Human body can withstand variation in environmental temperature due to tight thermoregulation. During systemic exposure, heat is dissipated by increased blood flow and sweating. However, heat stress produces strain on the cardiovascular system, evidenced by large increase in sympathetic neural activity, heart rate and left ventricular contractility, coupled with reductions in central blood volume, left ventricular filling pressures and cerebral perfusion [1].
Heat to a localized part such as to the extremity is known to improve the cutaneous blood flow and tissue perfusion [2]. The reflex control of skin blood flow in humans includes sympathetic neurogenic vasodilatation during body heating and noradrenergic vasoconstriction during body cooling induces neural release of substance P and bradykinin [3]. Later, much prolonged vasodilatation is caused by release of Nitric Oxide (NO) from endothelium [3]. It improves transdermal delivery of drugs and nutrients. In a classical study, human forearms subjected to 45oC temperature for two hours showed maximal increase in blood flow. Temperature up to 43oC for eight hours to the digits is well tolerated [4]. A study from Minson et al., from University of Oragon and Rochester, a temperature of 43oC was used to study the skin blood flow response to local heating and it showed statistically significant percentage rise of the skin blood flow [5].
Oxygen is essential for healing of chronic wounds. Oxygen is involved in all the phases of wound healing such as inflammatory, proliferative and maturation. Oxygen enhances leukocyte functions, induces angiogenic responses, growth factor secretion, collagen deposition, fibroblast related wound contraction. Topical oxygen therapy has become standard therapy in management of lower extremity wounds [6,7].
A combination of local heat and oxygen would be beneficial in many clinical scenarios of non-healing wounds without any systemic effects. No studies have addressed the effects of the warm oxygen therapy exposure to extremity. The hypothesis of the study was that exposure of extremity to warm oxygen causes local vasodilatation independent of systemic mechanisms seen with total body exposure to hot environment exposure.
Hence, the purpose of the present study was to evaluate the local and systemic effects of the exposure of extremity to warm oxygen in healthy volunteers.
Materials and Methods
The present prospective observational study was conducted in Vydehi Institute of Medical Sciences and Research Centre, Bengaluru, Karnataka, India, among the employees of the institution during the months of May 2016 to June 2016. Institutional Ethics Review Board approval was taken before the conduct of the study.
Inclusion criteria were healthy volunteers between 18-25 years who consented for the study. Subjects who had cardiovascular diseases, neurological, endocrine diseases, dermatological disease of foot and smoking were excluded.
The minimum sample size required for statistical analysis was 30. Subjects who gave the consent for the study were enrolled in the study. The participant information brochure explaining the study was given to each of the volunteers and the study was clearly explained. Demographic profile was collected. Vital parameters of the subjects were taken before the procedure.
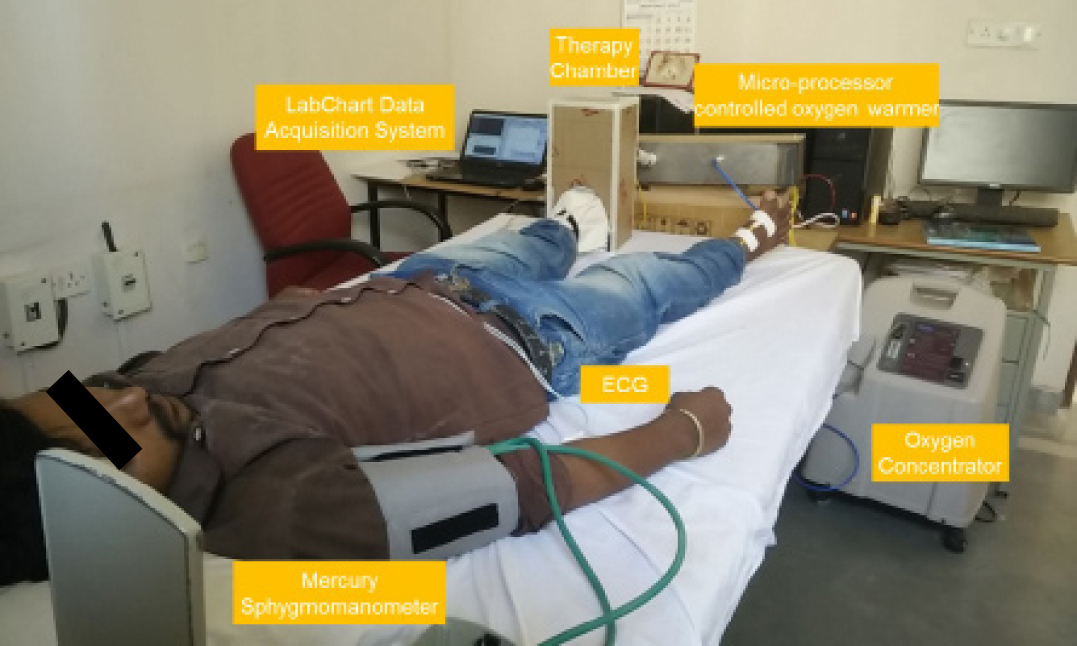
The study setup included the oxygen concentrator, oxygen warmer, therapy chamber, sensors and the data acquisition system [Table/Fig-1].
Oxygen was generated using the oxygen concentrator. Invacare – Platinum 9, a validated oxygen concentrator used in the experiment was an adjustable flow oxygen concentrator that generated 87%-95.6% oxygen depending on the flow rate. For the purpose of our experiments, the flow rate was fixed at 7l/min which generated a constant oxygen supply of 93%-95.6% concentration.
Oxygen from the concentrator was routed to the oxygen warmer which heated the oxygen to a temperature range of 30oC-65oC. The oxygen warmer was a micro-processor controlled heater that warmed the constant stream of oxygen and precisely maintained the ambient temperature of oxygen inside the therapy chamber at 43oC. The warm oxygen was in turn fed to the therapy chamber through insulated pipes.
The therapy chamber used for the experiment was an insulated box of dimensions 16 cm x 16 cm x 34 cm with adequate cushioning and insulation. The inner wall of the chamber was lined with polystyrene and heat reflective material to retain heat and maintain the temperature of the environment at 43oC.
The study was conducted in a room where temperature of 26oC-28oC was maintained. One temperature sensor each was fixed with adhesive tape at the same position over the dorsum of both feet [Table/Fig-2]. These temperature sensors measured the skin temperature of the right and left foot and recorded the information continuously every 11 seconds. Initial stabilization values were taken with both the feet outside at ambient room temperature. Then one of the leg was kept inside the chamber for a period of 90 minutes. The contralateral limb not exposed to the chamber was the control used to monitor the changes.
Positions of skin temperature sensor and pulse monitor on feet.

On the foot to be exposed to warm oxygen, the pulse monitor was strapped to the plantar surface of the hallux as shown in [Table/Fig-2]. The pulse monitor was connected to AD Instruments data logger. A foot was placed inside the therapy chamber and a flap with Velcro based contraption was used as a closing mechanism to reasonably retain the warm oxygen within the therapy chamber. However, sufficient flexibility was provided so that the restraining mechanism was not tight while at the same time ensured heat retention within the therapy chamber. It must be noted that the warm oxygen pumped into the therapy chamber at 7l/min had sufficient room to escape to the atmosphere i.e., the experiment was conducted under normobaric conditions. The oxygen warmer was automatically switched off when the temperature of dry oxygen increased beyond 43oC.
The volunteer’s basal blood pressure and core body temperature were measured. During the procedure, blood pressure and core body temperature were recorded every 15 minutes using a manual sphygmomanometer and digital thermometer respectively and recorded manually. Electrocardiogram (ECG) was measured continuously using a 3 lead ECG and fed to AD Instruments data logger. Images of the plantar aspect of the index foot were taken before and after the warm therapy to document hyperaemia. At the end of the study the subject was provided with a Numeric Rating Scale (NRS-11) based scoring which requires the participant to verbally score pain at the scale of 0-11 points and asked to rate the comfort/discomfort that they had experienced during the procedure and was documented by healthcare worker.
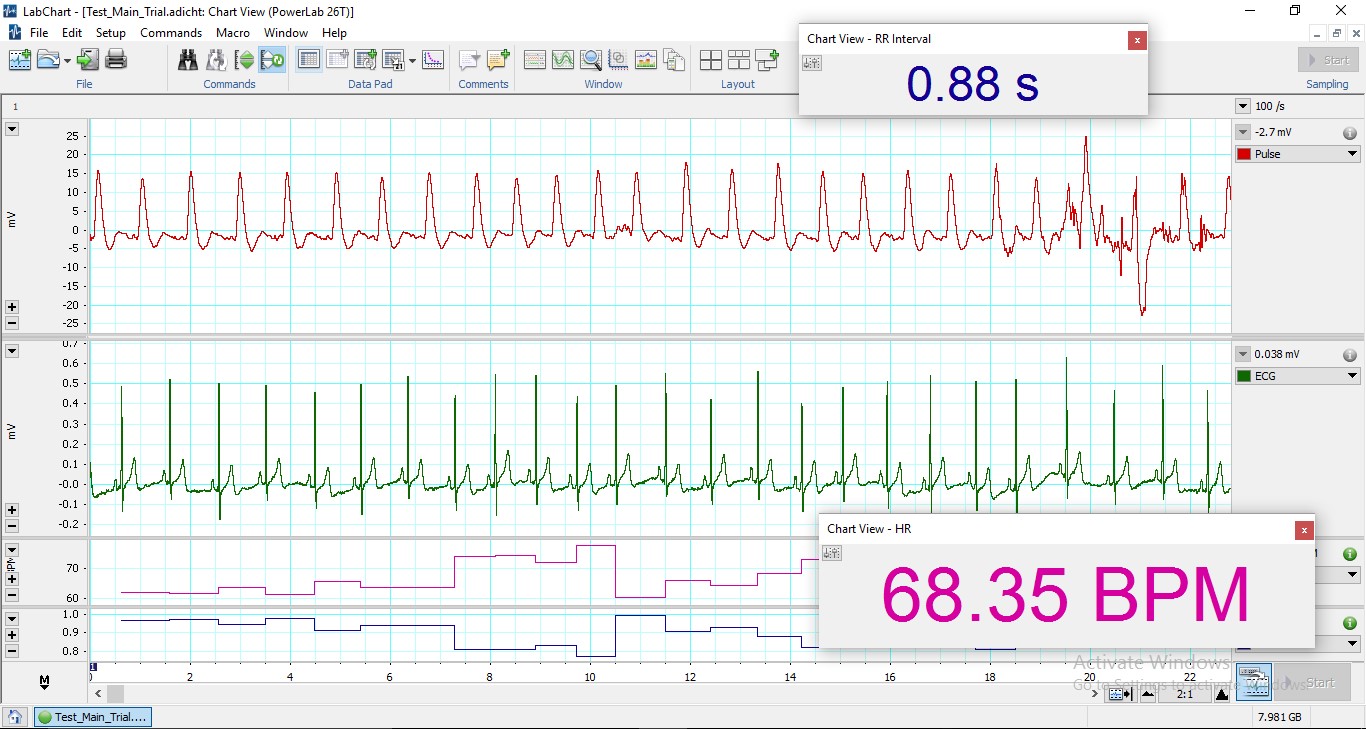
The instruments connected to AD Instruments data acquisition system were directly visualized and recorded on the LabChart software [Table/Fig-3].
Snapshot of AD instruments LabChart viewer.
Statistical Analysis
All the analysis was done using SPSS-16.0 software and p-values less than 0.05 were considered statistically significant.
Results
Of the 35 volunteers selected for the pilot study, data from 31 volunteers were considered for further statistical analysis. Data recorded from four volunteers were discarded due to technical errors. The results were analysed for statistical significance to evaluate the systemic and local effects of warm oxygen exposure to the lower extremities in healthy volunteers.
A total of 31 healthy male volunteers were selected for the pilot study, which were of mean age of 20.9 years±2 years. Their mean height was 167.1cm±8.6 cm, mean weight 54.8Kg±8.6 kg and mean BMI 19.7±3.1.
The average experimental foot skin temperature was 34oC when compared to the normal foot which was 32.9oC, an increase of 3.34% during the 90 minutes experiment. This increase in the foot temperature was statistically significant (p=0.011).
The core body temperature changed from 98.63oF to 98.54oF, a decrease of 0.32% during the course of the experiment. The decrease in temperature was statistically significant (p<=0.037).
The average heart rate changed from 75.8 to 71.9 BPM, a decrease of 5.15% during the experiment. This change in the heart rate is statistically significant (p=0.001).
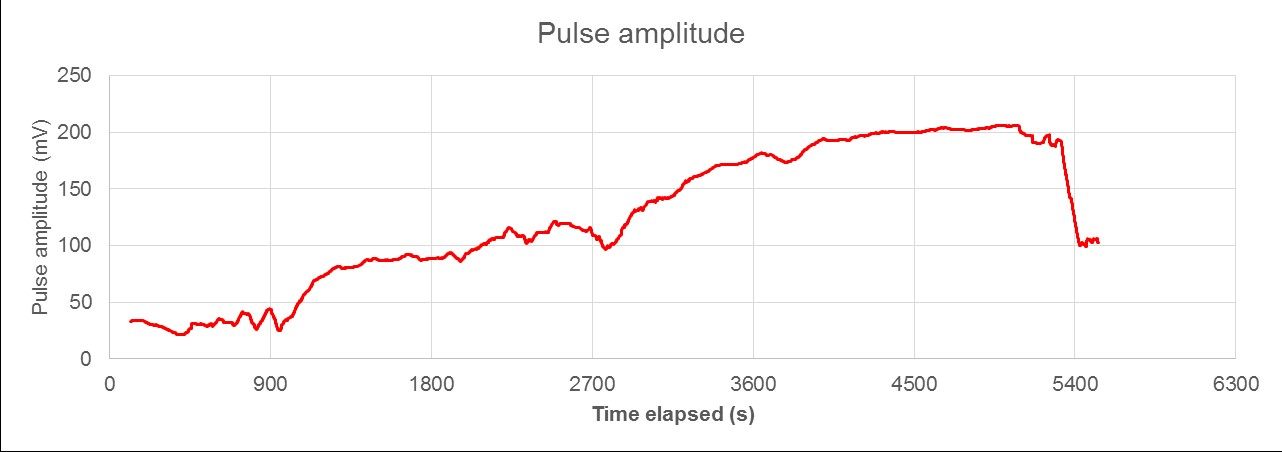
The average pulse amplitude changed from 39.8 mV to 79.8 mV, an increase of 100.5% over the duration of the experiment [Table/Fig-4]. This change is statistically significant (p<0.001). Pulse amplitude change of the subjects was graphically represented [Table/Fig-5]. ECG was monitored and recorded throughout the protocol period and no ECG changes were noticed.
Change in pulse amplitude recorded in one of the subjects.
| Heart Rate (Beats/Min) | Core Body Temperature (F) | Pulse Amplitude (mV) | Skin Temperature (0C) |
|---|
| Start of the experiment | 75.8 | 98.6 | 39.8 | Left Foot | 34 |
| End of the experiment | 71.9 | 98.5 | 79.8 | Right Foot | 32.9 |
Average experimental systolic blood pressure changed from 109.9±10.5 mmHg to 107.8±9.7 mmHg, a decrease of 1.91% during the 90 minutes experiment. This change in systolic blood pressure was not significant (p=0.054).
Due to inadequate light exposure in the experiment room and lack of standardization procedure followed to capture image of plantar aspect of index foot, no conclusive results could be drawn from the images to analyse hyperaemia.
No subject complained of discomfort in the lower extremity that was exposed to warm oxygen. All subjects rated zero on the NRS-11, when asked to rate the asked to rate the comfort/discomfort that they had experienced during the procedure.
Discussion
The goal of the present study was to evaluate if application of local heat with oxygen improves local blood flow and tissue oxygenation. Local heat in humans produces vasodilation as a result of sympathetic cholinergic action and release of local vasodilator substances such as nitric oxide, substance P, calcitonin, gene related peptide etc. In a study a temperature of 43oC was used to study the skin blood flow response to local heating of the limb and it showed statistically significant percentage rise of the skin blood flow [5].
Our study showed similar results with doubling of skin blood flow with an average increase in pulse amplitude. Many methods have been used to measure blood flow, for example - pulse oximeter, Laser Doppler flow meter. In the present study piezo electric pulse oximeter waveform analysis and percentage of pulse amplitude was utilized to document vasodilatory response. Topical oxygen supplement is known to improve tissue oxygenation as measured by pulse oximeter. However, this change was not observed in present due to intact skin.
In a classic study by Moritz AR et al., the lowest surface temperature that was responsible for cutaneous burns was 44oC and the minimum time required to cause burns was four hours [8]. We applied a temperature of 42oC for 90 minutes which was safe range to the study population with reference to tolerance and risk of burns.
Local vasodilatation can cause immediate decrease in arterial blood pressure and heart rate due to decrease in the vascular resistance [9]. We noticed both decrease in heart rate and blood pressure but heart rate drop was statistically significant.
The result of the study can be extrapolated to the healing of chronic non healing wounds using warm oxygen therapy. Further studies are required on patient population to prove benefits in clinical settings.
Limitation
The current pilot study was conducted in small group of patients which in itself is a limitation; study on larger group can provide more valid results. This study addresses healthy volunteers and not the target group of patients with chronic wounds.
Conclusion
This study has definitely shown increase in skin blood flow on exposure of warm oxygen to the extremity. Extending the same therapy on patients with non-healing wounds could provide novel therapy in such patients.