Unless contraindicated, spinal anaesthesia is the preferred mode of anaesthesia in patients undergoing surgeries of lower limbs. Used alone in spinal anaesthesia, hyperbaric bupivacaine 0.5% is associated with relatively short duration of action leading to the need to rescue with general anaesthesia if the surgical procedure exceeds beyond the drug’s duration of action [1]. Over the years many drugs have been used as an additive to spinal anaesthesia in order to hasten its onset of action, decrease the time to surgical incision, prolong the duration of action and to provide adequate postoperative analgesia. These drugs include midazolam, ketamine, fentanyl, clonidine [2,3], many opioids and non opioids. Use of opioids is associated with its side effects like pruritis, nausea, vomiting, constipation, and respiratory depression which can be distressing for the patient [4].
In this study, we aim to compare the efficacy of two different doses (3 μg and 5 μg) of dexmedetomidine given in combination with 0.5% hyperbaric bupivacaine via intrathecal route in orthopaedic patients undergoing lower limb surgeries with regards to the haemodynamic stability, incidence of side effects (hypotension and bradycardia) and postoperative analgesia.
Materials and Methods
The study was a prospective randomized clinical trial conducted at Sikkim Manipal Institute of Medical Science, Gangtok, Sikkim, India. After the approval of the Ethical Committee of the Institute, 60 ASA Grade I and II orthopaedic patients between the ages of 20 to 60 years who were undergoing lower limb surgeries were included in the study. Sample size was based on previous study [7] and determined using MedCalc software version 16.2.1. All patients were screened in the pre anaesthesia clinic prior to taking up for surgery. Written consent was taken from all the patients enrolled in the study. Uncooperative patients, patients with uncontrolled hypertension and diabetes, patients with allergy to the study drugs, patients with height less than 150 cm and patients having condition which are contraindication to spinal anaesthesia such as patient refusal, infection at site of injection, coagulopathy, increased intracranial pressure were excluded from the study [Table/Fig-1].
Flow chart of patient inclusion/exclusion criteria.
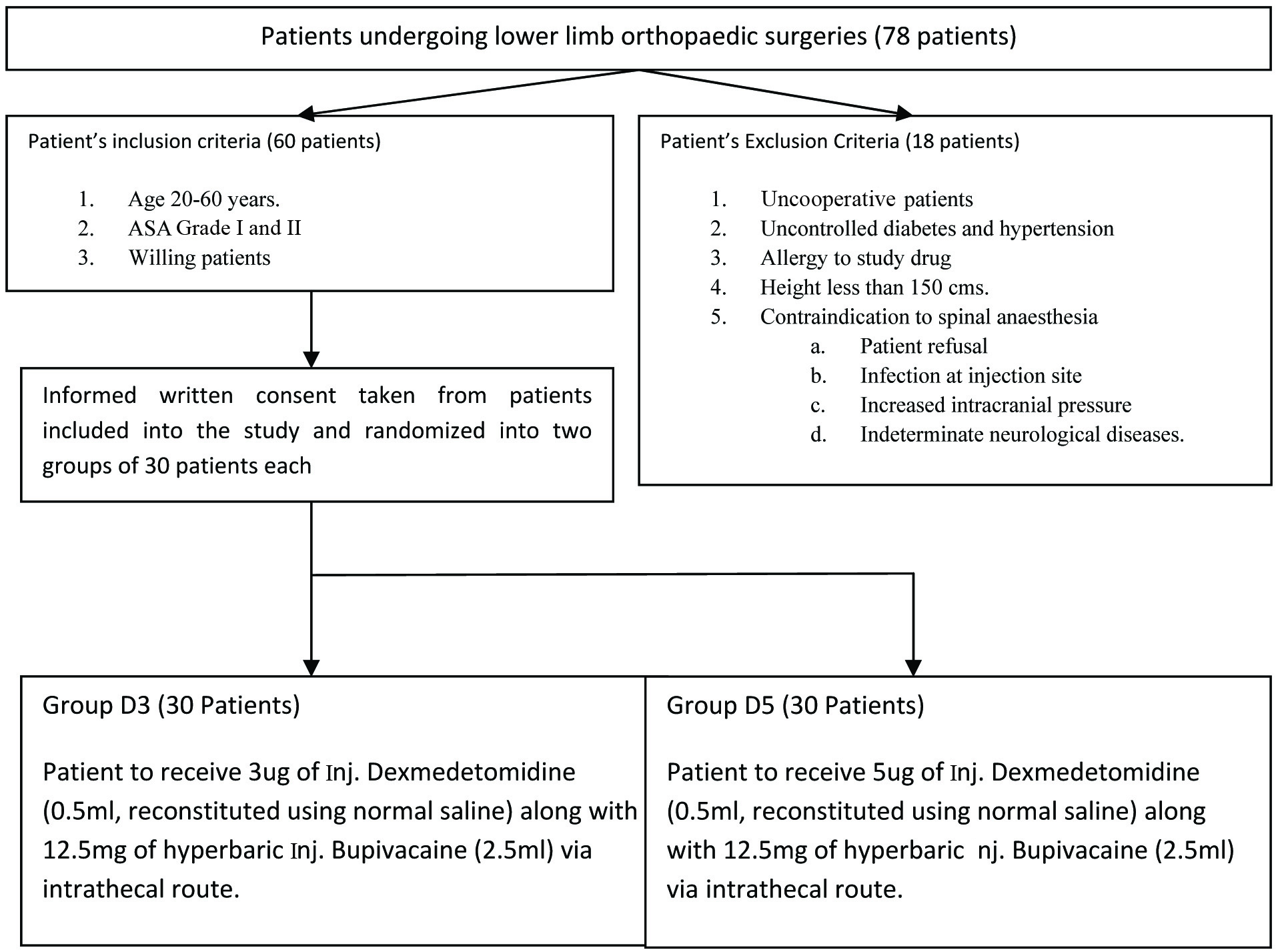
The patients were randomized into two groups of 30 patients; Group D3 and Group D5 using a computer generated random number table. All patients in Group D3 received 12.5 mg of 0.5% hyperbaric bupivacaine along with 3 μg of Inj. Dexmedetomidine (0.5 ml, reconstituted with normal saline) while patients in Group D5 received 5 μg of inj. Dexmedetomidine (0.5 ml, reconstituted with normal saline) along with 12.5 mg of 0.5% hyperbaric bupivacaine. The total volume of study drug was kept constant in all 60 patients (3 ml). The anaesthesiologist performing the procedure as well as the patient enrolled into the study were blinded from the study drug.
Prior to performing lumber puncture, standard monitoring including electrocardiography, pulse oximetry and non invasive blood pressure measurement was done and patient was co-loaded with 15 ml/kg body weight of ringer lactate. Lumbar puncture was done using 25 gauge Quinke spinal needle via median approach in L3-L4 intervertebral space with patients in sitting position under full aseptic precaution. Successful placement of spinal needle in sub arachnoids space was confirmed by aspiration of cerebrospinal fluid and the study drug was injected over 10 second period and the patients were placed supine after the drug was injected.
The sensory and motor blockade was tested every two minutes after the injection of drug till the attainment of the highest level of block. Haemodynamic monitoring was done every two minutes for the first 10 minutes and subsequently every 15 minute till the end of surgery using an automated multichannel monitor. The sensory blockade was tested by pin prick along the midclavicular line and the motor blockade was assessed as per the Bromage scale [8]; (Grade 1: free movement of legs and feet, Grade 2: Just able to flex knees with free movement of feet, Grade 3: Unable to flex knees, but with free movement of feet, Grade 4: Unable to move legs or feet) [Table/Fig-2].
Description of bromage scale [8].
| Grade | Criteria | Degree of block |
|---|
| 1 | Free movement of legs and feet | Nil (0%) |
| 2 | Just able to flex knees with free movement of feet | Partial (33%) |
| 3 | Unable to flex knees, but with free movement of feet | Almost complete (66%) |
| 4 | Unable to move legs or feet | Complete (100%) |
Fall in systolic blood pressure to less than 90 mm Hg or less than 30% of baseline value was defined as hypotension and was treated with Inj. Mephenteramine 3 mg bolus doses in increments. Similarly, bradycardia was defined as fall in heart rate to less than 60 beats per minutes and treated with Inj. Atropine 0.3 mg bolus doses. After the end of surgery, patient was shifted to the Post Anaesthesia Care Unit (PACU) and was discharged from PACU once the modified aldret score was nine or more [9].
Data recording were done for Time to reach the Highest Level of Sensory Block (TTHSB), Time to reach the best motor blockade (Bromage scale of 4) (TTBS4), Time To Surgical Incision after giving spinal anaesthesia (TTSI), changes in haemodynamics, Total Duration Of Surgery (TDOS) incidence of side effects and time to first rescue analgesia postoperatively (TTFRA).
All the data’s were analysed using IBM SSPE statistical software version 23.0. Mean±SD and unpaired t-test were used for statistical analysis and comparison of age, TTHSB, TTBS4, TTSI, TDOS and TTFRA between the two groups with a p-value of less than 0.05 was considered significant. Chi-square test was used for qualitative data analysis.
Results
The two groups analysed were similar in terms of demographic profile including patients’ age, sex, weight and height with no statistically significant difference [Table/Fig-3]. The mean time to reach highest sensory block (T10) dermatome was similar in both groups, 3.34 minutes±0.37 (D3)/ 3.48 minutes±0.34 (D5) while the time to reach Bromage scale 4 was 5.12±0.46 minutes in D3 and 4.9±0.37 minutes in D5 which was also statistically insignificant. The time to surgical incision after spinal anaesthesia was 23.57±4.22 minutes in Group D3 while in Group D5 the same was 24.53±4.22 minutes (statistically not significant). The total duration of surgery was almost similar in both Groups (153.07 minutes (D3 group): 149.97 minutes (D5 Group) [Table/Fig-4].
| Criterion | Group D3 | Group D5 | p value (< 0.05) |
|---|
| Age (years) | 36.33±11.604 | 41.77±12.62 | 0.088 |
| Sex (Male: Female) | 21:9 | 16:14 | - |
| Weight (Kgs) | 64.4±8.20 | 66.40±7.15 | 0.257 |
| Height (Cms) | 158.09±4.29 | 159.27±4.07 | 0.10 |
| ASA (I:II) | 23:7 | 21:9 | - |
Group D3= Dexmed 3 μg; Group D5= Dexmed 5 μg; ASA= American society of Anaesthesiologist: Students t-test was used for analysis of Age, weight and height with a p-value of < 0.05 considered significant while Chi-Square test was used for evaluation of sex and ASA status.
Summary of various parameters analysed.
| Criterion | Group D3 | Group D5 | p-value (< 0.05) |
|---|
| TTHSB (mins) | 3.34±0.37 | 3.48±0.34 | 0.534 |
| TTBS4 (mins) | 5.12±0.46 | 4.90±0.37 | 0.088 |
| TTSI (mins) | 23.57±4.22 | 24.53±4.22 | 0.378 |
| TDOS (mins) | 153.07±16.61 | 149.97±17.55 | 0.485 |
| TTFRA (mins) | 206.47±18.86 | 271.33±16.83 | 0.001 |
| Hypotension | 3 | 3 | - |
TTHSB= time to highest sensory block (T10); TTBS4 = time to Bromage scale 4; TTSI = time to surgical incision; TDOS = total duration of surgery; TTFRA = time to first rescue analgesia after skin closure. Students t-test was used for analysis of above parameters with a p-value of < 0.05 considered significant.
The change in haemodynamics was similar (p>0.05) and gradual in both the groups with a fall in blood pressure and heart rate in the first 10 minutes after spinal anaesthesia and a steady course there after with slight increase towards the end of surgery as the effect of the drugs begin to wear down [Table/Fig-5,6 and 7]. Similar results were noted in mean arterial pressure [Table/Fig-8]. Two patients each in both the groups needed one rescue bolus dose of Inj. Mephenteramine 3 mg to treat fall in systolic blood pressure less than 90 mmHg.
Comparison of mean heart rate between two groups.
| Criterion | Group D3 | Group D5 | p-value (<0.05) |
|---|
| Pre-Op | 88.9 | 86.9 | 0.48 |
| 2 Min | 86.9 | 84.9 | 0.44 |
| 4 Min | 85.2 | 85.0 | 0.95 |
| 6 Min | 83.4 | 83.0 | 0.85 |
| 8 Min | 81.6 | 80.8 | 0.74 |
| 10 Min | 80.4 | 79.6 | 0.71 |
| 15 Min | 79.5 | 79.3 | 0.92 |
| 30 Min | 77.9 | 77.9 | 0.97 |
| 45 Min | 77.2 | 77.3 | 0.99 |
| 60 min | 76.5 | 77.7 | 0.60 |
| EOS | 76.7 | 77.1 | 0.87 |
D3= Dexmedetomidine 3 μg; D5= Dexmedetomidine 5 μg; EOS= end of surgery. p-value calculated using Student’s t-test with a p-value of <0.05 considered statistically significant.
Comparison of mean systolic blood pressure between two groups.
| Criterion | Group D3 | Group D5 | p-value (<0.05) |
|---|
| Pre-Op | 129.1 | 133.2 | 0.07 |
| 2 Min | 126.9 | 128.1 | 0.45 |
| 4 Min | 122.2 | 125.1 | 0.07 |
| 6 Min | 120.9 | 122.7 | 0.30 |
| 8 Min | 116.4 | 119.5 | 0.19 |
| 10 Min | 115.9 | 117.5 | 0.37 |
| 15 Min | 112.2 | 113.4 | 0.47 |
| 30 Min | 112.2 | 112.5 | 0.90 |
| 45 Min | 107.7 | 112.1 | 0.23 |
| 60 min | 110.4 | 111.8 | 0.49 |
| EOS | 120.9 | 123.3 | 0.32 |
D3= Dexmedetomidine 3 μg; D5= Dexmedetomidine 5 μg; EOS= end of surgery. p-value calculated using Student’s t-test with a p-value of <0.05 considered statistically significant.
Comparison of mean diastolic blood pressure between two groups.
| Criterion | Group D3 | Group D5 | p-value (<0.05) |
|---|
| Pre-Op | 76.8 | 79.1 | 0.47 |
| 2 Min | 78.9 | 77.9 | 0.67 |
| 4 Min | 75.5 | 76.2 | 0.75 |
| 6 Min | 73.3 | 74.2 | 0.70 |
| 8 Min | 69.9 | 70.9 | 0.66 |
| 10 Min | 71.4 | 70.7 | 0.75 |
| 15 Min | 68.9 | 67.5 | 0.49 |
| 30 Min | 68.9 | 67.9 | 0.66 |
| 45 Min | 68.2 | 68.0 | 0.95 |
| 60 min | 67.4 | 67.9 | 0.79 |
| EOS | 71.9 | 73.1 | 0.58 |
D3= Dexmedetomidine 3 μg; D5= Dexmedetomidine 5 μg; EOS= end of surgery. p-value calculated using Student’s t-test with a p-value of <0.05 considered statistically significant.
Comparison of mean MAP between the two groups.
| Criterion | Group D3 | Group D5 | p-value (<0.05) |
|---|
| Pre-Op | 97.1 | 98.3 | 0.57 |
| 2 Min | 96.1 | 96.2 | 0.94 |
| 4 Min | 92.6 | 93.9 | 0.45 |
| 6 Min | 90.4 | 91.8 | 0.46 |
| 8 Min | 86.8 | 88.7 | 0.35 |
| 10 Min | 87.1 | 87.5 | 0.84 |
| 15 Min | 84.6 | 84.1 | 0.76 |
| 30 Min | 84.6 | 83.8 | 0.68 |
| 45 Min | 83.3 | 84.0 | 0.73 |
| 60 min | 82.6 | 83.9 | 0.49 |
| EOS | 90.4 | 91.6 | 0.53 |
D3= Dexmedetomidine 3 μg; D5= Dexmedetomidine 5 μg; EOS= end of surgery; MAP= mean arterial pressure. p-value calculated using Student’s t-test with a p-value of <0.05 considered statistically significant.
A statistically significant difference (p<0.001) was observed in time to first rescue analgesia after skin closure with Group D3 having 206.47 minutes while in Group D5 the time was 271.33 minutes [Table/Fig-4].
Discussion
In our study, we found that dexmedetomidine in a dose of 3 μg and 5 μg in 0.5 ml volume is an effective additive to hyperbaric bupivacaine 0.5% in spinal anaesthesia producing good haemodynamic stability during the intraoperative period and a prolonged postoperative analgesia. The dose dependent side effects of dexmedetomidine namely hypotension and bradycardia were not seen with doses of 3 μg and 5 μg; although, the duration of postoperative analgesia was significantly longer with dexmedetomidine in 5 μg dose compared to 3 μg doses.
Since its FDA approval for use in humans as a short term medication for sedation/analgesia in the intensive care unit, researchers have been exploring the prospect of using dexmedetomidine as an additive in spinal analgesia taking into advantage its highly selective agonistic action for intrathecal α2 receptors which have antinociceptive actions for both somatic and visceral pain [10]. Dexmedetomidine prolongs the sensory block by depressing the release of C fibres transmitters and by hyperpolarisation of post synaptic dorsal horn neurons [11,12].
In the study conducted by Shaikh SI and Dattatri R patients were randomly allocated into three groups of 30 patients each with the first group received 15 mg of 0.5% hyperbaric bupivacaine with normal saline, second group received 15 mg of hyperbaric bupivacaine with 5 μg and the third group received 15 mg of hyperbaric bupivacaine with 10 μg of dexmedetomidine with normal saline to a total volume of 3.5 ml [13]. They found that the mean time taken to attain sensory block of T10 dermatome and motor block of Bromage 4 grade was significantly rapid in second and third group as compared to bupivacaine group. The time taken for regression of sensory block and the time to first rescue analgesic also significantly increased by addition of dexmedetomidine in a dose dependent manner. The findings of our study were similar to that of Shaikh SI and Dattatri R with dexmedetomidine 5 μg added to hyperbaric bupivacaine producing a shorter time to attain a Bromage scale of 4 and a longer time to rescue analgesia as compared to dexmedetomidine 3 μg.
A meta analysis on the effect of different doses of intrathecal dexmedetomidine on spinal anaesthesia conducted by Zhang Y et al., which included nine studies with Jaded score of 3-5 on various doses of dexmedetomidine concluded that the action of spinal anaesthesia may be prolonged by increasing the dose of intrathecal dexmedetomidine but the risk of bradycardia is increased at the same time [14]. In our study, the incidence of hypotension and bradycardia was not significant with dexmedetomidine being used in 3 μg and 5 μg doses intrathecally but the duration of postoperative analgesia was comparable to that achieved by higher doses of dexmedetomidine as in other studies.
Study conducted by Nayagam HA et al., concluded that dexmedetomidine in a dose of 5 μg is ideal for use as an additive in spinal anaesthesia [2]. The findings of our study are on a similar line with 5 μg dose producing a prolonged duration of postoperative analgesia compared to dexmedetomidine in 3 μg dose.
Study conducted by Sudheesh K et al., used dexmedetomidine in doses of 3 μg and 5 μg as an additive to spinal anaesthesia in patients undergoing ambulatory perianal surgeries and found the changes in haemodynamic parameters during the intraoperative period were similar in both the groups with overall gradual decrease in haemodynamic parameters below the baseline value [7]. We have reported a similar pattern of haemodynamic changes in our study.
All patients enrolled into the study were followed up in orthopaedics outpatient department for a period of six months from the completion of study and were not found to have any neurological sequelae which could otherwise be attributed to intrathecal dexmedetomidine administration.
Limitation
The sample size was small and as all the lower limb orthopaedic cases were included in the study, the duration of surgery was not uniform. The limitation of study could have been reduced if only one type of lower limb orthopaedic cases were included in the study to ensure uniformity in the duration of surgery and time to first rescue analgesia.
Conclusion
Dexmedetomidine is an effective additive to spinal anaesthesia which provides a stable haemodynamics and prolonged postoperative analgesia. Used in a dose of 5 μg (in 0.5 ml volume) maximal beneficial effect of dexmedetomidine can be obtained.
Group D3= Dexmed 3 μg; Group D5= Dexmed 5 μg; ASA= American society of Anaesthesiologist: Students t-test was used for analysis of Age, weight and height with a p-value of < 0.05 considered significant while Chi-Square test was used for evaluation of sex and ASA status.
TTHSB= time to highest sensory block (T10); TTBS4 = time to Bromage scale 4; TTSI = time to surgical incision; TDOS = total duration of surgery; TTFRA = time to first rescue analgesia after skin closure. Students t-test was used for analysis of above parameters with a p-value of < 0.05 considered significant.
D3= Dexmedetomidine 3 μg; D5= Dexmedetomidine 5 μg; EOS= end of surgery. p-value calculated using Student’s t-test with a p-value of <0.05 considered statistically significant.
D3= Dexmedetomidine 3 μg; D5= Dexmedetomidine 5 μg; EOS= end of surgery. p-value calculated using Student’s t-test with a p-value of <0.05 considered statistically significant.
D3= Dexmedetomidine 3 μg; D5= Dexmedetomidine 5 μg; EOS= end of surgery. p-value calculated using Student’s t-test with a p-value of <0.05 considered statistically significant.
D3= Dexmedetomidine 3 μg; D5= Dexmedetomidine 5 μg; EOS= end of surgery; MAP= mean arterial pressure. p-value calculated using Student’s t-test with a p-value of <0.05 considered statistically significant.