Bonding has been an area of paramount interest in Orthodontic research ever since the introduction of acid etching technique by Buonocore in 1955 [1]. An ideal orthodontic adhesive should have optimal bond strength to withstand masticatory and orthodontic forces and also debond with no damage to the enamel at the end of the treatment.
Transbond XT, a conventional light cured Bis-GMA based composite resin has been the popular material of choice in Orthodontic bonding today. This product is time tested and by far the most ideal bonding adhesive in Orthodontics. Orthofix, a new material was exclusively introduced for orthodontic bonding purposes and owing to the indigenous make, the material is less expensive compared to the imported adhesives. However, the application of this material for orthodontic purpose has not been scientifically evaluated so far. Therefore, the present study was designed to evaluate the overall bond failure rates and the overall mean survival time of two Bis-GMA based composite materials, namely, Transbond XT and Orthofix by an in-vivo double blinded randomized clinical trial. The bond failure pattern and mean survival time between maxillary and mandibular arches and between anterior and posterior segments of the two composite materials were also done.
Materials and Methods
The protocol of this study was revised and approved by the Department of Orthodontics, Saveetha Dental College and Hospital, Saveetha University, Chennai, Tamil Nadu, India. Written informed consent was obtained from those who agreed to participate voluntarily prior to clinical trial and human ethical clearance was obtained from scientific review board and ethical committee of Saveetha University. The study involved selected subjects requiring fixed orthodontic treatment.
Thirty three consecutive participants who fulfilled the inclusion criteria were included in the study from a list of patients seeking orthodontic treatment which consisted of 19 females and 14 males.
Inclusion Criteria
Having complete permanent dentition
Patients requiring fixed appliance therapy
Type of malocclusion including Class I, Class II and Class III
Adolescent or adult patients
Absence of buccal or labial restorations
Both extraction and non extraction patients
Exclusion Criteria
Teeth with facial restorations or congenital enamel defects
Teeth not fully erupted
Surgically exposed teeth
Teeth where bracket could not be immedietly placed
Dentition with occlusal interferences and deep bite hindering proper bracket positioning
In order to have an adequate power of 90% for showing a statistically significant difference (p<0.05) in proportions with atleast one failed bracket after six months, the RCT needed 270 teeth per group which is approximately 33 patients using a log rank test, ignoring the matching. A buffer of 20% was included in order to compensate for any loss to follow up.
The selected 33 patients were randomly allocated by lottery method into two groups: Group A with 17 patients and Group B with 16 patients. Double blinding was done where the patient was unaware of the material used and site where the adhesive was used. The operator was not involved in choosing the site for placement of the adhesive.
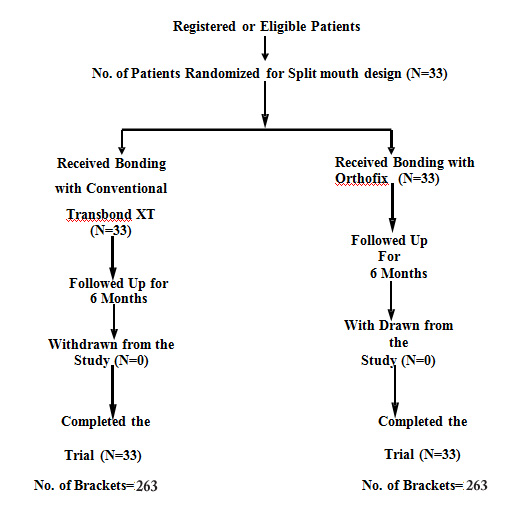
The split mouth design was followed in this study where each patient acted as his own control hence, errors due to patient variability was reduced. The variability introduced due to different oral conditions and masticatory loads in different individuals was also minimized. Each patient’s mouth was divided into four quadrants. In Group A, maxillary right and the mandibular left quadrants were bonded using Orthofix [Table/Fig-1,2] and the remaining quadrants were bonded using Transbond XT [Table/Fig-3,4]. In Group B, the quadrants were reversed. This was done so that both the materials were equally distributed on maxillary and mandibular right and left quadrants. The profile of the randomized clinical trial is tabulated in [Table/Fig-5].
Orthofix (Anabond stedman pharma research).

Stedbond S (Anabond stedman pharma research).

Transbond XT (3M Unitec, Monrovia California).

3M Scotchbond multipurpose.

Profile of randomized clinical trial.
Standardization was achieved by bonding all the brackets in one appointment by the same operator. The usual choice of aligning arch wires was either a 0.014 inch NiTi wire or a 0.016 inch NiTi wire, depending on the initial level of alignment and crowding.
Bonding, follow up and assessment of bond strength was conducted by one operator (investigator). The data was recorded in the record sheet prepared for each patient for the purpose of follow up which included all the required personal details of the patient. The record sheet also had the dates of bonding of each bracket, dates of follow-up calls, adhesive in each quadrant, site and date of bond failure and the possible reason for the bond failure.
Both patient groups were followed for a period of six months. If a bond failed, the details were recorded. The patients were reviewed every 3-4 weeks. Also, in between normal follow up appointments, patients were enquired about any unreported breakages by regular phone calls.
The duration of treatment for each breakage was calculated as the difference between the date of breakage and the date of initial bonding. But bonded teeth that had been rebonded after failure were not included in the study because replacing a bracket can affect its bond strength [2]. The data so obtained at the end of six months was then statistically evaluated.
Statistical Analysis
The data obtained from the study was tabulated. The level of significance was at 5% (0.05), and the power of the study was 90%. The mean and standard deviation was calculated for both the groups to get the arithmetic average of the observations. The independent t-test was performed to compare the mean values between the groups and chi-square test was performed to compare the proportion of bond failure in different groups. The Kaplan Meier estimator was performed to calculate the survival time.
Results
Among the 33 patients, there were 263 brackets in each of the groups. There was no loss of follow up.
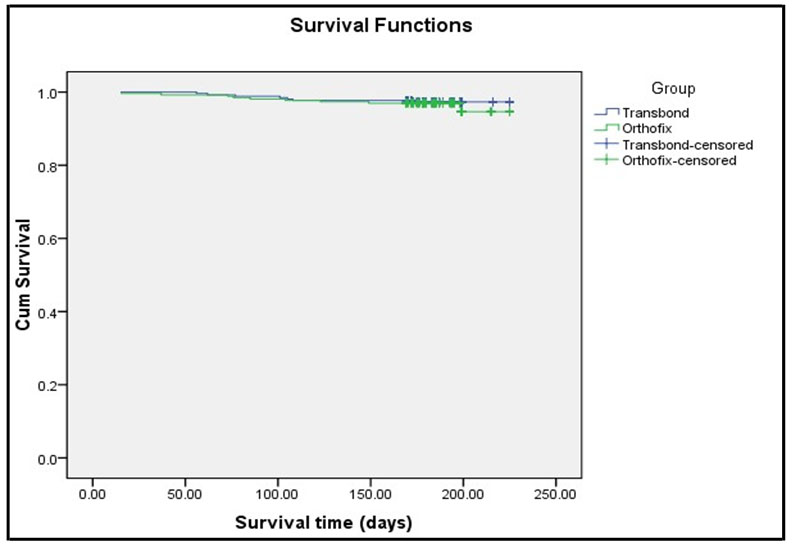
There were 16 bond failures in total, of which seven (2.7%) occurred with Transbond XT and nine (3.6%) occurred with Orthofix. Chi-square analysis result showed that the proportion of failure between all the groups were statistically not significant (p>0.05) [Table/Fig-6]. The mean survival time in Transbond XT group was 183.56±19.75 days and in Orthofix, it was 182.98±22.7 days (p>0.05) [Table/Fig-7]. The mean estimated survival time for Transbond XT was 221.58 days (SE of the estimate was 1.321) and for Orthofix was 220.07 days (SE of the estimate was 1.671) [Table/Fig-8]. All of the above differences were found to be statistically insignificant. The Kaplan-Meier survival plot showed similar survival time for both the groups and most of the bond failures were noted in the initial three months of treatment [Table/Fig-9].
Comparison of overall bond failure rates between Transbond XT and Orthofix.
| Group | Total |
|---|
| Transbond XT | Orthofix |
|---|
| N | % | N | % | N | % |
|---|
| Status | Success | 256 | 97.3 | 254 | 96.6 | 510 | 97.0 |
| Failure | 7 | 2.7 | 9 | 3.4 | 16 | 3.0 |
| Total | 263 | 100.0 | 263 | 100.0 | 526 | 100.0 |
| Chi-square Tests | Value | Df | p-value |
| Pearson Chi-square | 0.258 | 1 | 0.612 |
Independent t-test to compare mean survival days between Transbond XT and Orthofix.
| Group | N | Mean | S.D. | p-value |
|---|
| Survival Time(days) | Transbond XT | 263 | 183.56 | 19.75 | 0.756 |
| Orthofix | 263 | 182.98 | 22.70 |
Kaplan-Meier survival analysis-means for survival time between Transbond XT and Orthofix.
| Group | Mean |
|---|
| Estimate | Std. Error | 95% Confidence Interval |
|---|
| Lower Bound | Upper Bound |
|---|
| Transbond XT | 221.58 | 1.321 | 218.99 | 224.17 |
| Orthofix | 220.07 | 1.671 | 216.80 | 223.35 |
| Overall | 220.82 | 1.067 | 218.73 | 222.92 |
Overall Kaplan Meier survival plot comparing Transbond XT and Orthofix.
The failure rate and survival time were studied with both groups based on the maxillary and mandibular arches. The failure rate of Transbond XT in maxilla was 2.3% and mandible was 3%. Orthofix also showed a similar failure rate with 3.1% in maxilla and 3.8% in mandible. The significance value of 0.7 showed that there was no statistical significance among the groups [Table/Fig-10]. The mean survival time for Transbond XT in maxillary arch was 183.95±18.94 days and in mandibular arch was 183.17±20.59 days. Similarly the mean survival time in maxillary arch for Orthofix is 184.08±18.03 days and in mandibular arch is 181.89±26.55 days. The difference between these mean values were statistically in significant [Table/Fig-11].
Comparison of bond failure rates in maxillary and mandibular arch for brackets bonded with Transbond XT and Orthofix.
| Group | Arch | Total |
|---|
| Maxilla | Mandibular |
|---|
| | N | % | N | % | N | % |
|---|
| Orthofix | Status | Success | 127 | 96.9 | 127 | 96.2 | 254 | 96.6 |
| Failure | 4 | 3.1 | 5 | 3.8 | 9 | 3.4 |
| Total | 131 | 100.0 | 132 | 100.0 | 263 | 100.0 |
| Transbond XT | Status | Success | 128 | 97.7 | 128 | 97.0 | 256 | 97.3 |
| Failure | 3 | 2.3 | 4 | 3.0 | 7 | 2.7 |
| Total | 131 | 100.0 | 132 | 100.0 | 263 | 100.0 |
| Group | Chi-square Tests | Value | Df | p-value |
| Orthofix | Pearson Chi-square | 0.107 | 1 | 0.743 |
| Transbond XT | Pearson Chi-square | 0.139 | 1 | 0.709 |
Independent t-test to compare mean survival days between arches in Transbond XT and Orthofix.
| Group | | Arch | N | Mean | S.D. | p-value |
|---|
| Orthofix | Survival Time(days) | Maxillary | 263 | 184.08 | 18.03 | 0.437 |
| Mandibular | 263 | 181.89 | 26.55 |
| Transbond XT | Survival Time(days) | Maxillary | 263 | 183.95 | 18.94 | 0.747 |
| Mandibular | 263 | 183.17 | 20.59 |
The survival rate was found to be more in the anterior segment when compared to the posteriors. [Table/Fig-12]. The survival time for Transbond XT and Orthofix also showed similar differences [Table/Fig-13].
Comparison of bond failure rates in anterior and posterior for brackets bonded with Transbond XT and Orthofix.
| Group | Segment | Total |
|---|
| Anterior | Posterior |
|---|
| N | % | N | % | N | % |
|---|
| Orthofix | Status | Success | 180 | 97.3 | 74 | 94.9 | 254 | 96.6 |
| Failure | 5 | 2.7 | 4 | 5.1 | 9 | 3.4 |
| Total | 185 | 100.0 | 78 | 100.0 | 263 | 100.0 |
| Transbond XT | Status | Success | 182 | 97.8 | 74 | 96.1 | 256 | 97.3 |
| Failure | 4 | 2.2 | 3 | 3.9 | 7 | 2.7 |
| Total | 186 | 100 | 77 | 100 | 263 | 100 |
| Group | Chi-square Tests | Value | Df | p-value |
| Transbond XT | Pearson Chi-square | 0.640 | 1 | 0.424 |
| Orthofix | Pearson Chi-square | 0.977 | 1 | 0.323 |
Independent t-test to compare mean survival days between anterior and posterior segment in Transbond XT and Orthofix.
| Group | | Segment | N | Mean | S.D. | p-value |
|---|
| Orthofix | Survival Time(days) | Anterior | 263 | 183.45 | 21.13 | 0.604 |
| Posterior | 263 | 181.86 | 26.15 |
| Transbond XT | Survival Time(days) | Anterior | 263 | 184.45 | 17.88 | 0.258 |
| Posterior | 263 | 181.42 | 23.67 |
Discussion
In orthodontic treatment, the need to replace brackets frequently may severely impair the progress of treatment and can be expensive in terms of material and time. Therefore, a low clinical failure rate is a necessary clinical criterion of paramount importance. Orthofix a Bis- GMA based light cure orthodontic adhesive (marketed by Anabond Stedman Pharma Research) has been introduced specifically for orthodontic bonding. Orthofix contains Bis-GMA/TEGDMA matrix with barium glass fillers and fumed silica. The total filler content is 65% w/w with an average particle size of about 0.7 micron. Polymerization occurs by exposing Orthofix to visible light at a wave length of 470 nm and an intensity of 500 W/cm2 for about 20 seconds [3]. This composite resin is manufactured based on the technology developed by Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST). The material has been tested at SCTIMST as biocompatible and non-cytotoxic.
Laboratory tests are often used to evaluate the performance of bonding agents but clinically bonded brackets are subjected to a wide range of forces acting at different temperatures [4]. The bond strength in a clinical scenario is a reflection of all the characteristics of an adhesive like microleakage, debonding characteristics, flow properties, depth of penetration, depth of curing and water sorption. The survival time assesement allows some significant difference to be underlined which is impossible with failure rates [5].
A split mouth randomised clinical trial was adapted where each patient was his own control, therefore, errors due to patient variability was reduced. Both the operator and the patients were unaware of the adhesive being used.
Literature revealed that different studies done to evaluate bond failure rates in the past had different follow up time periods. A study by Banks P et al., [6] with follow up through the complete treatment period was ideal as different types and magnitude of forces were experienced at different phases of treatment. Other studies reported had a follow up time ranging from six months (Ireland JA et al., [7], Littlewood SJ et al., [8]),12 months (Elekdag-Turk S et al., [9]) to15 months (Krishnaswamy R et al., [10]). In the present study, all the patients were followed up for six months time and bracket failures were noted.
It is pertinent to remember that failure rate and pattern might change with increased follow up time as higher dimension wires were used in the terminal stages of the treatment [11]. This parameter was only partially considered in this study as most of the cases included in the study had reached 19X25 NiTi in 0.022 slot which was an increased force level during the six months of the study [12].
Studies by O’Brien KD et al., [13], Sunna S et al., [14], Adolfsson U et al., [15] reported failure rates between 4.7-6.6%, 4.5-7.7%, 7.2% respectively for various adhesive bracket combinations. The overall bond failure rate in the present study over the period of six months was found to be 3%. This shows that there was a 97% success rate with a mean survival time of 220.82 days [Table/Fig-6,7].
The overall bond failure rate and mean survival days for Transbond XT (2.7%/221.58) was similar to Orthofix (3.4%/220.07) with no statistically significant difference during the six month period of the study [Table/Fig-7].
Since not all brackets failed by the end of study period, a survival analysis was done. The Kaplan-Meier survival analysis showed that the mean survival time for brackets bonded with Transbond XT (221.58 days) was similar to Orthofix (220.07 days) and the Log Rank test showed that brackets bonded with Orthofix had a survival time for six months statistically equal to that of brackets bonded with Transbond XT [Table/Fig-8,9].
Studies reported by Krishnaswamy R et al., [10], Aljubouri YD et al., [16] revealed maximum number of bond failures in the initial five to six months of treatment for a 15 months follow up study, done to compare efficacy of curing source. First, any deficiency in the bond strength of individual bracket/adhesive combination such as air inclusion, inadequate enamel preparation, and poor moisture control would become evident during the first few months of treatment. Second, this initial period of treatment is also a time of acclimatization for patients because they experience restrictions concerning the food that can be masticated with abonded appliance. Unfortunately, it is also a time of experimentation, and bond failures happen when patient is advised restrictions on diet. Third, the initial phase of treatment in many patients involves deep bite, and as a consequence, heavy occlusal forces might be applied to many bonded attachments, thereby resulting in bond failures.
Similar to the findings of the above studies, the present study showed maximum number of bond failures after the initial three months of the treatment. The possible reasons for the bond failure in most patients were due to hard brushing and biting on hard food in spite of being cautioned.
The literature on bonding has shown that the pattern of orthodontic bond failure in vivo is not uniform for all the teeth in either dental arch and also between the arches. So, in the present study, comparisons were also studied in the bond failure rates in different locations of the mouth, in order to identify the pattern of orthodontic bond failure.
The trend observed by most of the studies in past was more number of bonds failing in mandibular arch compared to maxillary arch Newman GV [17] (Max: 10% and Mand: 16%), Zacchirsson BU et al., [18] (Max: 9.5%, Mand: 20.8%), Trimpeneers LM et al., [19] (Max: 15% Mand: 22%), Adolfsson U et al., [15] (Max: 4.85%, Mand: 9.9%). Although, the reason for these different patterns of bond failure are not fully understood, potential reasons could include increased masticatory loading on mandibular bonds and poor moisture control (Hobson RS et al., [20], Mattick CR et al., [21]). Sunna S et al., [14] in their in vivo study showed greater failure rate in mandibular (9%) as compared to maxillary arch (4%) but, in their ex vivo study for each tooth type, there were no significant differences in shear bond strength between dental arches. In the present study, failure rates demonstrated significant differences between maxillary and mandibular attachments, with mandibular bonds failing more frequently (Max: 2.7% bond failure and Mand: 3.4% bond failure) [Table/Fig-10,11].
The pattern observed in the previous studies showed premolar/posterior failures exceeded incisor/anterior failures as reported by Sunna S et al., [14] (Ant: 5.1% Post: 10.7%), Zacchirson BU [18] (Ant: 7.1% Post: 18.2%), O Brien KD et al., [13] (Ant: 2.6% Post: 11.8%), Trimpneers LM et al., [19] (Ant: 13.8% Post: 26.4%), Adolfsson U et al., [15] (Ant: 5.6% Post: 11.2%).
Several authors have similar findings like Newman GV [17], Zacchirson BU [18], Trimpneers LM et al., [19] and Adolfsson U et al., [15]. The reason for the failure include poor moisture, poor visibility, increased masticatory loads, and altered tooth morphology with increased a prismatic enamel in posterior teeth affecting the micromechanical bond properties. Another factor is the increased labial curvature of the premolars. Uneven resin thickness due to increased curvature might lead to higher levels of bond failure in these teeth. In the present study, it was seen that among the failures in anterior segment, teeth #21 and 12 showed more number of debonding. Maximum number of failures were seen in the premolars in the mandibular segment. Possible reason for bond failure in anteriors could probably be negligence by the patient while eating.
Thus, the results of this in vivo evaluation of Transbond XT and Ortho fix revealed that both the adhesives exhibited low bond failure rate. This can be attributed to the inherent bond strength of both Transbond XT and Orthofix. Thus, Orthofix can be considered an ideal orthodontic bonding adhesive.
Apart from acceptable clinical survival rates and bond strength, an ideal orthodontic adhesive should also have acceptable handling properties, reduced chairside time, and should be non toxic, aesthetic and cost effective. Orthofix was introduced as an orthodontic bonding adhesive however, had some limitations regarding its flow and thereby handling properties.
To summarize the present study highlighted the in vivo bond strength of a new composite resin for orthodontic bonding. There are however, other characteristics for a material to be an ideal orthodontic adhesive and that needs to be evaluated.
Limitation
Like in all others studies, this study had a few limitations like a longer follow up period is necessary, time taken in placement of the brackets with this material and the frequency of errors in placement.
Conclusion
Both the materials Transbond XT and Orthofix showed a low bond failure rate. The overall bond failure rate and mean survival time for Transbond XT was similar to Orthofix with no statistically significant difference. The survival of both the materials was within the same range. This signifies that the difference in survival of the two materials is the same.
Therefore, Orthofix can be used as an ideal orthodontic adhesive in terms of bond failure rate and survival time as analyzed in this study.