Carcinoma Cervix Presenting as Ischaemic Stroke in Young Female: A Case Report and Review of Literature
Suruchi Gupta1, Nikhil Gupta2, Shilpa Singhal3, Nikhil Nair4
1 Senior Resident, Department of Gynaecology, Safdarjung Hospital, Delhi, India.
2 Fellow, Department of Clinical Immunology and Rheumatology, CMC, Vellore, Tamil Nadu, India.
3 Senior Resident, Department of Pathology, BJ Medical College, Ahemdabad, Gujarat, India.
4 Senior Resident, Department of Radio-Diagnosis, AIIMS, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nikhil Gupta, Fellow, Department of Clinical Immunology and Rheumatology, CMC, Vellore-632004, Tamil Nadu, India.
E-mail: drnikhilguptamamc@gmail.com
Stroke is a disabling disease which increases the burden of already suffering cancer patients. Several mechanisms of stroke exist in cancer patients which includes - metastatic or non-metastatic such as coagulation disorders, infections or therapy related. Increased risk of ischaemic stroke has been validated for several cancers. However, there is scarce literature reported in carcinoma cervix patients. Review of literature suggests that stroke occurs more frequently in cancer patients than in the average population. We report an unusual case of a patient who presented with stroke but was later diagnosed as a case of carcinoma cervix.
Cerebrovascular accident, Hemiparesis, Metastasis, Radiotherapy
Case Report
A 30-year-old married woman presented to the emergency ward with complaints of sudden hemiparesis of left side of body eight hours after its onset. The patient’s past medical history was unremarkable. She was taking no medications (including oral contraceptive pills and ergotamine). She was a non-smoker. There was no history of seizures, slurring of speech, or decline in her cognitive functions. There was no history of diabetes or hypertension, or repeated abortions.
On physical examination, the patient’s blood pressure level was 132/78 mm Hg in the right arm and her pulse rate was 88/min. All the peripheral pulses were palpable. She was afebrile, conscious and oriented. There was no neck rigidity or calf tenderness. Systemic examination including cardiovascular, pulmonary, abdominal, skin and musculoskeletal examination findings were unremarkable. There were no carotid bruits. On neurologic examination, there was paralysis of left upper and lower limb with power of 0/5 at all joints. Higher mental functions including memory were normal. Fundus examination was normal. On investigations, haemogram, erythrocyte sedimentation rate, blood sugar, kidney function tests, liver function tests, cholesterol, serum electrolytes, urine analysis, chest X-ray, ECG and ECHO were normal. Her Computed Tomography (CT) thorax, abdomen and pelvis were unremarkable.
Coagulation profile including prothrombin time, activated partial thromboplastin time, antinuclear antibody test, anticardiolipin antibody IgM, serum homocysteine, protein C level and antithrombin III level were within normal limits.
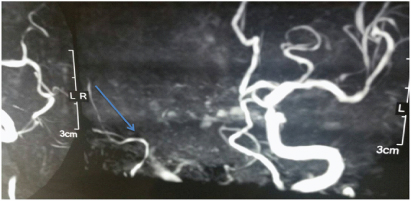
Magnetic Resonance Imaging (MRI) scan of the brain revealed T2 weighted hyperintense lesions in left capsulo ganglionic and parieto-occipital regions. 3D MR arteriogram image showed non visualisation of right internal carotid artery and its major branches [Table/Fig-1]. Diffusion weighted image showed diffusely bright appearance of right cerebral hemisphere suggestive of diffusion restriction indicating acute infarct.
A–3D MR arteriogram image showing non visualisation of right internal carotid artery and its major branches (arrow).
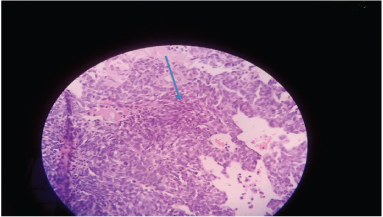
While taking history, she fortunately told about the two to three episodes of post-coital bleeding per vaginal since one month for which gynaecological reference was taken. Her menstrual history was normal. Pelvic examination revealed an ulcero-proliferative cervical growth. Biopsy of the lesion showed a poorly differentiated squamous cell carcinoma [Table/Fig-2].
Biopsy of the lesion showing a poorly differentiated squamous cell carcinoma (arrow).
After a thorough clinico-radiological workup disease was staged as FIGO Stage IIa. Metastatic workup which included computed tomographic scan of the thorax, abdomen and pelvis, did not reveal any metastasis. Patient was started on tablet ecospirin and statin. Gynaecologically, patient was planned for chemoradiation.
Discussion
Carcinoma cervix is a common cancer occurring in women. It is most often diagnosed in middle aged women. Clinically, the patient can present with various complaints. In early stage, invasive carcinoma of the cervix causes no symptoms and is only discovered accidentally. Symptoms come with surface ulceration and consist only of irregular uterine bleeding or discharge or both, these being around peri or postmenopausal. The initial episode of bleeding usually follows coitus, straining at stool or any condition which exposes the cervix to trauma. Subsequent losses can be alarmingly heavy. Other symptoms usually occur at advanced stage of cancer. They include frequency of micturition, dysuria, urinary incontinence, rectal pain, deep pelvic ache, low backache, sciatica, ureteric colic, oedema of the legs, loss of weight, anorexia and malaise. Liver metastases may present as right upper quadrant pain and fullness; lung metastases as haemoptysis and a persistent cough [1]. Neurological deficit in carcinoma cervix is a rare phenomenon and is often considered to be a sign of cerebral metastasis. Tsai SJ et al., has reported increased risk of stroke in carcinoma cervix patients [2]. However, imaging, “such as CT and MRI, or even brain biopsy” is needed for correct diagnosis and subsequent management [3-4].
Neurological complications in cervical cancer can be due to either metastatic or non-metastatic causes, former being more common. [4,5]. Cerebrovascular disease is an important cause of central nervous system pathology in the cancer patient [6]. In such cases, metastatic cause should be first ruled out by clinical signs and radiological imaging. Thereafter, risk factors of cerebral ischemic events, tumour related effects, coagulation disorders, infection, therapy-related effects and paraneoplastic causes should be looked for [7].
Our patient was a young 30-year old without any classical risk factor of stroke. Her coagulation profile was normal. She was a Stage IIa carcinoma cervix. There was no evidence of metastasis and MRI also showed ischaemic infarcts.
Conclusion
Carcinoma cervix patients may have a higher risk of neurological complications like non metastatic stroke and venous thromboembolic events, especially in younger patients. Hence, physicians should anticipate this also, in dealing with patients presenting with symptoms of central nervous system pathology as to provide prompt and comprehensive treatment. Future studies may be planned to find out any association between stroke and carcinoma cervix.
[1]. Kumar P, Malhotra N, Jeffcoate’s principles of gynaecology 2008 seventh editionJaypee brothers:471-72. [Google Scholar]
[2]. Tsai SJ, Huang YS, Tung CH, Lee CC, Lee MS, Chiou WY, et al, Increased risk of ischemic stroke in cervical cancer patients: a nationwide population-based studyRadiat Oncol 2013 8:41 [Google Scholar]
[3]. Grisold W, Oberndorfer S, Struhal W, Stroke and cancer: a reviewActa Neurol Scand 2009 119:1-16. [Google Scholar]
[4]. Kuan AS, Teng CJ, Wu HH, Su VYF, Chen YT, Chien SH, et al, Risk of ischemic stroke in patients with ovarian cancer: a nationwide population-based studyBMC Medicine 2014 12:53 [Google Scholar]
[5]. Dearborn JL, Urrutia VC, Zeiler SR, Stroke and cancer- a complicated relationshipJ Neurol Transl Neurosci 2014 2(1):1039 [Google Scholar]
[6]. Rogers LR, Cerebrovascular complications in cancer patientsNeurol Clin 1991 9:889-99. [Google Scholar]
[7]. Graus F, Delattre JY, Antoine JC, Dalmau J, Giometto B, Grisold W, et al, Recommended diagnostic criteria for paraneoplastic neurological syndromesJ Neurol Neurosurg Psychiatry 2004 75:1135-40. [Google Scholar]