Studies have found that more than 80% of patients experience pain after surgery [1]. Moderate to severe pain in most of the cases (approximately 80%) are reported [2]. Postoperative pain due to several complications such as readmission after discharge, increasing morbidity, increased costs of hospital, delayed wound healing, increased infections etc., can led to prolonged hospital stay, one of the most common challenges for health care personnel. Therefore management of postoperative pain play a vital role in quality of health care and provide prosperity to patients [3,4].
Laminectomy is one of the most common surgeries. Annually rate is 300,000 to 400,000 [5]. The reports show $ 2.5 billion spent on back surgery in the United States [6] and lumbar pain annually causes loss of about 150 million days of work [7].
The important objectives of anaesthesia in neurosurgical patients are maintenance of haemodynamic stability and facilitating early emergence [8]. The perfect sedative should have properties like rapid onset, quick recovery and least pain, behavioural disorders and adverse effects [9]. The choice of anaesthesia in lumbar surgery, is challenging [8]. Today, the three applicable agents are: propofol, sevoflurane and desflurane [10].
Research has demonstrated that the selection of a suitable anaesthesia method can achieve a good quality of care [11]. So we compared the effects of different anaesthetics on patients who are undergoing Lumbar Disc Surgery. The aim of this study was to assess the effect of sevoflurane plus propofol on postoperative pain and complication after lumbar disc surgery.
Materials and Methods
This was a randomized double- blind clinical trial that was carried out at the Imam Khomeini hospital (center of surgery and trauma) affiliated with Ilam University of Medical Sciences, Ilam, Iran, during the year 2015-2016. The study population included all the patients for laminectomy who were referred to our department. This study was approved by the Vice chancellor for research at the Ilam University of Medical Sciences, Ilam, IR, (EC: 94/H/280) and informed consent was obtained from all samples. This study was registered at the Iranian Registry of Clinical Trials (IRCT2015071122870N2).
The inclusion criteria were – Primigravid patients, Multigravid with previous vaginal delivery, gestational age from 32 weeks or more.
Women requiring elective caesarean section, patients with high risk factors such as Pregnancy-Induced Hypertension (PIH), Gestational Diabetes Mellitus (GDM), oligohydramnios and Intrauterine growth restriction (IUGR) diagnosed during antenatal visits or at admission during labour were excluded from the study.
Sample Collections
The sample size was calculated according to data from a pilot study with 10 patients using following formula.
n= (Z1+Z2)2 (2S2) /d2 = 25
Z1 = 95%= 1.96
Z2 = 80%= 0.84 (test power)
S (an estimate of the standard deviation of VAS in the groups; 1.67 was obtained in a pilot study).
d (The minimum of the mean difference of VAS between the groups which showed a significant difference and was obtained 1.3.).
Thus, 75 patients belonging to American Society of Anaesthesiologists (ASA) grade I or II, aged 20-60 years, scheduled for elective laminectomy under general anaesthesia were enrolled in this study. Patients were randomized into 3 groups. In each group, there were 25 patients: group A (sevoflurane), group B (propofol) and group C (sevoflurane plus propofol). A simple random sampling design was used. Sampling with a sealed envelopes technique and coding was done. Coded as: code 1= sevoflurane, code 2= propofol and code 3=sevoflurane plus propofol. The patients, anaesthesiologists and surgeons were blinded to the drug administered. Coding and sealed envelopes technique for the double-blind was prepared by a nurse who was not participating in the study.
1) The patients in the Group A (sevoflurane) received anaesthesia with Thiopentone (5 mg/ kg IV for induction), Atracurium (0.5 mg/ kg IV), and maintained with sevoflurane (1-1.5%) and Nitrous Oxide (50%) in Oxygen. Group B (propofol) received anaesthesia with propofol (2 mg/ kg IV for induction), Atracurium (0.5 mg/ kg IV), and maintained with 100 mic/kg/min of propofoland Nitrous Oxide (50%) in Oxygen. Group C (sevoflurane plus propofol) received anaesthesia with propofol (2 mg/ kg IV for induction) Atracurium (0.5 mg/ kg IV), and maintained with sevoflurane (1-1.5%) and Nitrous Oxide (50%) in Oxygen multigravid with a previous caesarean section.
Neurosurgeon and anaesthesiologist were same in all patients. Fentanyl was given in the operation room according to patient need and clinical discretion. Patients were reversed with 0.05 mg/kg Neostigmine combined with 0.02mg/kg Atropine. Standard monitoring included electrocardiogram, no invasive blood pressure, and pulse oximetry was done.
Measurements
We used VAS to determine severity of pain. The pain severity was assessed at 1, 4, 8, 12 and 24 hours after surgery. The patient’s mean Blood Pressure (BP), Heart Rate (HR), Respiratory Rate (RR), Saturation (SPO2), amount of intraoperative bleeding, urine retention, vomiting, shivering, nausea, and morphine consumption were recorded. Shivering was assessed on a scale with 0= no shivering observed, 1= shivering observed.
Statistical Analysis
Collected data were analysed using the statistical software SPSS, Ver.16. (SPSS Inc, Chicago, IL, USA). Descriptive statistics, Chi-square test, one-way ANOVA, post hoc LSD and Tukey test and repeated measure ANOVA was carried out to analyse the results. The p<0.05 was considered significant.
Results
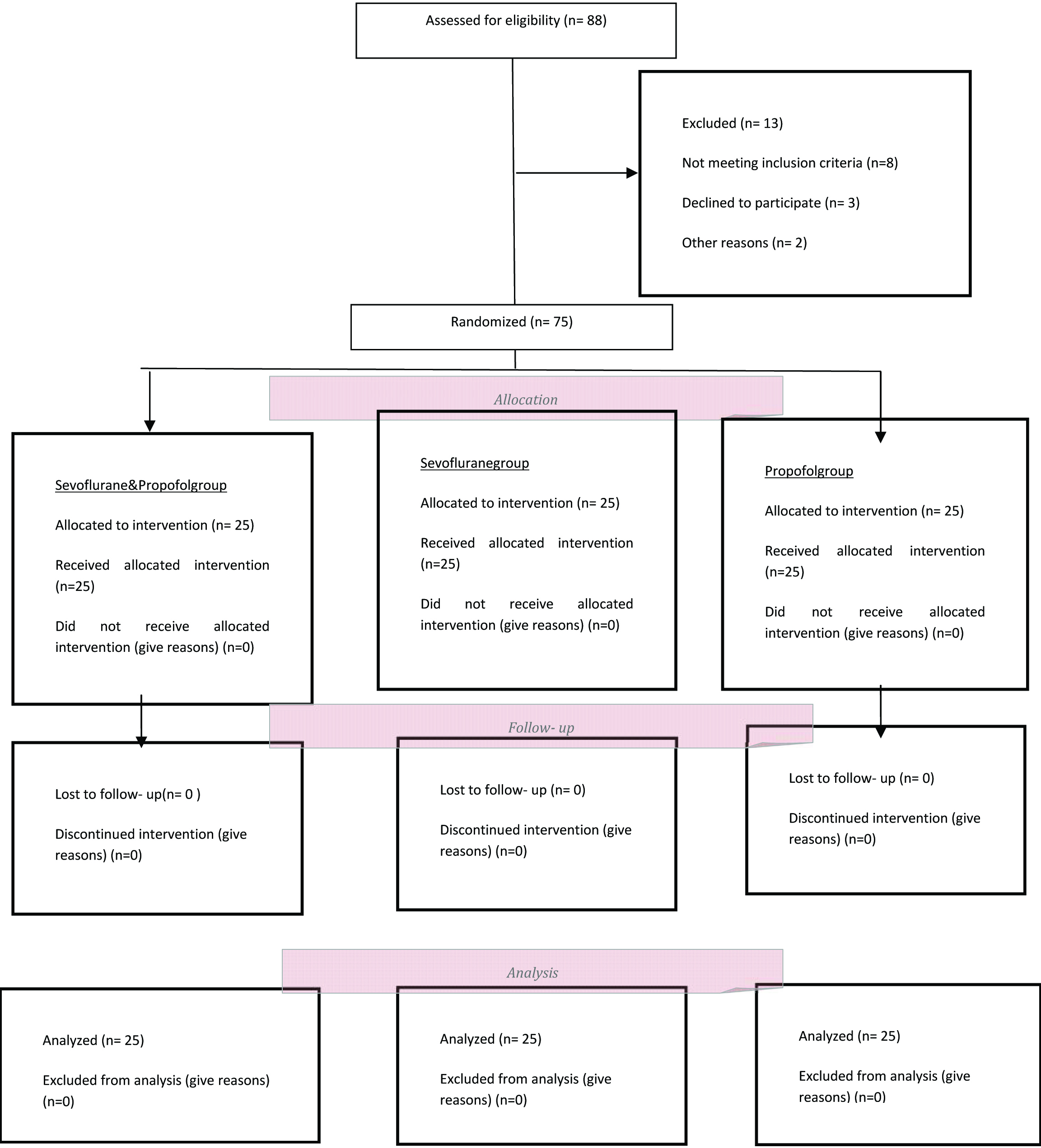
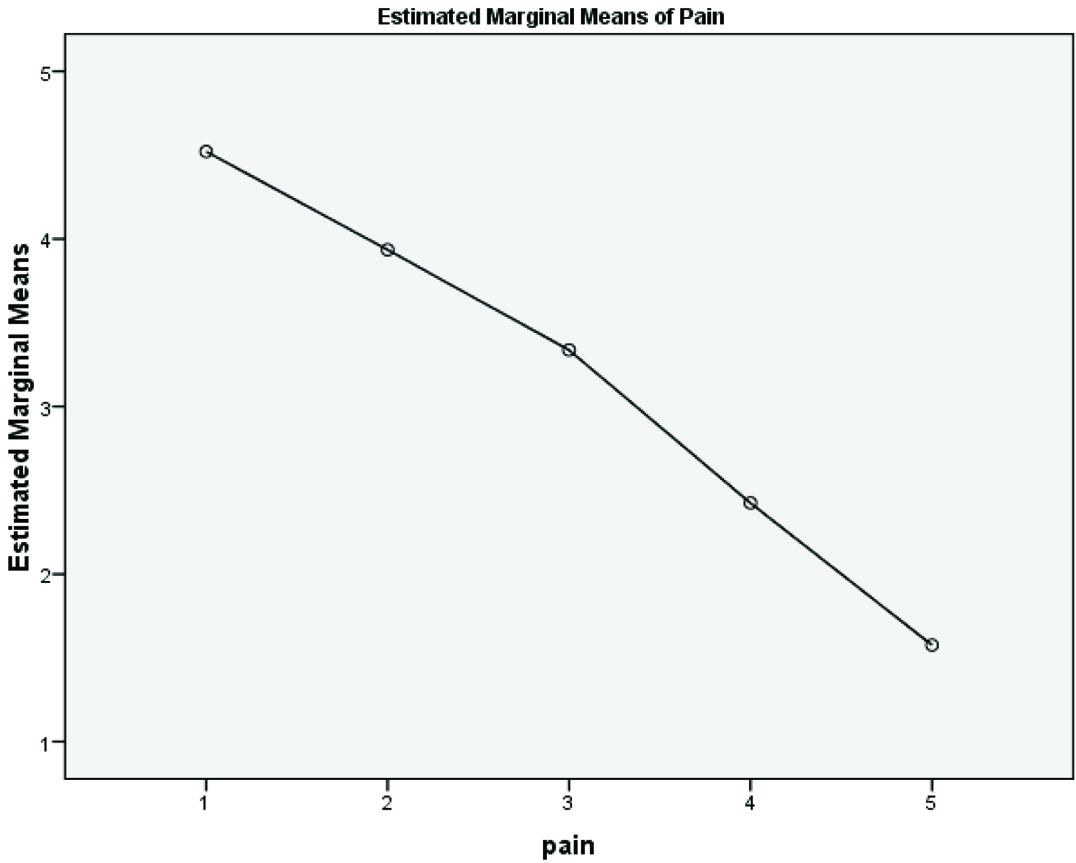
The [Table/Fig-1] shows the sequence of patients at various steps of the study. Patient’s characteristics were not different among the groups (p> 0.05) [Table/Fig-2]. According to Kolmogorov-Smirnov test, data distribution was normal and we used the parametric method (p> 0.05). One-way ANOVA showed that the mean pain severity score in the sevoflurane plus propofol group was significantly less than the propofol and sevoflurane groups at various intervals (p < 0.001) [Table/Fig-3]. The LSD and Tukey test confirmed these results (p< 0.001). Repeated measurement analysis showed that the mean pain score in the sevoflurane plus propofol, sevoflurane and propofol groups were significantly different at various intervals (p< 0.001) [Table/Fig-4].
CONSORT diagram of participant in the clinical trial.
Baseline characteristics and adverse effects of the patients1.
| Patients Characteristics | Propofol (n=25)(mean ±sd) | Sevoflurane (n=25) (mean ±sd) | Sevoflurane plus Propofol (n=25) (mean ±sd) | p-value |
|---|
| Age / year | 52.4±5.6 | 50.8±2.5 | 53.5±3.4 | 0.06** |
| Surgery Duration/min | 128±28.9 | 130±33.8 | 130±31.2 | 0.3** |
| Anaesthesia Duration /min | 151.6±23.5 | 150.4±43.4 | 152.3±27.2 | 0.4** |
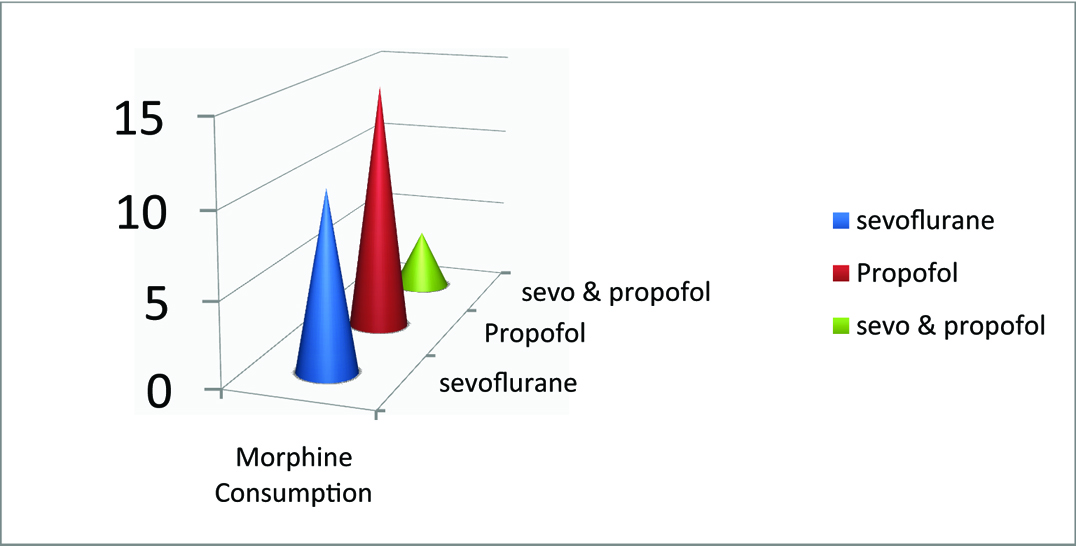
| Morphine Consumption /mg | 14.8±4.1 | 10.6±0.9 | 3.6±2.7 | <0.001* |
| Blood Pressure /S /mm | 123.6±34.5 | 112.6±20.5 | 102±18.4 | <0.001* |
| Blood Pressure /D/mm | 85.3±18.1 | 72.4±11.4 | 70.1±6.6 | <0.001* |
| Hart Rate /per-min | 77.4±2.5 | 74.3±3.3 | 70.1±2.5 | <0.001* |
| Spo2 | 95.2±0.9 | 96±0.8 | 95.3±0.4 | 0.3** |
| Recovery Time /min | 29.9±4.1 | 27.7±2.1 | 30.3±3.2 | 0.03*** |
| Blood loss | 278±35 | 243±48 | 241±47 | <0.001* |
| Nausea (n%) | 4(16%) | 15(60%) | 7 (28%) | 0.003 |
| Vomiting (n%) | 3(12%) | 12(48%) | 7 (28%) | 0.02*** |
| Shivering (n%) | 8 (32%) | 8 (32%) | 6 (24%) | 0.7** |
| Retention (n%) | 6 (24%) | 3 (12%) | 4 (16%) | 0.5** |
*p<0.001, ** p>0.05, *** p<0.05
1. Statistical test : mean, standard deviation, frequencies.
Severity of pain at various intervals in the groups2.
| Pain Score by VAS | Propofol (n=25) | Sevoflurane (n=25) | Sevoflurane plus Propofol (n=25) | p- value |
|---|
| 1 h after intervention | 6.8±1.1 | 3.3±0.4 | 2±0.2 | <0.001* |
| 4 h after intervention | 5.2±0.6 | 3±0.2 | 1.7±0.5 | <0.001* |
| 8 h after intervention | 3.6±0.5 | 2.1±0.1 | 1±0.2 | <0.001* |
| 12 h after intervention | 1.9±0.2 | 1±0.1 | 0.6±0.3 | <0.001* |
| 24 h after intervention | 1±0.4 | 0.3±0.2 | 0.1±0.1 | <0.001* |
*p<0.001
2. Statistical test: mean, Standard deviation, One-way ANOVA
Repeated measurement analysis of pain between groups.
The means of morphine consumption, blood loss, blood pressure and heart rate in the sevoflurane plus propofol group were significantly lower than the propofol and sevoflurane groups (p< 0.001) [Table/Fig-2,5]. The frequencies of nausea and vomiting in the sevoflurane group were significantly high than the other groups (p< 0.05) [Table/Fig-2]. No statistically significant difference between groups was observed in relation to shivering and retention (p > 0.05).
Morphine consumption in the groups.
Discussion
Postoperative pain can impair lung function and cause thromboembolism due to immobilization. In the process of postoperative pain due to catecholamine release cardiac workload, systemic vascular resistance and myocardial oxygen consumption can increase [12]. On the other hand, shivering can cause disruption in electrocardiogram, blood pressure and oxygen saturation monitoring [13].
Postoperative nausea and vomiting (PONV) cause increased cost of care and prolonged stay in the recovery room [14]. Opioids are the first choice to manage pain after surgery but they are associated with some complications [4].
Our finding suggested that sevoflurane plus propofol significantly reduced pain, and overall morphine consumption. Tawfik and Mostafa found that sevoflurane made the procedure painless as compared to propofol during periocular anaesthetic injections in oculoplastic procedures [9]. Choi et al., concluded that sevoflurane comparing propofol had a stable haemodynamic change, good recovery and less patient movement during the procedure in patients under interventional neuroradiology [15].
In the study by Ogurlu et al., no significant differences were found between the Sevoflurane and Propofol groups for opioid consumption or opioid-induced side-effects in patients after hysterectomy. Pain scores in the first four hours were significantly higher in the Sevoflurane group. Persistent surgical pain was less and pain scores were lower at one and three months in the propofol group [16]. Ortiz et al., concluded no statistically significant difference in pain scores, morphine and hydrocodone use in propofol, isoflurane, desflurane, or sevoflurane groups after laparoscopic cholecystectomy [17].
Park et al., concluded no significant differences in relation to anti-emetics, analgesics and the VAS scores between the sevoflurane combined with ramosetron and propofol groups in women undergoing total thyroidectomy [18]. Sirvinskas et al., in their study of comparison between sevoflurane and propofol on the activity of mitochondrial function related to ischemia-reperfusion injury in patients after Coronary Artery Bypass Graft Surgery (CABG) concluded that there were no significant differences in the duration of mechanical ventilation, haemodynamic parameters and length of stay in the ICU between the groups [19]. Guçlu et al., showed that Oxygen saturation was higher in the sevoflurane group than in the total intravenous anaesthesia group in the cardiopulmonary bypass [20].
Propofol, Sevoflurane, Isoflurane and Desflurane are commonly used to maintain anaesthesia in patients undergoing general anaesthesia [15]. Studies have shown that Sevoflurane is associated with faster recovery, whereas Isoflurane and Propofol have a similar recovery in general anaesthesia [21,22]. Propofol is effective in lowering the risk of PONV due to its antiemetic effect [15]. Sevoflurane, an inhalation anaesthetic with rapid induction, is non pungent and non irritating to the respiratory tract. Alternatively, propofol has a rapid onset time and short duration as short acting, intravenous anaesthetics [23].
It is well known that propofol has an antiemetic effect. Therefore, propofol-based Total Intravenous Anaesthesia (TIVA) has been reported to be effective to lower the risk of PONV [15].
Limitation
The limitations of our study include relatively small sample size and the subjective perception of pain by patients. All patients enrolled in this study underwent surgery by a single surgeon; and the data were collected from a single center that was the strengths of this study.
Conclusion
The current study finding revealed that sevoflurane plus propofol significantly reduced postoperative pain after lumbar disc surgery. It was observed that sevoflurane plus propofol had less adverse effects, decreased the amount of morphine consumption and increased patient satisfaction. But nausea and vomiting were significantly high in sevoflurane group following lumbar disc surgery.
Funding/Support
This study was supported by Ilam University of Medical Sciences (EC: 94/H/280).
*p<0.001, ** p>0.05, *** p<0.05
1. Statistical test : mean, standard deviation, frequencies.
*p<0.001
2. Statistical test: mean, Standard deviation, One-way ANOVA