frontal, parietal and occipital lobes. The patient was treated with anti-hypertensive after which patient’s symptoms subsided. The patient was followed up conservatively. Atypical variants of PRES should be borne in mind when pontine hyperintensity is encountered in hypertensive patient.
Hypertension, Magnetic resonance imaging, Pontine hyperintensity
Case Report
A 71-year-old male patient was referred for brain imaging, patient with the history of short period of loss of consciousness, headache and dizziness. The patient was a known hypertensive for the past two years but was not on regular medications. On clinical examination the patient had a very high blood pressure of 200/140 mmHg and there were no signs of any focal neurological deficit. Routine blood investigations including complete blood count and serum electrolytes were within normal limits.
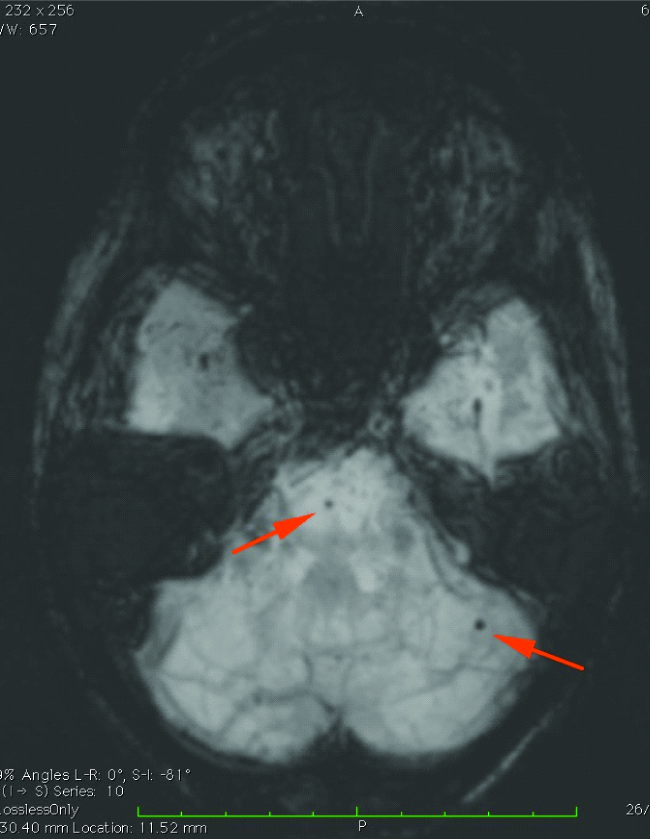
Brain MRI was performed on a 3T unit (Magnetom Spectra, Siemens). The following pulse sequences were used: - axial T2, FLAIR, sagittal T1, SWI, T2 coronal, diffusion imaging at B0, B1000 with ADC and 3D TOF MRA. MRI Brain SWI [Table/Fig-1] showed haemorrhages involving right cerebellum, pons, left posterior parietal lobe, both putamen and parietal sub cortical region with blooming of lesions in SWI representing microbleeds.
MIP SWI axial section of brain showing microbleeds in pons and left cerebellar hemisphere (represented by arrows).
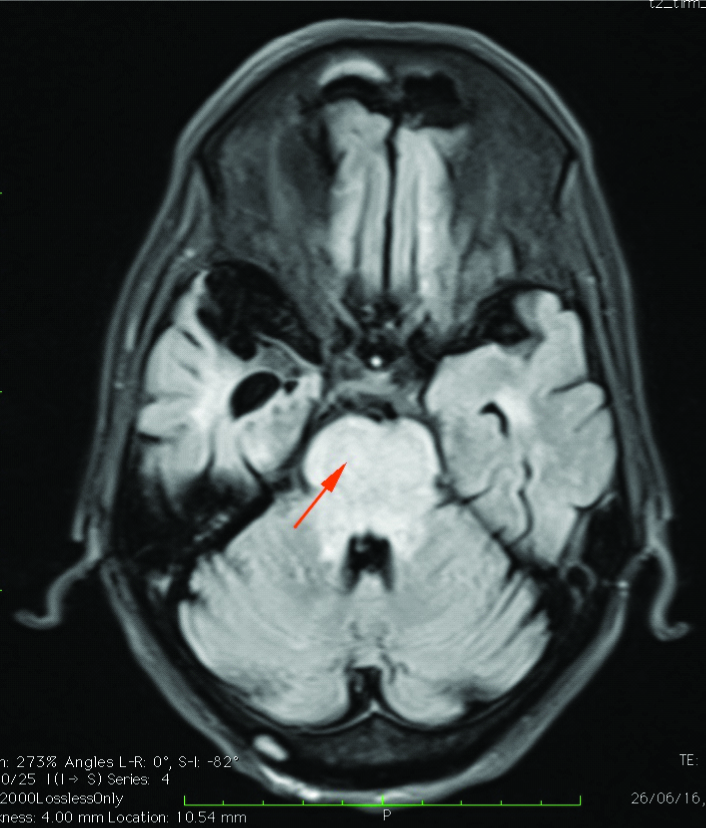
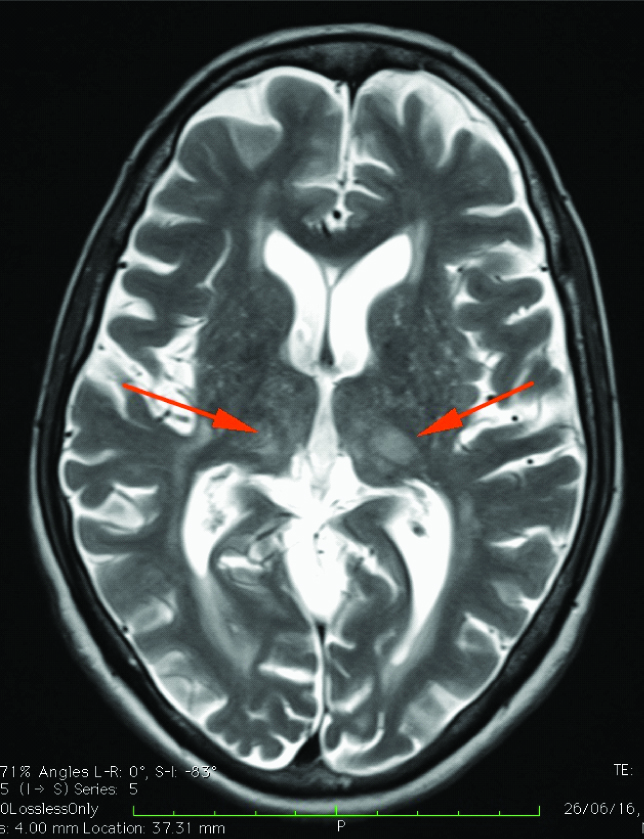
There was diffuse T2- FLAIR hyper-intensity involving brainstem predominantly involving pons [Table/Fig-2] with restricted diffusion. Hyperintensities were also seen in bilateral thalami [Table/Fig-3] and bilateral periventricular white matter. Magnetic Resonance Angiogram (MRA) was unremarkable without significant narrowing or occlusion of major intracerebral arteries.
FLAIR axial section of brain at the level of pons showing hyperintensity of pons (represented by arrow).
T2W axial section of brain showing ill-defined hyperintensities involving bilateral thalami (represented by arrows).
On the basis of clinical examination and imaging findings, a diagnosis of central variant of PRES superimposed on chronic hypertensive encephalopathy was made. Relative lack of brainstem signs and symptoms also supports the diagnosis of PRES.
The patient was treated with continuous IV infusion of 0.3 mcg/kg/min of sodium nitroprusside and then titrated according to the mean arterial pressure following which the blood pressure gradually came down to 160/84 mmHg over a period of two days. Later he was switched over to oral antihypertensives (olmesartan+amlodipine) and the BP was stabilised to 120/80 mmHg over a period of one week.
The symptoms of the patient subsided. Patient was not willing for follow up scan and hence follow up imaging could not be done. Informed consent has been obtained from the patient for publishing.
Discussion
PRES refers to the condition of vasogenic oedema of white matter that occurs in various clinical settings like elevated blood pressure, chemotherapy toxicity, bone marrow transplantation [1,2]. It is a clinicoradiological entity characterized by altered mental status, headache, and visual disturbances due to transient altered cerebral perfusion. This condition is reversible with resolution of the findings in the follow up scan. The pathophysiology behind PRES is not clearly understood and two mechanisms have been put forth- failure of auto regulation and endothelial dysfunction resulting in vasogenic oedema [1,2]. The terminology PRES is actually a misnomer as it can involve other regions of brain parenchyma.
Typical and atypical forms of PRES have been documented. In the typical form, the parieto-occipital lobes are consistently involved. Three patterns of imaging [1] have been identified in the typical form. They are holohemispheric, superior frontal sulcal and dominant parieto-occipital pattern. In holohemispheric pattern the watershed areas between ACA-MCA and MCA-PCA is usually involved and the frontal pole involvement in frontal lobes will be seen. In the superior frontal sulcal pattern, in addition to parieto-occipital involvement, superior frontal sulcus will be involved without extension to frontal pole. Finally in the dominant parieto-occipital pattern, there will be typical posterior involvement of parieto-occipital lobes. In the atypical forms [1], there can be unilateral or asymmetric pattern of involvement and in partial expression of PRES, there is absence of classical parieto-occipital lobe involvement with either parietal or occipital lobe involvement. Unusual locations like brainstem, cerebellum, basal ganglia and splenium, deep white matter involvement in PRES have been documented previously [3-7]. Atypical patterns like parenchymal or subarachnoid haemorrhages, restricted diffusion and altered brain perfusion in PRES [2] have also been documented.
The present case is an example of atypical central variant pattern of PRES. In central variant, there is preferential involvement of brainstem, thalami and periventricular white matter with sparing of frontal, parietal and occipital cortex [3,4,6]. Similar case reports of central variant of PRES have been documented earlier. Maciel R et al., have reported a similar case due to hypertension and the MRI findings resolved completely on follow up scan after control of hypertension [5]. Karakis I et al., have reported three similar cases of brain stem variant of PRES due to hypertension [6]. McKinney AM et al., in his study has shown that 4% of PRES cases were central variant [2]. Bartynski WS et al., has shown that 12.5% of patients have brainstem involvement with four patients having thalami and mid brain vasogenic oedema as dominant pattern [1].
The differential diagnosis of pontine T2- FLAIR hyperintensities includes central pontine osmotic myelinolysis/pontine neoplasm/ infarction/demyelination and central variant of PRES [7]. These entities can be differentiated on the basis of MR imaging findings along with clinical correlation. In central pontine myelinolysis, the central fibres are affected with sparing of periphery and show restricted diffusion. The affected area enhances with contrast. Pontine astrocytoma –diffuse variety affects typically paediatric age group patients and enhances on contrast administration. Pontine infarction is often asymmetric and affects both central and peripheral portion showing restricted diffusion in acute stages. Pontine hypertensive encephalopathy affects central and peripheral portion and does not enhance with contrast. It is generally associated with hypertension and most often do not show restricted diffusion. This condition is reversible with control of blood pressure. In demyelination, apart from the brainstem typical areas in the supratentorial regions of the brain like periventricular, corpus callosum are affected and they show restricted diffusion in the acute phase [7].
The combination of MRI findings with lack of brainstem signs in a patient with hypertension should alert the clinician about the possibility of central variant of PRES.
Conclusion
The clinicians and radiologist should be aware of atypical variants of PRES so that an accurate diagnosis and early treatment could be given to the patient to avoid permanent neurological damage.
[1]. Bartynski WS, Boardman JF, Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndromeAmerican Journal of Neuroradiology 2007 28(7):1320-27. [Google Scholar]
[2]. McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, SantaCruz KS, Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findingsAmerican Journal of Roentgenology 2007 189(4):904-12. [Google Scholar]
[3]. McKinney AM, Jagadeesan BD, Truwit CL, Central-variant posterior reversible encephalopathy syndrome: brainstem or basal ganglia involvement lacking cortical or subcortical cerebral oedemaAmerican Journal of Roentgenology 2013 201(3):631-38. [Google Scholar]
[4]. Chen DY, Tseng YC, Hsu HL, Huang YL, Chen CJ, Teaching NeuroImages: central variant of posterior reversible encephalopathy syndromeNeurology 2014 82(19):e164 [Google Scholar]
[5]. Maciel R, Nzwalo H, Palma R, Pizhin D, Martins A, Shamassa M, The resolution of central variant of posterior reversible encephalopathy syndromeThe Neurohospitalist 2015 5(2):91-92. [Google Scholar]
[6]. Karakis I, MacDonald JA, Stefanidou M, Kase CS, Clinical and radiological features of brainstem variant of hypertensive encephalopathyJVIN 2009 2(2):172-76. [Google Scholar]
[7]. Guzmán-De-Villoria JA, Ferreiro-Argüelles C, Fernández-García P, Differential diagnosis of T2 hyperintense brainstem lesions: Part 2. Diffuse lesionsSemin Ultrasound CT MR 2010 31(3):260-74. [Google Scholar]