Distal humerus fractures are associated with many problems like fracture communition, osteoporotic bone and complex fracture anatomy. Elderly patients are even more difficult to manage because poor quality bone makes osteosynthesis challenging. There have been variable reports as regards to functional outcome of open reduction and internal fixation of these fractures. Also, newer literature suggests, total elbow arthroplasty as a reasonable option in these patients barring the cost [1-5]. Achieving a good functional range of motion at the elbow with stability are the primary objectives in managing a communited distal humerus fracture. Hence, it is very necessary to determine if fracture fixation is successful in achieving a stable mobile joint. Managing good articular reduction thereby, making sure that painful arthritis does not develop is equally critical. Not many studies have assessed the success of internal fixation of communited intra-articular fractures in elderly in terms of functional success [6,7]. The number of patients included in these studies is too few to draw viable conclusions.
The aim of the study was to evaluate the intermediate term results (minimum follow up of two years) of communited intra-articular distal humerus fractures treated with bicolumnar plating with or without olecranon osteotomy in elderly Indian population.
Materials and Methods
In the present retrospective cohort study, patients operated with bicolumnar plating for communited intra-articular distal humerus fractures at the tertiary care center were included in the time period between February 2009 and April 2013. The study was carried out on 63 consecutive patients after approval of the Institutional Ethics Committee and Departmental Review Board. All patients had an age more than 60 years at the time of surgery. A minimum follow up of two years post surgery was a mandatory criterion. Only fractures those were Orthopaedic Trauma Association (OTA) type 13C were included [8]. Type 13-C1 fractures encompass simple articular, metaphyseal fractures, Type 13-C2 are simple articular but have a communited metaphysis and lastly Type 13-C3 are multi fragmentary articular fractures.
All patients had underwent open reduction internal fixation with bicolumnar plating using a posterolateral or lateral locking plate and a medial locking or reconstruction plate medially [9]. No patient having pre existing arthritis or inflammatory joint disease was included. All fractures were closed and open fractures were discarded from the study. All surgeries were done within one week of trauma in lateral position using the standard posterior midline approach by different surgeons in the same trauma unit. Most of the patients were operated by the triceps reflecting approach while only six had needed an olecranon osteotomy [10,11]. Two patients developed a postoperative wound complication with discharge and had received immediate wash and antibiotics for two weeks following which their course was uneventful. All patients were subjected to the elbow range of motion and physiotherapy protocol as per the standard departmental guidelines. The physiotherapy protocol included immediate elbow range of motion within one week of surgery along with isometric exercises. All patients were supported by means of a hinged elbow brace for three to four weeks. After four weeks of surgery the brace was discarded and unrestricted flexion extension and pronosupination was commenced.
After taking due consent from the Departmental and Institutional Review Board, the patients were subjected to a thorough clinical examination. After a thorough history, complete evaluation of the range of motion including the flexion- extension arc and supination-pronation arc was done. The Disabilities of Arm and Shoulder and Hand (DASH) score and the Mayo Elbow Performance (MEP) score were calculated [12,13]. DASH score is thirty point exhaustive questionnaire that accurately analyses the function of the arm, elbow and hand scoring the difficulty with which the patient performs a given activity from 1 to 5. The MEP score is an elbow centric score that assesses the pain, mobility, stability and function of the elbow.
Statistical Analysis
All data were tabulated in a Windows Excel spreadsheet (Microsoft Excel 2011) and statistically analysed using SPSS software version 20.0. The results were compared to the contralateral normal elbow using the student’s t-test. A p-value of less than 0.05 was considered significant.
Results
Of the 63 patients that were included, only 41 were available for data collection and analysis as 14 patients could not be traced. Five patients refused to give consent. Three patients had died of unrelated causes in the interim period. The mean age of the patients was 66.4 years with a standard deviation of 4.7 years. Of the remaining 41 cases, 11 were type 13-C1, 23 were type 13-C2 and seven were type 13-C3. Of the included patients, 27 were males while 14 were females. The mean follow-up was of 38 months with the range being from 26 to 82 months. Two patients had undergone implant removal and implant prominence. Three patients had radiological evidence of elbow arthritis. There were no complications with respect to the olecranon osteotomies and two patients had undergone a secondary procedure of excision of a mass of heterotropic ossification.
The mean extent of flexion was 120 (range of 80 degrees to 140 degrees) with a mean flexion contracture of 15 degrees. The mean range of supination was 81° with a standard deviation of 14° and the mean range of pronation was 75 degrees with a standard deviation of 11 degrees [Table/Fig-1].
Comparison of functional scores and range of motion with the normal contralateral side.
| Operated side | Non operated side | p-value |
|---|
| Mean | S.D | Mean | S.D |
|---|
| DASH Score | 21.4 | 4.9 | 12.2 | 3.9 | <0.001 |
| MEP Score | 85 | 15.5 | 90 | 19 | 0.1954 |
| Mean Flexion Arc (degrees) | 105 | 19 | 126 | 13 | <0.001 |
| Supination (degrees) | 81 | 14 | 88 | 17 | 0.0451 |
| Pronation (degrees) | 75 | 11 | 82 | 12 | 0.0073 |
DASH-Disablities of arm and shoulder and hand; MEP-Mayo elbow performance; SD-standard deviation, test used-unpaired t-test
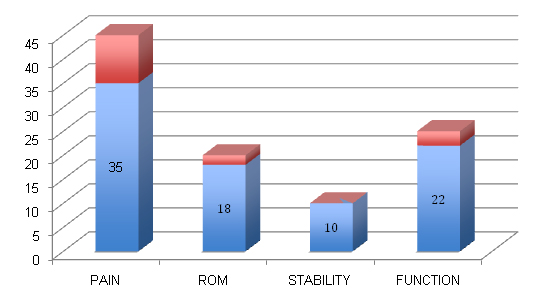
The mean MEP score was 85 with a range of 50 to 100. All elbows were stable. Also, the range and function were found to be good. Of the 41 elbows, six were in the ‘excellent’ group (score 91-100), 25 were ‘good’ (score 75-90), eight were ‘fair’ (score 60-74) and two were ‘poor’ (score less than 60) [Table/Fig-2,3].
Distribution of patients with respect to the MEP score.
| MEP SCORE |
|---|
| GROUP | SCORE | NUMBER (n) |
|---|
| Excellent | 91-100 | 6 |
| Good | 75-90 | 25 |
| Fair | 60-74 | 8 |
| Poor | <60 | 2 |
| Total | 41 |
MEP-Mayo elbow performance
Average performance of patients in each component of MEP score. Maximum score-(Total-100; Pain-45; ROM-20; Stability-10; Function-25).
On the other hand, the mean DASH score was 21.4 with a standard deviation of 4.9. The two patients who had a MEP score in the poor zone had a DASH score of 54 and 67.2 respectively. Both these patients had radiological evidence of elbow arthritis. Both patients who had undergone a secondary procedure for removal of a heterotropic ossification mass, had a MEP score lying in the ‘fair’ range.
The mean DASH score on the operated side was 21.4 as opposed to 12.2. Both these scores fell within Group 2 of DASH score i.e., with good functional outcome [12]. Also, the mean MEP score was 85 and 90 on the operated and normal side respectively. This was not a significant difference (p = 0.1954). The mean ranges of motion and the flexion arc were within functional range.
Discussion
Treatment of distal humerus fractures mainly the intra articular types is a challenging task. These fractures may be compounded by many problems such as significant communition and multiple intra-articular fracture lines. This problem is further compounded by increased incidence of osteoporosis in the older population. Several studies have demonstrated a good outcome of fixation in these fractures. However, many studies have quoted a significant failure rate of upto 25% especially in elderly patients. The aim of treatment was accurate articular reduction, rigid fixation and early, efficient physiotherapy and rehabilitation.
In our study, all patients achieved fracture union with mean MEP and DASH scores being 85 and 21.4 respectively. These scores although poor were comparable to the opposite side. Also, the mean supination-pronation arc and flexion-extension arc was 156 degrees and 105 degrees respectively. This is well within the functional range of elbow. The mean block to extension was at 15 degrees with a mean maximal flexion of 120 degrees. All patients had radiologic evidence of fracture union and only two patients underwent a secondary procedure for removal of a heterotropic ossification mass.
A study by Greiner S et al., in 2008 evaluating the functional outcome after osteosynthesis in distal humerus fractures had similar results [14]. The mean DASH score was 18.5±11.5 with the mean flexion being 121 degrees and an extension deficit of 17.9 degrees. Another study by Atalar AC et al., evaluating the functional outcome of complex distal humerus fractures in 21 patients found the mean MEP and DASH score to be 86.1 and 7.5 respectively [15]. Also, the mean range of flexion was 118.1 degrees. Doornberg JN et al., evaluated long term results of parallel plate fixation in thirty patients in all types of distal humerus fractures. The average MEP and DASH score was 91 and 7 points respectively [6]. The average flexion arc was 106 degrees and the supination pronation arc was 165 degrees. However, all these studies did not focus on the elderly population. A retrospective study by Huang JI et al., evaluated the functional outcome of bicolumnar plating only in the elderly. The MEP and DASH score in their study was 83 and 37.6 respectively. The mean elbow flexion- extension arc was from 20 to 120 degrees [Table/Fig-4] [6,7,14,15].
Comparison of functional outcomes with similar studies.
| n | DASH Score | MEP Score | Flexion-Extension Arc | Supination-Pronation Arc |
|---|
| Greiner S et al., (2008) [14] | 14 | 18.5 | 91 | 103.8 | - |
| Atalar AC et al., (2009) [15] | 21 | 7.5 | 86.1 | 90.2° | - |
| Doornberg JN et al., (2007) [6] | 30 | 7 | 91 | 106° | 165° |
| Huang JI et al., (2011) [7] | 14 | 37.6 | 83 | 92° | 152° |
| Our study | 41 | 21.4 | 85 | 105° | 156° |
Many studies have evaluated the functional outcome of total elbow arthroplasty and claimed it to be a better option mainly in the elderly age group. A study by Cobb TK et al., in 1997 included 15 elbows that underwent total elbow arthroplasty [1]. They found the mean range of flexion from 25 to 130 degrees. Gambirasio R et al., reported a mean MEP and DASH score of 93 and 23 with total elbow arthroplasty at three years follow up [3]. Kamineni S et al., reported a minimum follow up of two years for distal humerus fractures treated with total elbow arthroplastyI [4]. The mean MEP score was 93 and the mean flexion-extension arc was from 24° to 131°. However, many studies included patients having inflammatory arthritis of the elbow which was not so in our study [16-20].
Although, our study conclusively establishes the success of early bicolumnar plating for communited distal humerus fractures with respect to the functional outcome, we feel there are certain shortcomings. The primary weakness of this trial was that it is a retrospective study. Also the maximum follow up available with us is six years and 10 months with the mean follow up being 38 months only. We do not have any comparison of results with total elbow arthroplasty mainly in elderly patients in our institute.
Our study conclusively establishes that excellent functional outcome can be achieved with open reduction and internal fixation in Type C distal humerus fractures in elderly including the ones that are communited. Total elbow arthroplasty although a viable option, gives similar results to a well done internal fixation. This is of extreme significance especially when affordability of the prosthesis is an issue. Our study concurs with similar studies in the past as regards to the functional outcome [6,7,14,15]. However, it is one of the few studies that has specifically evaluated the outcome in elderly [7].
Conclusion
Accurate reduction along with stable internal fixation is the foundation stone of success in intra-articular distal humerus fractures. We establish that internal fixation with bicolumnar plating offers good functional results in communited intra-articular fractures even in osteoporotic bone with a negligible complication and revision rate in elderly population.
DASH-Disablities of arm and shoulder and hand; MEP-Mayo elbow performance; SD-standard deviation, test used-unpaired t-test
MEP-Mayo elbow performance