A Case of Bilateral Corneal Perforation in a Patient with Severe Dry Eye
Jyoti Deswal1, Sudesh Kumar Arya2, Amit Raj3, Anubha Bhatti4
1 Junior Resident, Department of Ophthalmology, Government Medical College and Hospital, Chandigarh, India.
2 Professor, Department of Ophthalmology, Government Medical College and Hospital, Chandigarh, India.
3 Assistant Professor, Department of Ophthalmology, Government Medical College and Hospital, Chandigarh, India.
4 Senior Resident, Department of Ophthalmology, Government Medical College and Hospital, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jyoti Deswal, H.No. 25/10 –A, Jasbir Colony, Near Sheela Bypass, Rohtak-124001, Haryana, India.
E-mail: jyoti_deswal@yahoo.co.in
Dry eye is a common problem affecting mainly the adult population. In severe cases, it can result in sterile corneal ulcer and perforation. We report a rare case of a 26-year-old male, a known patient of severe dry eye who presented with sterile corneal ulcer with corneal perforation in both the eyes. The patient was managed by applying cyanoacrylate glue and bandage contact lens in both eyes and topical antibiotic, topical cyclosporine and preservative free artificial tears at two hourly intervals. The patient was investigated for the systemic cause of severe dry eye but no cause could be ascertained. On follow up, the patient reported marked relief in photophobia. On examination, both eyes showed sealed perforation with well formed anterior chamber. In conclusion, one should examine a dry eye patient carefully and detect corneal ulcers and perforations in time so as to prevent its sequelae.
Anterior chamber, Cyanoacrylate glue, Photophobia
Case Report
A 26-year-old male presented to the outpatient department with complaints of painful decrease in vision in both the eyes for the past seven days. The decrease in vision was associated with photophobia and redness, more in left eye than right. There was no history of any trauma to any eye.
On evaluation of his records, the patient was found to be a known case of severe dry eye, diagnosed two years earlier, for which he had taken treatment in the form of artificial tears and topical fluorometholone 0.1% occasionally for five to six months, but patient was off drugs for the past one and a half year.
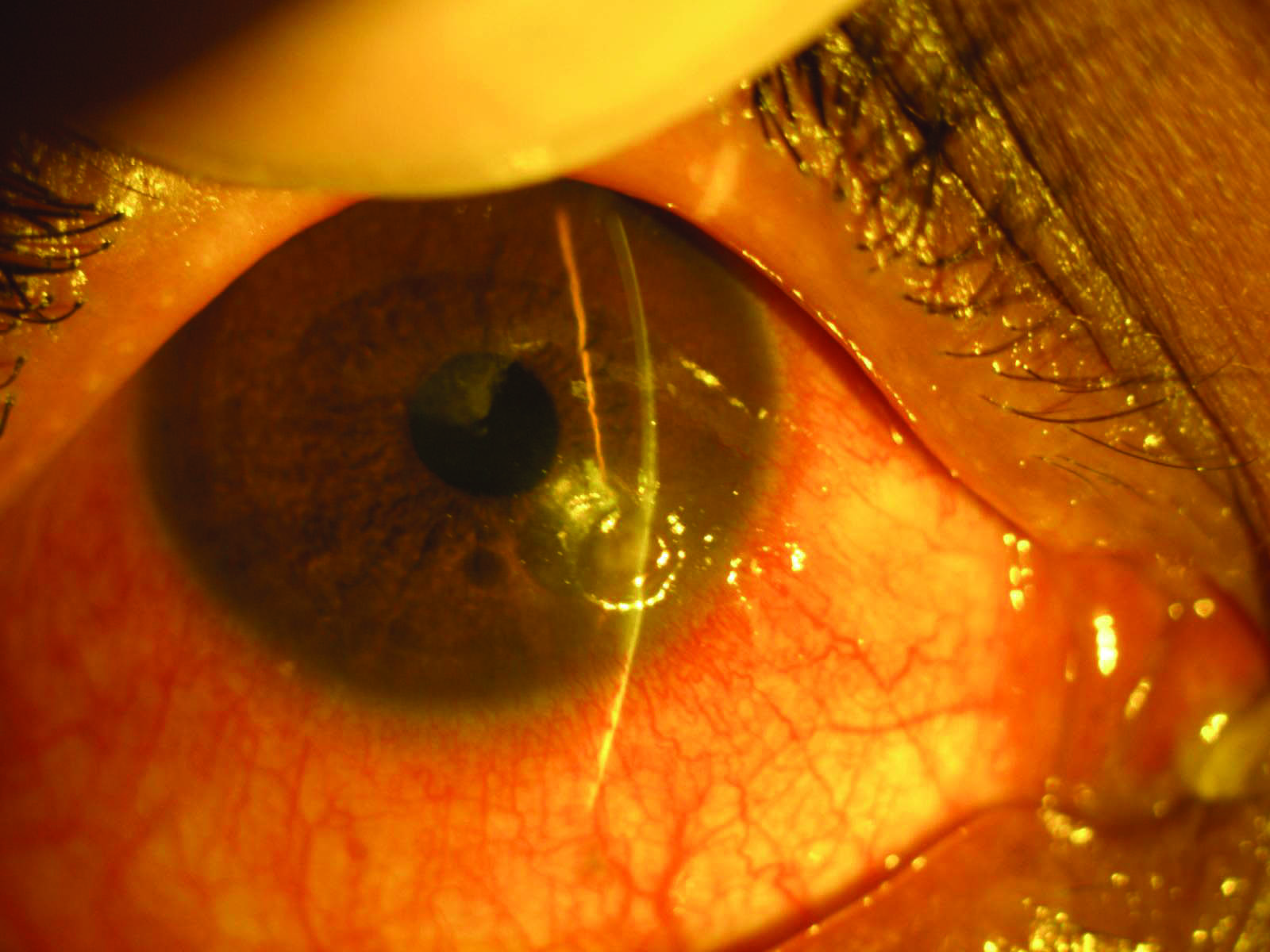
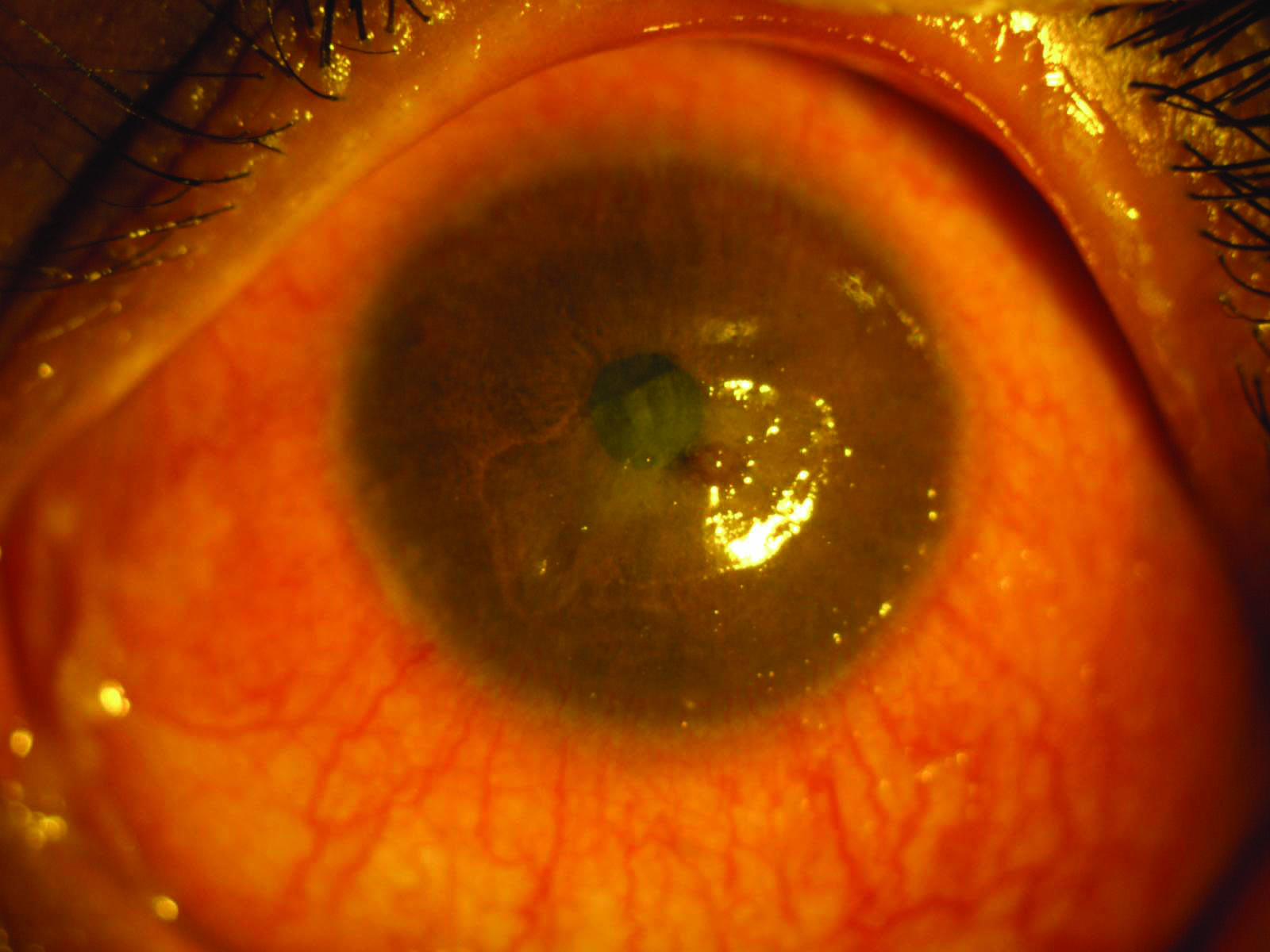
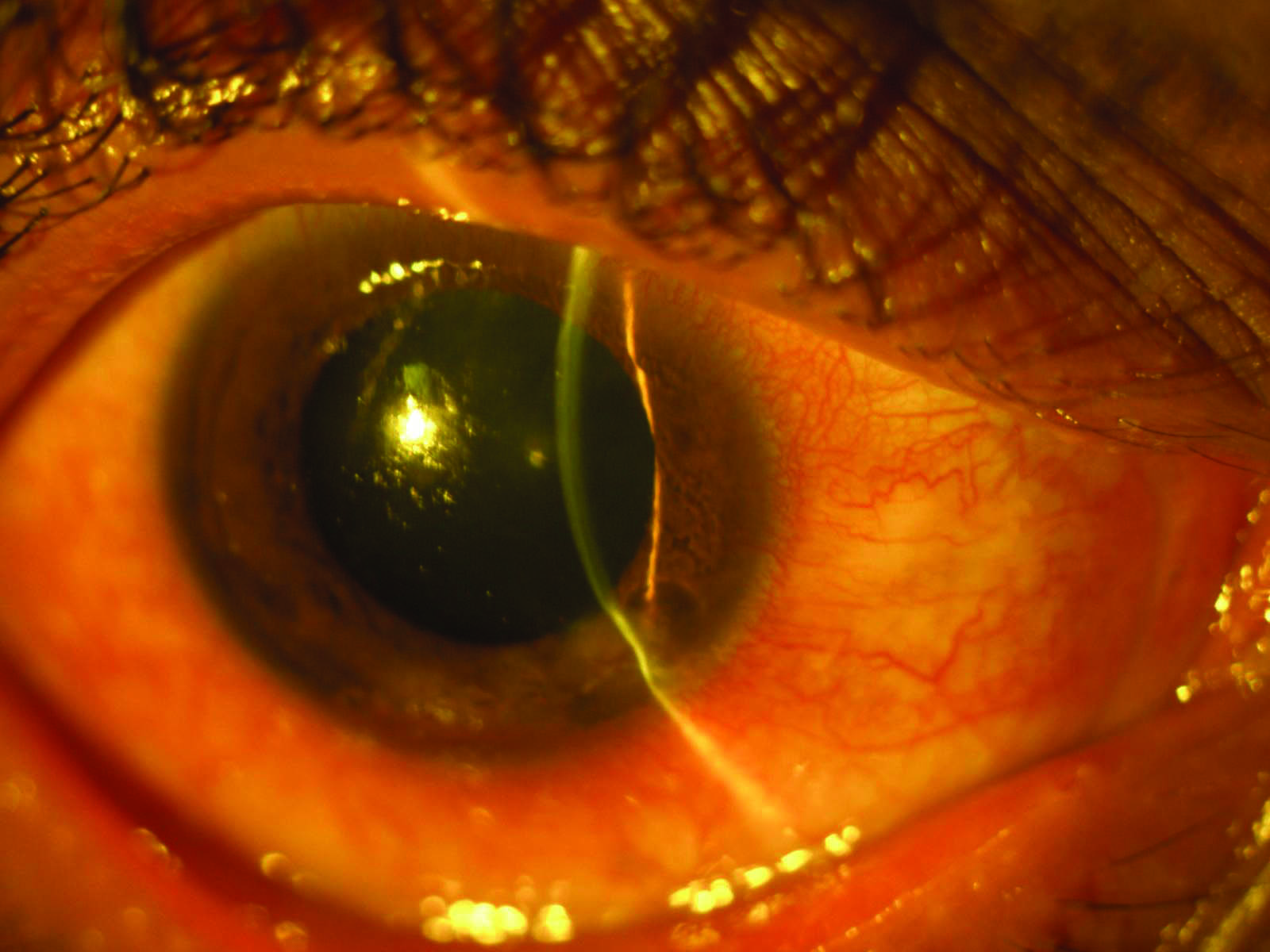
On examination, the patient has moderate built and was well-nourished. Best corrected visual acuity in right eye was 6/24 and Hand Motion Close to Face (HMCF) in left eye. Slit lamp examination revealed lusterless congested conjunctiva in both the eyes. There was a self sealed corneal perforation with sterile corneal ulcer of size 1.5x1.5 mm in right eye in inferonasal quadrant [Table/Fig-1] and a sterile corneal ulcer of size 6.5x4.0 mm in left eye with central corneal perforation with iris plugging the perforation [Table/Fig-2]. The anterior chamber was flat in left eye [Table/Fig-3]. There was no evidence of meibomian gland dysfunction or lid deformity in any of the eye.
Showing self sealed corneal perforation in inferonasal quadrant.
Showing sterile corneal ulcer with perforation in left eye.
Left eye on slit illumination showing flat anterior chamber.

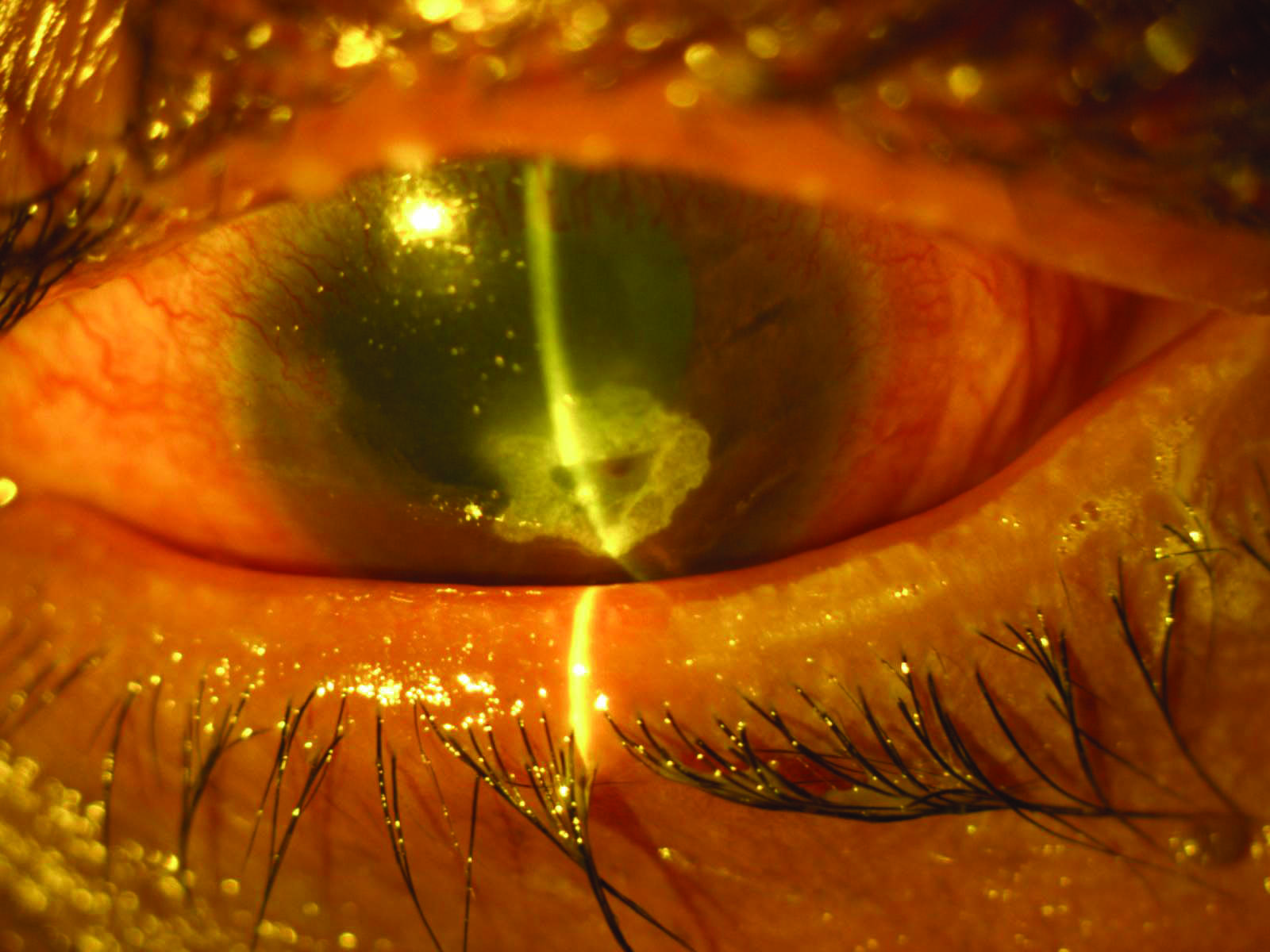
Cyanoacrylate glue was applied and bandage contact lens was placed in both eyes. He was started on topical antibiotic (gatifloxacin 0.3%) QID, topical cyclosporine 0.5% BD and preservative free artificial tears at two hourly interval. On the next day, the glue in the left eye got dislodged. The microleaks were covered using a small piece of sterile plastic sheet along with cyanoacrylate glue. Bandage contact lens was placed. Anterior chamber was of normal depth when examined next day. The patient was investigated for any systemic cause of severe dry eye. ESR was within normal limits, rheumatoid factor was negative and oral mucosal biopsy for Sjogren’s syndrome came out to be normal.
On follow up at day 7, the patient reported marked relief in photophobia. On examination, both eyes showed sealed perforation with well formed anterior chamber [Table/Fig-4,5].
Showing right eye on day 7.
Left eye at day 7 showing cyanoacrylate glue sealing the perforation and well formed Anterior Chamber (AC).
Discussion
Dry eye is an ocular surface disease which affects approximately 10%-30% of the population, especially those aged above 40 years [1]. It causes ocular discomfort, visual disturbance and tear film instability which can sometimes lead to permanent irreversible dimness of vision. Patients with Sjogren’s syndrome may suffer from sterile or infectious corneal ulceration. Occasionally, corneal perforation may occur in such cases and may cause blindness. Baranwal VK et al., reported a case of sterile corneal perforation in a 20 year old Indian male with severe dry eye disease [2]. Inagaki E et al., reported corneal perforation in four patients with dry eye related to ocular chronic graft-versus-host disease [3].
Sterile corneal ulcers can also be seen with collagen vascular diseases, autoimmune disorders, rheumatoid arthritis, ocular pemphigoid, local irradiation, in cases with trauma and in Mooren ulcers [4,5]. Sterile corneal ulcers may also develop due to conditions that affect the ocular surface epithelial integrity such as, recurrent corneal erosions, exposure keratitis, neurotrophic keratitis and keratomalacia. A case report from Ghana reported bilateral corneal perforation in Steven-Johnsons syndrome which lead to blindness in one eye of the patient [6].
Occurrence of corneal perforation after intraocular surgical procedures like cataract surgery, conductive keratoplasty and Descemet stripping endothelial keratoplasty have been reported in previously undiagnosed Sjogren’s syndrome [7-9]. To the best of our knowledge, there is no such case of severe dry eye reported, causing spontaneous corneal perforation in both the eyes.
Conclusion
One should examine a dry eye patient carefully and the patient must be investigated for sudden onset of diminution in vision, photophobia, redness and discharge in eyes so as to timely detect corneal ulcers and perforations and prevent its sequelae.
[1]. Dry Eye Workshop (DEWS) CommitteeReport of the dry eye workshop (DEWS)Ocul Surf 2007 5:65-204. [Google Scholar]
[2]. Baranwal VK, Satyabala K, Mishra A, Dutta AK, Sterile corneal perforations in a case of severe dry eyesMed J Armed Forces India 2015 71:290-92. [Google Scholar]
[3]. Inagaki E, Ogawa Y, Matsumoto Y, Kawakita T, Shimmura S, Tsubota K, Four cases of corneal perforation in patients with chronic graft-versus-host diseaseMol Vis 2011 17:598-606. [Google Scholar]
[4]. Petroutsos G, Paschides CA, Kitsos G, Skopouli FN, Psilas K, Sterile corneal ulcers in dry eye. Incidence and factors of occurrenceJ Fr Ophtalmol 1992 15:103-05. [Google Scholar]
[5]. Hemady R, Chu W, Foster CS, Keratoconjunctivitis sicca and corneal ulcersCornea 1990 9:170-73. [Google Scholar]
[6]. Noh UKM, Then KY, Spontaneous bilateral corneal perforation in stevens- johnsons syndrome–a challenge in managementMalays J Med Sci 2013 20:84-87. [Google Scholar]
[7]. Cohen KL, Sterile corneal perforation after cataract surgery in Sjogren syndromeBr J Ophthalmol 1982 66:179-82. [Google Scholar]
[8]. Shan SJC, Wu EI, Akpek EK, Sterile corneal melt after DSEK in patients with previously undiagnosed Sjogren syndromeArch Ophthalmol 2009 127:219-21. [Google Scholar]
[9]. Ou JI, Manche EE, Corneal perforation after conductive keratoplasty in patients with previously undiagnosed Sjogren syndromeArch Ophthalmol 2007 125:1131-32. [Google Scholar]