Patient participation and their empowerment is a powerful tool for the achievements on hand hygiene in health care sector [1]. Worldwide each year, nearly millions of patients were affected by HCAIs [2]. Although HCAI is the most frequently occurring adverse event in health sector, its true global burden remains challenging because of the difficulty in obtaining reliable data [2].
In developed countries, prevalence of HCAI among hospitalized patients were around 5%-15% [3] and in Intensive Care Units (ICUs), were between 9-37% [4]. According to Global Antibiotic Resistance Partnership (GARP) study, in India, the prevalence of HCAIs were around 11% to 83% and also reported that 30% of natal deaths are due to sepsis acquired from hospitals [5].
Transmission of hospital acquired pathogens occurs mostly through the unhygienic practices of the health care workers mainly via contaminated hands. Proper hand washing with soap and water has been considered one of the most important infection control measures to prevent HCAI [6]. Preventing HCAIs remains a highest priority for prevention and control specialists, though many organizations are still struggling to achieve full compliance with hand hygiene protocols [6].
“My five movement” framed by World Health Organisation (WHO) for hand hygiene compliance is considering the patient contact, patients’ surrounding and equipment’s during patient care and hand hygiene compliance for preventing HCAI. Hospital surroundings have direct or indirect contact with patient and also have frequent contact with health care providers [1].
Patient empowerment is recognized as the main tool to increase hand washing compliance among Health Care Workers (HCWs). Proper audio-visual aids coupled with health education motivates the patients to discuss on merits of hand washing with HCWs. Despite this encouragement, there were many barriers to patient participation in hand hygiene compliance like poor awareness on hand hygiene, fear and being disrespectful from HCWs clearly still exist [7-12]. Previous studies have shown that even with encouragement, patients are more likely to challenge nurses and support staff regarding hand hygiene compared with physicians [8].
In India, there is still a paucity of community based studies on assessing empowerment of patients hand hygiene practices. Understanding and assessing the global burden of hospital acquired infections and perception of hand hygiene practiced in hospital by common people are important key areas to improve the hygiene practices. The present study was conducted to assess the empowerment of patients regarding hand hygiene through website.
Materials and Methods
It was the web-based cross-sectional survey conducted from September 2013 to December 2013 among online users. The study was conducted using survey monkey online questionnaire form. A predesigned questionnaire was framed based on WHO criteria to assess the awareness and patient empowerment on hand hygiene [13]. Total 10 questions were framed to assess the extent of the patient empowerment, availability of hand hygiene products in the hospital, involvement of communities to promote hand hygiene and infection control, and assessed various approaches which were considered most useful to educate people in regard to hand hygiene. Knowledge on HCAIs was also assessed [13]. Participants above 18 years and using the online services were included for the study.
Sample size-calculated by using the following formula:
n = zα2pq/l2
Where,
Zα = Type 1 error = 1.96 i.e. 5% (From the normal distribution table)
P = 0.5 (assuming prevalence of hand hygiene practice is 50%) [14]
q = 1 - p
l = 0.05 (Taking 8% as relative error)
n = ((1.962)2 ×0.5×0.5) / (0.08)2 = 150
10% as non-response rate
=150 + 15 = 165
The survey was based on non probability convenience sampling done using survey monkey online service; total 125 questionnaires were sent via Gmail and also the questionnaire was posted on Facebook (100 responses expected).
The data were transferred into excel sheet. Epi info 7 was used for analysis of data. Data were represented in percentages and proportions. Chi-square test was applied to test the significant difference between gender and respondent characteristics on hand hygiene empowerment. The p-value <0.05 was considered statistically significant.
Ethical clearance was obtained from Institutional Human Ethics Committee. Confidentiality about the participants was maintained throughout the study.
Results
Out of 165 expected responses, 94 (57%) participants completed the survey. Majority of the respondents were from Tamil Nadu and Pondicherry, India and six (6.4%) of the respondents were from other countries (US/UK/France).
[Table/Fig-1] shows the socio-demographic distribution of study participants. Majority of the participants belonged to the age group of 20-35 years with nearly equal participation from both male and female. Around 73.4% of the participants were from urban area and 61.7% were professional by occupation followed by self-employed (20.2%). Almost all respondent ever visited hospital in their life time; among them 86.2% of the respondents visited hospitals within one year. Only less than one fourth of them visited hospitals within one month.
Socio-demographic distribution of study population (n=94).
| Variables | | Frequency (n=94) | Percentage (%) |
|---|
| Age in years | <20 | 2 | 2.1 |
| 20-35 | 62 | 66 |
| 35-50 | 17 | 18.1 |
| >50 | 13 | 13.8 |
| Gender | Male | 48 | 51.1 |
| Female | 46 | 48.9 |
| Residence | Urban | 69 | 73.4 |
| Rural | 25 | 26.6 |
| Occupation | Student | 13 | 13.8 |
| Professional | 58 | 61.7 |
| Self-employed | 19 | 20.2 |
| Non-working/Housewife | 4 | 4.3 |
| Hospital visit | Ever visited hospital in life time | 94 | 100 |
| Visited within 1 year | 81 | 86.2 |
| Visited within 1 month | 23 | 24.5 |
[Table/Fig-2] shows the gender wise distribution of participants empowerment on hand hygiene. Nearly, more than half of the respondents reported the non compliance on hand hygiene among HCW. Female has greater empowerment on hand hygiene when compared with the males with significant difference. Around 43.5% of female patients asked HCW to wash/sanitize their hands before examination compared with 14.6% of male patients with significant difference (p=0.003). Total 27 out of 94 participants asked their HCWs to sanitize their hands before examination.
Gender wise distribution of participant empowerment on hand hygiene (n=94).
| S. No | Response from the respondent | Malen =48 (%) | Femalen = 46 (%) | Totaln = 94 (%) | p-value* |
|---|
| 1 | Ever asked health care worker to wash/sanitize their hands before examination | 7 (14.6) | 20 (43.5) | 27 (28.7) | 0.003 |
| 2 | Did you feel comfortable when health care worker asked to remind them to wash/sanitize their hands before examination | 41 (85.4) | 41 (89.1) | 82 (87.2) | 0.759 |
| 3 | Did you feel comfortable to ask health care worker to wash/sanitize their hands when they did not ask to remind them to wash/sanitize their hands before examination? | 9 (19.6) | 19 (39.6) | 28 (29.8) | 0.043 |
| 4 | Ever asked your health care worker to wash/sanitize their hands, if they examine you without washing their hands after examining a patient next to you. | 26 (54.2) | 39 (84.8) | 65 (69.1) | 0.002 |
*p-value <0.05 statistically significant
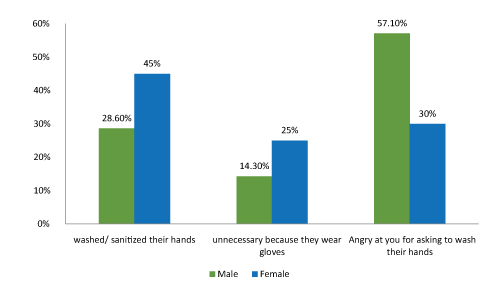
Almost 37% of the HCWs proceeded to sanitize their hands, whereas 57.1% of males and 30% females reported that their HCWs were angry for asking to wash their hands and 25% of females and 14.3% of males reported that HCWs said washing hands are unnecessary because they already wear gloves [Table/Fig-3].
Response of HCW when respondent asked to wash/sanitize their hands before examination.
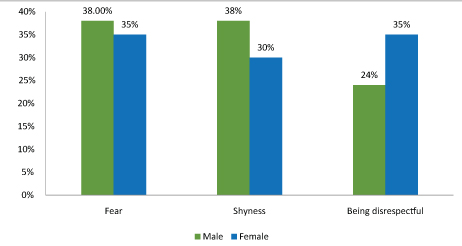
Majority of the male reported that out of fear and shyness they felt discomfort, whereas, female reported that being disrespectful was the major reason for not reminding their HCWs to wash/sanitize their hands [Table/Fig-4].
Reason for not feeling comfortable to ask HCWs to sanitize their hands when they did not ask to remind them to wash/sanitize their hands before examination.
Only 3.2% of them reported that they acquired hospital acquired infection once in their life time. Around 27.7% of the participants reported that their country/community have a program that educates/communicates patients about the importance of hand hygiene. There was no significant difference seen between male and female participants in hand hygiene attitude [Table/Fig-5].
Attitude on hand hygiene practices based on gender (n=94).
| S. No | Response from the respondent | Malen =48 (%) | Femalen = 46 (%) | Totaln = 94 (%) | p-value* |
|---|
| 1 | Did hand cleaning materials available in nearby hospital | 18 (37.5) | 13 (28.3) | 31 (33) | 0.385 |
| 2 | Did your community have program related to hand hygiene | 10 (20.8) | 16 (34.8) | 26 (27.7) | 0.168 |
| 3 | Have you ever acquired hospital acquired infection in your life time? | 1 (2.1) | 2 (4.3) | 3 (3.2) | 0.616 |
*p-value <0.05 statistically significant
Urban participants have greater empowerment on hand hygiene when compared with the rural participants with significant difference [Table/Fig-6]. Regarding attitude, urban participants were aware of the community based programmes on hand hygiene than the rural participants with significant difference [Table/Fig-7]. There were no significant associations found between patient empowerment and attitude on hand hygiene with age, occupation and number of hospital visits.
Distribution of participant empowerment on hand hygiene based on participants residence (n=94).
| S. No | Response from the respondent | Urbann =69 (%) | Ruraln = 25 (%) | Totaln = 94 (%) | p-value* |
|---|
| 1 | Ever asked health care worker to wash/sanitize their hands before examination | 23 (33.3) | 4 (16) | 27 (28.7) | 0.100 |
| 2 | Did you feel comfortable when health care worker asked to remind them to wash/sanitize their hands before examination | 64 (92.8) | 18 (72) | 82 (87.2) | 0.007 |
| 3 | Did you feel comfortable to ask health care worker to wash/sanitize their hands when they did not ask to remind them to wash/sanitize their hands before examination? | 22 (31.9) | 6 (24) | 28 (29.8) | 0.460 |
| 4 | Ever asked your health care worker to wash/sanitize their hands, if they examine you without washing their hands after examining a patient next to you. | 45 (65.2) | 20 (80) | 65 (69.1) | 0.173 |
*p-value <0.05 statistically significant
Attitude on hand hygiene practices based on participants residence (n=94).
| S. No | Response from the respondent | Urbann =69 (%) | Ruraln = 25 (%) | Totaln = 94 (%) | p-value* |
|---|
| 1 | Did hand cleaning materials available in nearby hospital | 26 (37.7) | 5 (20) | 31 (33) | 0.107 |
| 2 | Did your community have program related to hand hygiene | 25 (36.2) | 1 (4) | 26 (27.7) | 0.002 |
| 3 | Have you ever acquired hospital acquired infection in your life time? | 2 (2.9) | 1 (4) | 3 (3.2) | 0.072 |
*p-value <0.05 statistically significant
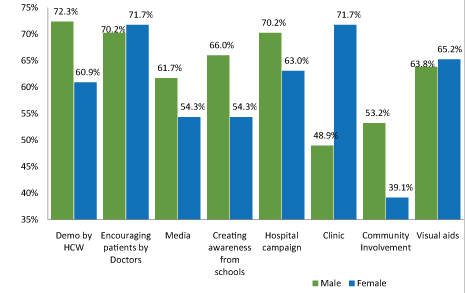
Majority of the male participant reported that Behavior Change Communication (BCC) can be done through HCWs and by hospital campaign, whereas females reported that BCC will be effective when it was done via clinic and also by encouraging patients to ask about the importance of hand hygiene by HCWs/provider. Nearly 53.2% of males and only 39.1% of females said that community involvement plays an effective role in BCC [Table/Fig-8].
Best way for behaviour change communication*.
*Multiple responses
[Table/Fig-9] shows the association between respondent characteristics and their report on compliance of hand hygiene among health care workers. Non compliance on hand hygiene among HCWs were commonly reported by urban respondents with a significant difference (p=0.004). However, there were no significant differences found in terms of sex, occupation and age groups regarding their report on compliance of hand hygiene among HCWs.
Association between respondent characteristics and their report on compliance of hand hygiene among HCWs (n=94).
| Respondent Characteristics | Variables | Respondents report on Compliance of hand hygiene among HCWs | p-value* |
|---|
| Yes (n=37) | No (n=57) |
|---|
| Sex | Male (n=48) | 18 (37.5) | 30 (62.5) | 0.833 |
| Female (n=46) | 19 (41.3) | 27 (58.7) |
| Age groups | <20(n=2) | 0 (0) | 2 (100) | 0.170 |
| 20-35(n=62) | 21 (33.9) | 41 (66.1) |
| 35-50(n=17) | 10 (58.8) | 7 (41.2) |
| >50(n=13) | 6 (46.1) | 7 (53.9) |
| Occupation | Student(n=13) | 2(15.4) | 11 (84.6) | 0.130 |
| Professional(n=58) | 25 (43.1) | 33 (56.9) |
| Non-Professional(n=19) | 7 (36.8) | 12 (63.2) |
| Non-working/Housewife(n=4) | 3 (75) | 1 (25) |
| Place | Urban (n=69) | 21 (30.4) | 48 (69.6) | 0.004 |
| Rural (n=25) | 16 (64) | 9 (36) |
*p-value <0.05 statistically significant
[Table/Fig-10] depicts the association between respondent characteristics and awareness on hospital acquired infection. It was observed that the respondent’s knowledge on hospital acquired infection, males are having higher knowledge compared with that of females with significant difference (p<0.001). However, there were no significant differences found in terms of place, occupation and age groups regarding awareness on hospital acquired infection.
Association between respondent characteristics and awareness on hospital acquired infection (n=94).
| Respondent Characteristics | Variables | Awareness on hospital acquired infection among respondent | p-value* |
|---|
| Yes (n=27) | No (n=67) |
|---|
| Sex | Male (n=48) | 22 (45.8) | 26 (54.2) | <0.001 |
| Female (n=46) | 5 (10.9) | 41 (89.1) |
| Age groups | <20 (n=2) | 0 (0) | 2 (100) | 0.226 |
| 20-35 (n=62) | 20 (32.3) | 42 (67.7) |
| 35-50 (n=17) | 6 (35.3) | 11 (64.7) |
| >50 (n=13) | 1 (7.7) | 12 (92.3) |
| Occupation | Student (n=13) | 3 (23.1) | 10 (76.9) | 0.957 |
| Professional (n=58) | 17 (29.3) | 41 (70.7) |
| Non- Professional (n=19) | 6 (31.6) | 13 (68.4) |
| Non-working/Housewife (n=4) | 1 (25) | 3 (75) |
| Place | Urban (n=69) | 19 (27.5) | 50 (72.5) | 0.428 |
| Rural (n=25) | 8 (32) | 17 (68) |
*p-value <0.05 statistically significant
Discussion
In India, there is still a paucity of community based studies on assessing the empowerment of patients on hand hygiene using WHO questionnaire. Most of the studies in India were assessing the hand hygiene practices among HCWs [15,16] however, they failed to capture the patient’s empowerment on hand hygiene and the barriers encountered by them.
Increasing patient participation and their empowerment to improve HCW hand hygiene compliance showed inconsistent results in many studies [7-12]. Similarly several studies have observed obstacles to patients’ in challenging HCW regarding hand hygiene [8–12,17-19]. Our study mainly focuses on empowerment and understanding the various barriers that exist to patients on increasing the hand hygiene compliance among HCWs and also to suggest measures to overcome potentially from those barriers with technological prompts.
In the present study, almost all respondent ever visited hospital in their life time; among them 86.2% of the respondents were visited hospitals within one year. Only less than one fourth of them visited hospitals within one month. Similar observations were reported by Michaelsen K et al., that is 98% of the respondent visited hospital more than one year and only 26.4% of them visited within past one month [12].
It was important that HCWs clean their hands routinely, however in the event that patients realized that the HCWs had not cleaned their hands, they would less frequently seek health care to that HCWs. In the present study, nearly half of the respondent reported the non compliance on hand hygiene among HCWs. Similar observations were reported by Michaelsen K et al., and Longtin Y et al., [12,17]. Though discussing hand hygiene practices with physicians would decrease hospital acquired infections, the majority of patients did not challenge their physicians to clean their hands due to various barriers. In this present study, 71% of the respondent never asked their HCWs to wash/sanitize their hands before examination, however this observation was higher than the study conducted by Michaelsen K et al., (12%) and Safdar N et al., (9.5%) [12,20]. To challenge the physician regarding hand hygiene there were significant difference observed between male and female respondents and the major barrier stated in the present study was fear and being disrespectful, which was similar to Michaelsen K et al., and Longtin Y et al., in the present study [12,17].
Majority of the respondents were not comfortable to ask HCWs to wash/sanitize their hands even when HCWs did not remind them. To add-up, awareness regarding hospital acquired infections was low among the respondent and also significant difference was found among male and female. This suggests that there is an urgent need for tools that encourage patients to discuss hand hygiene with their doctor.
Though the awareness regarding hospital acquired infections were similar to both urban and rural respondent, commonly the non compliance on hand hygiene among HCWs were reported by urban respondents with a significant difference (p=0.004).
Community plays an important role in implementing the programme. Only 27.7% of the respondents reported that they were having programmes related to the hand hygiene in their community. This shows the lack of awareness regarding the dreadful hospital acquired infections in the community.
Respondents were asked for the best tool for BCC, most of them reported that demonstration by HCWs were effective, which correlates with the previous work [8]. In the present study, respondents were also reported creating awareness from the schools were most important to overcome the inhibitions to discuss about hand hygiene and also media and visual aids play a vital role to help the patients by creating awareness regarding hand hygiene. These reports were similar to other studies that used visual prompts of various types including posters and information packets for creating awareness among patients and specifically for those patients who feel too shy to speak up regarding hand hygiene [7-11]. Most of the respondents felt that HCWs were solemnly responsible for creating BCC regarding hand hygiene, with least involvement of community.
Limitation
It was an online based study which relied on a voluntary convenience sampling of the respondents who were using internet. The present study was conducted in a short time, the response rate among the online users was low. Only 24.5% of the respondents visited hospital within a month, others visited a hospital a month later which leads to potential recall bias. As it was an online based survey, we are not able to obtain the full socio-demographic details regarding the participants. It is feasible and appropriate results would be obtained if the patients from different hospital settings and geographical area were included.
Conclusion
In this present study, we found that most patients were not aware of the risks of health care associated infections and identify them at risk for contracting hospital acquired infections. Also adherence and empowerment on hand hygiene practices is suboptimal among people. To improve the compliance of hand hygiene practices among HCWs, one should focus in multimodal and multidisciplinary approaches. Patients play an important role to improve the hand hygiene compliance among HCWs. There seems to be a lack of knowledge regarding hand hygiene. Hand hygiene is an important practice, to reduce the risk and spread of infection in the health sector. In service education, information leaflets, automated dispensers, and performance feedback on hand hygiene adherence rates need to be associated with further improvements.
*p-value <0.05 statistically significant
*p-value <0.05 statistically significant
*p-value <0.05 statistically significant
*p-value <0.05 statistically significant
*p-value <0.05 statistically significant
*p-value <0.05 statistically significant