Pseudo Aneurysm of Aberrant Right Gastroepiploic Artery Mimicking Pseudocyst of Pancreas– A Rare Case Report
Abhinav Jauhari1, Ambuj Shrivastava2, Rajesh Kumar Soni3, Ashutosh Darbari4
1 Senior Resident, Department of Surgery, V.M.M.C. and Safdarjung Hospital, New Delhi, India.
2 Postgraduate Student, Department of Radio diagnosis, Sri Devarajurs Medical College, Kolar, Karnataka, India.
3 Professor, Department of Surgery, V.M.M.C. and Safdarjung Hospital, New Delhi, India.
4 Associate Professor, Department of Surgery, Chirayu Medical College, Bhopal, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Abhinav Jauhari, Flat No. 903, B2 Tower, Gardenia Glory, Sector 46, Noida-201303, Uttar Pradesh, India.
E-mail: abhinavjauhari05@gmail.com
Pseudoaneurysm of peripancreatic vessel is a rare complication of pancreatitis. The splenic artery is the most commonly affected vessels close to the pancreas. Pseudoaneurysm of right gastroepiploic artery is rare. It can rupture into Gastro Intestinal (GI) tract, retroperitoneum, peritoneal cavity, biliopancreatic duct or pseudocyst. Clinical diagnosis of unruptured pseudoaneurysm is rarely possible because there are no specific signs and symptoms. We hereby report a case of pseudoaneurysm of aberrant right gastroepiploic artery in 30-year-old male which presented with history of epigastric pain and lump with episode of haematemesis and malena. Diagnosis was suspected on Doppler Ultrasonography (USG), which was later confirmed by CECT and angiography. Patient was treated by coil embolization. The pain and lump in epigastrium disappeared within five to six days. Patient is symptom free after six months of follow up.
Embolization, Haematemesis, Pancreatitis
Case Report
A 30-year male presented with history of pain in epigastrium and haematemesis since seven days. He was having melena since last four days. Pain was severe in intensity and was radiating to the back. History of excessive intake of alcohol seven days back was present. Patient was a known case of recurrent pancreatitis having history of repeated admissions for upper abdominal pain at our center. Patient was chronic alcoholic since last 12 years.
Clinical examination revealed tachycardia, hypotension, pallor, mild dyspnea and dehydration. Abdomen was tender and a lump was palpable in the epigastric region. The surface was smooth with well defined margins. The lump was not moving with respiration. A clinical diagnosis of recurrent pancreatitis with pseudocyst formation with septic shock was made. He was put on standard conservative treatment.
On investigation his haemoglobin was 7.2 gm/dl, pancreatic enzymes were raised (serum amylase 521 U/L, serum lipase 418U/L) and liver function tests were within normal limits. Plain abdomen radiograph showed no abnormality. USG abdomen with Doppler was suggestive of ananechoic mass in the head of pancreas with posterior acoustic enhancement and comparatively hyperechoic margins. The mass showed internal vascularity on colour Doppler with “to and fro” pattern on pulsed Doppler. The above findings were suspicious of pseudoaneurysm in the region of gastroduodenal artery likely due to regional inflammatory process in pancreatitis.
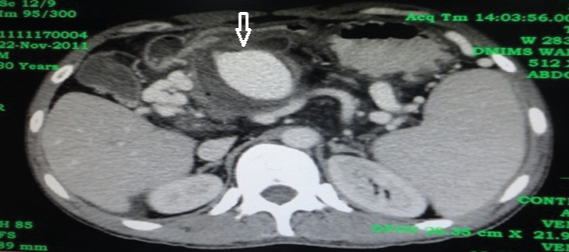
Contrast Enhanced Computed Tomography (CECT) was done to confirm the diagnosis. It revealed round to oval lesion in the region of neck and head of pancreas in the area of gastroduodenal artery showing contrast filling during the arterial and venous phase similar to that of a vessel, highly suggestive of pseudoaneurysm of peripancreatic vessel [Table/Fig-1].
CECT arterial phase demonstrating aneurysm.
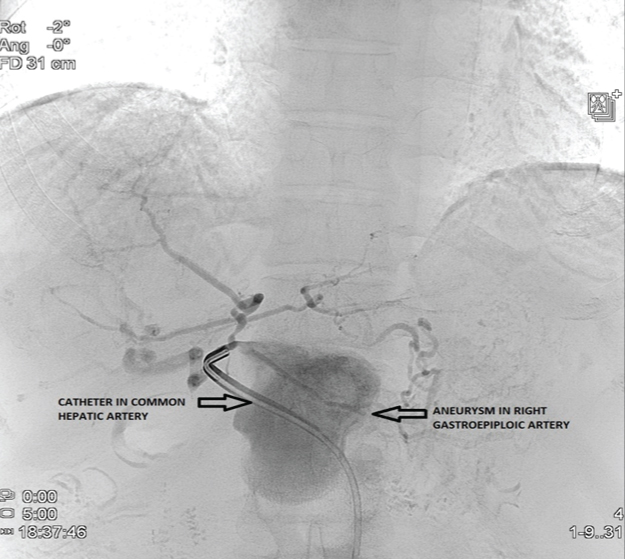
Conventional peripheral angiography (Trans femoral route) was done which demonstrated pseudoaneurysm of right gastroepiploic artery which was directly coming from common hepatic artery instead of arising from gastro duodenal artery (Aberrant origin) [Table/Fig-2].
Pre coiling angiogram of aneurysm.
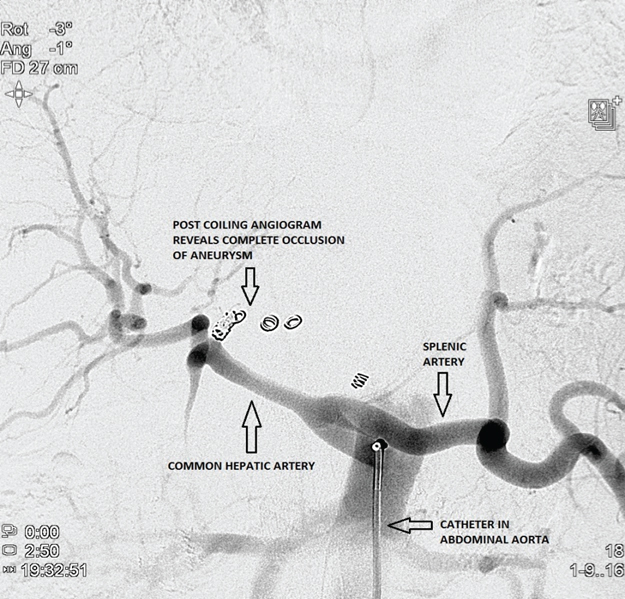
After confirming the presence of pseudoaneurysm, coil embolization of the aneurysm was performed in the same sitting by experienced radiological interventionist. Patient showed remarkable improvement after embolization procedure as good obliteration was achieved [Table/Fig-3]. The lump reduced in size, haematemesis stopped and stools became normal in colour. Patient was discharged after six days of procedure. The lump has completely disappeared and the patient is asymptomatic for last six months.
Post coiling angiogram showing complete occlusion of aneurysm.
Discussion
Visceral vessels are the sixth most common site for aneurysmal degeneration. Splenic artery is the commonest vessel followed by the hepatic artery, celiac artery, and more rarely other visceral arteries [1].
Pseudoaneurysm of peripancreatic vessels is an uncommon, but serious complication of pancreatitis [2]. A 10% of patients with chronic pancreatitis develop pseudoaneurysm with rupture occurring in 50% of them [3]. Pancreatitis with secondary pseudocyst is the most common cause of pseudoaneurysms, although they can occur even in the absence of a pseudocyst. Location of pseudoaneurysm depends on the fluid collection and pseudocyst in pancreatitis.
Two different mechanisms have been proposed for the development of pseudoaneurysm. It can develop either due to proteolytic digestion of the arterial wall or by erosion of a pseudocyst into a nearby vessel and conversion of its cavity into a pseudoaneurysm [3]. Splenic artery being in close proximity to the body of pancreas is most often involved followed by gastroduodenal, and pancreaticoduodenal [4]. Together they account for up to 90% of cases of pseudoaneurysms [5]. Pseudoaneurysm of aberrant right gastroepiploic artery is very rare [6].
Unruptured pseudoaneurysms are usually asymptomatic. Complications include rupture into the gastrointestinal tract, peritoneal cavity, retroperitoneum or pancreatic duct causing the lethal haemorrhage. Rupture into the gastrointestinal tract is commonest of all [7].
Increased risk factors for bleeding in pancreatitis include duration of disease; proximity of a vessel to pseudocyst; communication with the bile or pancreatic duct and splenic vein thrombosis [3]. One of the risk factors and chronicity of disease was present in our patient.
Signs and symptoms are nonspecific and therefore clinical diagnosis is rarely possible.
A bleeding pseudoaneurysm may manifest as gradually increasing anaemia with melena or as intermittent massive bleeding into the gastrointestinal tract [3]. Rupture into a pseudocyst or into peritoneal cavity may present with acute abdomen and shock. Our patient presented with haematemesis and melena because the pseudoaneurysm was located in head of pancreas, in close proximity of duodenum.
Prompt diagnosis and appropriate management of this rare complication is critical as it is associated with a mortality rate of 90% without treatment and 29% even with treatment [5].
USG abdomen is the baseline investigation but the findings are usually nonspecific. Colour doppler can help in the diagnosis by showing internal vascularity as in this case. CECT will show contrast filling during the arterial and venous phase. Angiography remains the gold standard for imaging of pseudoaneurysms [8] with additional advantage for guiding therapeutic embolization.
Optimal treatment of bleeding pseudoaneurysm remains debatable [9]. Treatment options include angiographic embolization and surgical ligation of the pseudoaneurysm with or without pancreatic resection. Aneurysm trapping by embolizing proximal and distal to the aneurysm is recommended for successful outcome.
Some authors suggest initial embolization of pseudoaneurysms as the treatment of choice with subsequent surgical intervention in case of recurrent haemorrhage [5]. Reported success rate of embolization is 60%-100% with mortality of 12%-33% [10]. We successfully embolised the lesion during angiography in the same sitting resulting in complete recovery.
Conclusion
In a patient of pancreatitis, a lump in epigastrium is usually due to pseudocyst formation. Pseudoaneurysm presenting as lump is a rare but dangerous complication. Rupture of pseudoaneurysm may result in mortality if not detected and treated timely, so this rare but important complication should always be kept in mind during evaluation of epigastric lump in a case of pancreatitis. Angiography is the gold standard for imaging pseudoaneurysm and embolization of the bleeding vessel can be a life saving procedure.
[1]. Baker KS, Tisnado J, Cho SR, Beachley MC, Splanchnic artery aneurysms and pseudoaneurysms: transcatheter embolizationRadiology 1987 163:135-39. [Google Scholar]
[2]. Kandel BP, Ghimire B, Lakhey PJ, Shrestha UK, Khakurel M, Upper gastrointestinal bleeding in chronic pancreatitisJournal of Institute of Medicine 2010 32:247-50. [Google Scholar]
[3]. Lee HS, Park JJ, Kim CD, Ryu HS, Hynu JH, Pseudoaneurysm and splenic infraction in chronicpancreatitisJ Kor Med Sces 1996 11:183-87. [Google Scholar]
[4]. Tessier DJ, Stone WM, Fowl RJ, Abbas MA, James C, Clinical features and management of splenic artery pseudo aneurysm: Case series and cumulative review of literatureJournal of Vascular Surgery 2003 38(5):969-73. [Google Scholar]
[5]. Johnson C, Chahin C, Rose B, Goyal M, Ruptured intracystic pseudoaneurysm of the left gastric artery, which complicated pancreatitisApplied Radiology 2008 37(2) [Google Scholar]
[6]. Pillay WR, Lalloo S, Thomson SR, Conrads MA, Embolisation of metachronous pseudoaneurysms complicating chronic pancreatitisHPB (Oxford) 2003 5(4):251-53. [Google Scholar]
[7]. Hourani SA, Al-Bdour MN, Rashaideh MA, Al-Nawayseh KR, Alasmar AA, Alkasasbeh MA, Pseudo aneurysm complicates pancreatic pseudocyst: importance of early detection and managementJ Surg Pak 2008 13:42-45. [Google Scholar]
[8]. Tessier DJ, Clinical features and management of splenic artery pseudo aneurysm: case series and cumulative review of literatureJ Vasc Surg 2003 38:969-74. [Google Scholar]
[9]. Bergert H, Hinterseher I, Kersting S, Leonhardt J, Bloomenthal A, Saeger HD, Management and outcome of haemorrhage due to arterial pseudoaneurysms in pancreatitisSurg 2005 137:323-28. [Google Scholar]
[10]. de Perrot M, Berney T, Buhler L, Delgadillo X, Mentha G, Morel P, Management of bleeding pseudoaneurysms in patients with pancreatitisBr J Surg 1999 86:29-32. [Google Scholar]