Primary Hypothyroid and Secondary Adrenal Insufficiency-Searching the Missing Link
Subhodip Pramanik1, Sayantani Chandra2, Pradip Mukherjee3, Subhankar Chowdhury4
1 Post Doctoral Trainee, Department of Endocrinology and Metabolism, IPGMER, Kolkata, West Bengal, India.
2 Postgraduate Trainee, Department of Otorhinolaryngology, IPGMER, Kolkata, West Bengal, India.
3 Associate Professor, Department of Endocrinology and Metabolism, IPGMER, Kolkata, West Bengal, India.
4 Professor and Head, Department of Endocrinology and Metabolism, IPGMER, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Subhodip Pramanik, Post Doctoral Trainee, Endocrinology and Metabolism, IPGMER, 242, AJC Bose Road, Kolkata-700071, West Bengal, India.
E-mail: subhodip.mck@gmail.com
Autoimmune diseases, Pituitary hyperplasia, Secondary hypothyroidism
A 10-year-old boy presented with poor scholastic performance and short height for last three years. He was gaining weight and developed facial puffiness for last three months. He was a student of class III and had history of poor appetite and constipation. Birth and developmental history were unremarkable.
On examination, he had puffy facies [Table/Fig-1], height 117 cm (< 3rd percentile, Height age 6.5 years), weight 24 kg (50th percentile, Weight age 9 years), Grade 1b goiter, delayed relaxation of ankle jerk and one patch of vitiligo at his right leg. His vitals were stable. Testicular volume 3 ml bilateral and stretched penile length 4 cm, suggesting prepubertal status. Systemic examination revealed no abnormality. His investigations revealed normal blood counts, renal function and electrolytes. His Thyroid Stimulating Hormone (TSH) was >150 uIU/ml, free thyroxin (FT4) was 0.4 ng/dl and Anti Thyroid Peroxidase Antibody (Anti TPO antibody) was 200 IU/ml (N<35 IU/ml) {by Chemiluminescence method, Immulite 1000 machine}. Radiograph left hand revealed bone age of one year [Table/Fig-2]. A diagnosis of primary autoimmune hypothyroidism was made and the patient was started on LT4 75 mg OD.
A child presenting with short stature and poor scholastic performance.

X-ray left wrist at presentation showing bone age one year.

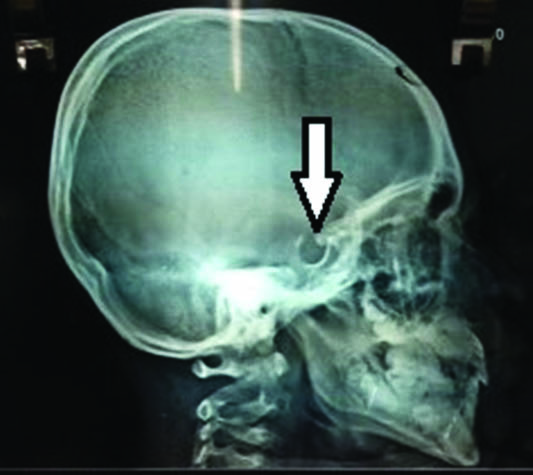
On first follow up after six weeks, his TSH came down to 9.75 uIU/ml and FT4 was 0.8 ng/dl but he was complaining of headache, dizziness and lethargy. Examinations revealed postural hypotension but no papilledema. A lateral X-Ray skull was done which revealed increased depth of sella turcica [Table/Fig-3].
Increased depth of sella turcica in X-ray skull lateral view (white arrow).
A possibility of feedback adenoma was considered and he was advised Magnetic Resonance Imaging (MRI) hypothalamic pituitary region and other anterior pituitary hormonal evaluation. His MRI on a later date revealed partially empty sella with thinned out pituitary tissue anchored in the floor of the sella [Table/Fig-4a,b] and paired serum cortisol and Adrenocorticotropic Hormone (ACTH) were 4.6 ug/dl and 4.2 pg/ml respectively. IGF 1 was normal and LH, FSH was prepubertal.
a) T2W MRI coronal view showing partially empty sella with thinned out pituitary tissue anchored in the floor of the sella (white arrow); b) T2W MRI sagittal view showing partially empty sella with thinned out pituitary tissue anchored in the floor of the sella (black arrow).
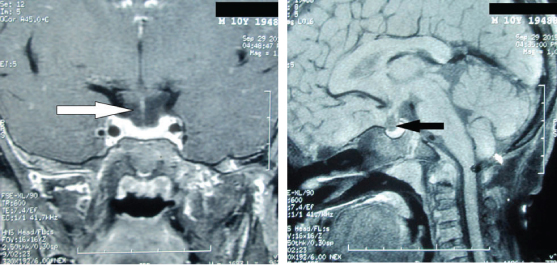
So the diagnosis was revised to primary hypothyroidism with empty sella syndrome with secondary adrenal insufficiency. Therapy was started with levothyroxine (LT4) 75 and T. hydrocortisone 5 mg at 8 am and 2.5 mg at 4 pm. Follow up strategy was formulated with periodic FT4 measurement and monitoring for signs of puberty. His facial appearance changed a lot [Table/Fig-5] and bone age advanced to three years [Table/Fig-6] after one year of therapy and still the patient is on treatment.
Facial appearance after one year of therapy.

X-ray left wrist after one year showing bone age three year.

Empty Sella (ES) is a common anatomical finding and has many causes like surgery, radiotherapy, infarction or sometimes it is idiopathic [1]. It is often associated with a hypofunctional disorder of one or more hormones due to insufficient residual anterior pituitary parenchyma. Therefore, most of the articles that link hypothyroidism with ES refer to secondary hypothyroidism (with reduced TSH) that may or may not be associated with other secondary hormone deficiencies [2]. Thus, our report of primary hypothyroidism associated with ES syndrome is unique in this regard.
However, this co-existent may not be entirely by chance. One such hypothesis is that the compensatory hyperplasia of pituitary, secondary to peripheral gland hypofunction may regress following replacement therapy, leading to cisternal herniation. In fact, several authors show that primary hypothyroidism results in an increased pituitary mass, which reverses after thyroxine replacement therapy [3]. However, in our patient we did not perform MRI prior to replacement therapy to demonstrate pituitary hyperplasia; still the increased depth of sella turcica in lateral X-Ray skull gives an indirect evidence of prior pituitary enlargement. Another possible explanation may be an almost simultaneous disorder of the pituitary and peripheral glands due to a similar pathogenic process. Autoimmune hypophysitis is often associated with either other autoimmune processes, particularly those involving the thyroid [4]. ES and primary hypothyroidism may be the outcome of the final progression of autoimmune hypophysitis and autoimmune thyroid disease. In the thyroid gland, this results in hypofunction and in the pituitary gland in a much reduced parenchyma favouring ES. As neither pituitary biopsy nor antipituitary antibody is easily available, detection in the first phase of autoimmune hypophysitis goes undetected in many patients. Recently, Manetti L et al., found antipituitary antibodies in 11.4% of 961 patients with autoimmune thyroid disorders; of whom eight had ES. We could not perform antipituitary antibody due to cost issues [5].
[1]. Bianconcini G, Bragagni G, Bianconcini M, Primary empty sella syndrome. Observations on 71 casesRecent Prog Med 1999 90:3-80. [Google Scholar]
[2]. Milosevic M, Stojanovic M, Nesovic M, Primary hypothyroidism associated with empty sella turcica and hypopituitarismMed Pregl 2005 58:410-13. [Google Scholar]
[3]. Larson NS, Pinsker JE, Primary hypothyroidism with growth failure and pituitary pseudotumor in a 13-year-old female: A case reportJournal of Medical Case Reports 2013 7:149-53. [Google Scholar]
[4]. Barbaro D, Loni G, Lymphocytic hypophysitis and autoimmune thyroid diseaseJ Endocrinol Invest 2000 23:339-40. [Google Scholar]
[5]. Manetti L, Lupi I, Morselli LL, Albertini S, Cosottini M, Grasso L, Prevalence and functional significance of antipituitary antibodies in patients with autoimmune and nonautoimmune thyroid diseasesJ Clin Endocrinol Metab 2007 92:2176-81. [Google Scholar]