Staged Hard and Soft Tissue Reconstruction Followed by Implant Supported Restoration in the Aesthetic Zone: A Case Report
Harinath Parthasarathy1, Lakshmi Ramachandran2, Anupama Tadepalli3, Deepa Ponnaiyan4
1 Professor, Department of Periodontology, Srm Dental College, Chennai, Tamil Nadu, India.
2 Post Graduate Student, Department of Periodontics, Srm Dental College, Chennai, Tamil Nadu, India.
3 Reader, Department of Periodontics, Srm Dental College, Chennai, Tamil Nadu, India.
4 Reader, Department of Periodontics, Srm Dental College, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Harinath Parthasarathy, Professor, Department of Periodontics, Srm Dental College, Bharathi Salai, Rama Puram, Chennai-600089, Tamil Nadu, India.
E-mail: hari_feb14@hotmail.com
Alveolar ridge deficiency is a common clinical consequence following tooth loss due to chronic periodontitis complicating ideal implant placement. Advanced hard and soft tissue augmentation procedures have been developed in the recent past with predictable clinical outcomes. A male patient presented with a Grade III mobile upper right central incisor associated with advanced bone loss and soft tissue deficit. Following extraction of tooth #11, socket augmentation was done using an autogenous cortico-cancellous block graft and subsequent soft tissue augmentation was done with palatal connective tissue graft. At the end of six months, a tapered self tapping implant fixture was placed with adequate primary stability and after eight weeks, second stage implant surgery was done with the Misch technique in order to recreate papillae and the implant was prosthetically restored. The alveolar ridge was adequately recontoured following the staged surgical protocol. The implant was well integrated at the end of 15 months. Execution of sequential surgical procedures in a highly deficient edentulous site made it possible to achieve of optimal pink and white aesthetics with stable implant supported fixed prosthesis.
Cortico-cancellous block graft, Guided bone regeneration, Connective tissue graft, Split finger technique
Case Report
A 45-year-old systemically healthy male patient reported to outpatient clinic, Department of Periodontics and Oral Implantology, SRM Dental College, Chennai, India, complaining of mobility in his upper front tooth for the past six months which was not associated with any history of trauma. Clinical observations included, mild extrusion, Grade III mobility, Miller’s Class IV recession in relation to right central incisor #11 and radiographic examination revealed advanced bone loss till apical third of the root [Table/Fig-1,2]. Though right lateral incisor #12 revealed recession clinically and bone loss radiographically, it didn’t exhibit any degree of mobility or active pocket. A diagnosis of localized chronic periodontitis was made in relation to teeth #11, 12. Since, the patient had a strong desire towards fixed replacement of his front teeth; atraumatic extraction was planned in relation to tooth #11 followed by socket augmentation for delayed implant placement, a duly signed consent according to Declaration of Helsinki was obtained.
Surgical Management
Guided Bone Regeneration
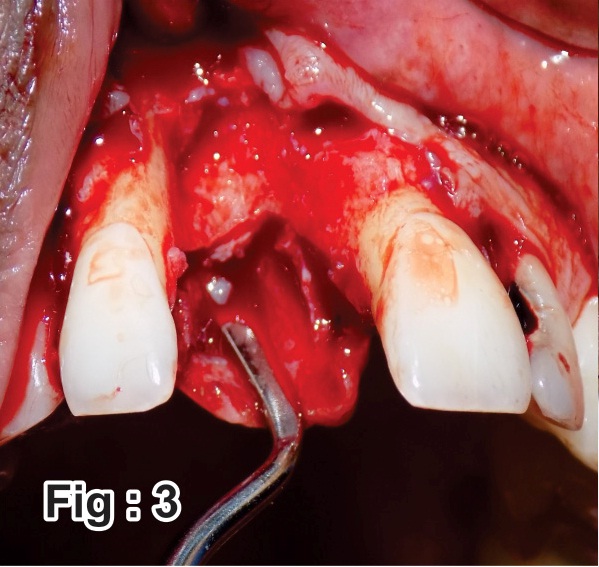
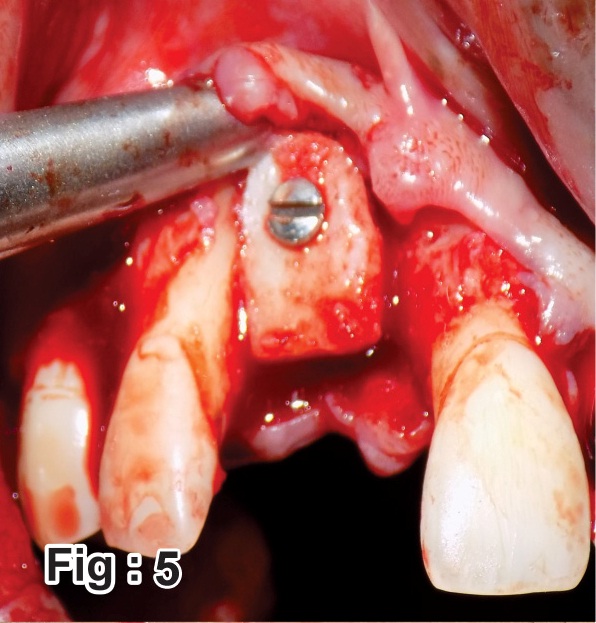
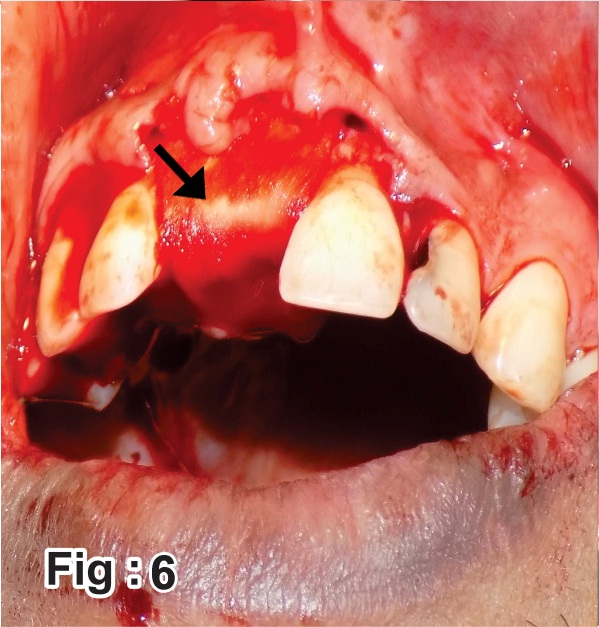
Following extraction, a horizontal mid crestal and two vertical releasing incisions on the buccal surface were given to raise a full thickness flap. A knife edge type of defect was observed (6, 4 mm in vertical and horizontal dimensions respectively). Prior to augmentation the recipient bed was prepared to receive a cortico-cancellous block graft [Table/Fig-3]. A cortico-cancellous block graft was atraumatically harvested from the buccal cortical plate of edentulous site in relation to teeth #46, 47, under copious saline irrigation [Table/Fig-4]. The donor site was chosen as the patient was not willing for implant supported restorations in relation to teeth #46, 47 owing to cost for multiple implant procedures and hence a fixed tooth supported prosthesis was planned for missing posteriors. The procured graft was shaped to fit the recipient bed and stabilised with the help of SS screws 1.5 mm [Table/Fig-5]. A xenogenic collagen membrane (HealiguideTM, Advanced Biotech Products Ltd. TamilNadu, India) was adapted over the graft, extending 2 mm laterally in the recipient site [Table/Fig-6].
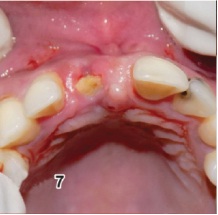
Both the surgical sites were approximated with 5-0 resorbable vicryl sutures (ETHICON Johnson & Johnson), non-eugenol pack was placed. Postoperative instructions regarding wound care and medication (analgesics and antibiotics) were given. Patient was reviewed at one and two weeks, healing was satisfactory in both the operated sites. During the second month recall, a small exposure of block graft was observed crestally (<3 mm), for which surgical intervention with soft tissue augmentation was planned [Table/Fig-7].
Soft Tissue Augmentation
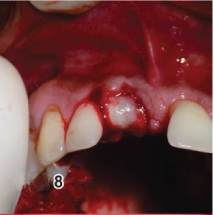
A minimal crestal incision was given, intraoperative examination revealed an intact graft, hence only the exposed portion of the graft was contoured using slow speed rotary instruments with copious saline irrigation and flap was undermined buccally to create a space. Connective Tissue Graft (CTG), harvested from palate was interposed into the space in a bucco-palatal direction and flap was approximated with a cross mattress sutures, non- eugenol pack was placed and postoperative medications were given [Table/Fig-8,9].
Implant Placement
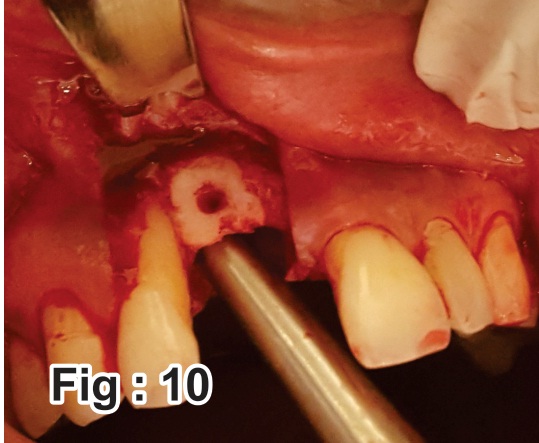
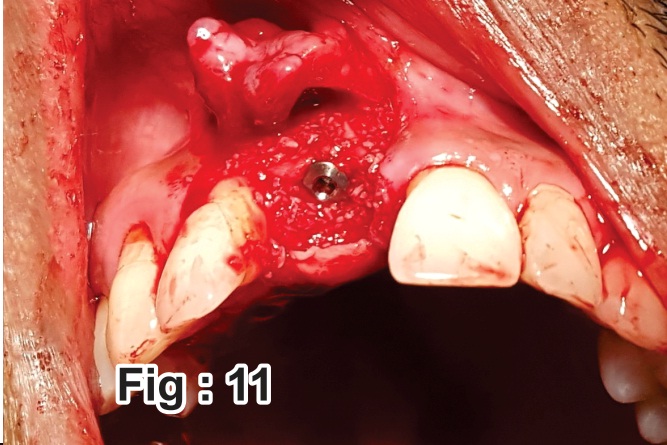
Following Guided Bone Regeneration (GBR) at the end of six months, the site was re-entered, coronally the demarcation line delineating the graft was clinically visible; however the graft was well integrated to the native bone apically with no mobility [Table/Fig-10]. Implant osteotomy was performed in a palatal direction in order to engage the palatal bone simultaneously maintaining the parallelism with the adjacent teeth and to obtain a good emergence profile. A tapered self tapping implant, (3.5 x 11.5 ADIN SYSTEM, Afula, Israel) was placed with an adequate primary stability of 35 Ncm. Particulate grafting (xenogenic graft OsseograftTM Advanced Biotech Products Ltd. Tamil Nadu, India) was done to augment the osteotomy site buccally and interproximally and implant was submerged for delayed loading [Table/Fig-11]. The addition of particulate graft interproximally along with coronal advancement of the flap had partially compensated the attachment loss on mesial aspect of tooth #12.
Peri-implant Papillae Creation (Misch technique) [
1]
Eight weeks following implant placement [Table/Fig-12], implant exposure was performed using the Misch technique to recreate papillae. The split finger technique comprised of a sulcular incision 2-3 mm palatal to the crest. Followed by elevation of full thickness buccal flap, healing abutment was placed, and the buccal flap was split in the midline to create fingers which were secured to respective mesial and distal de-epithelialized palatal papillae using 6-0 resorbable sutures [Table/Fig-13a,b].
Prosthetic Rehabilitation
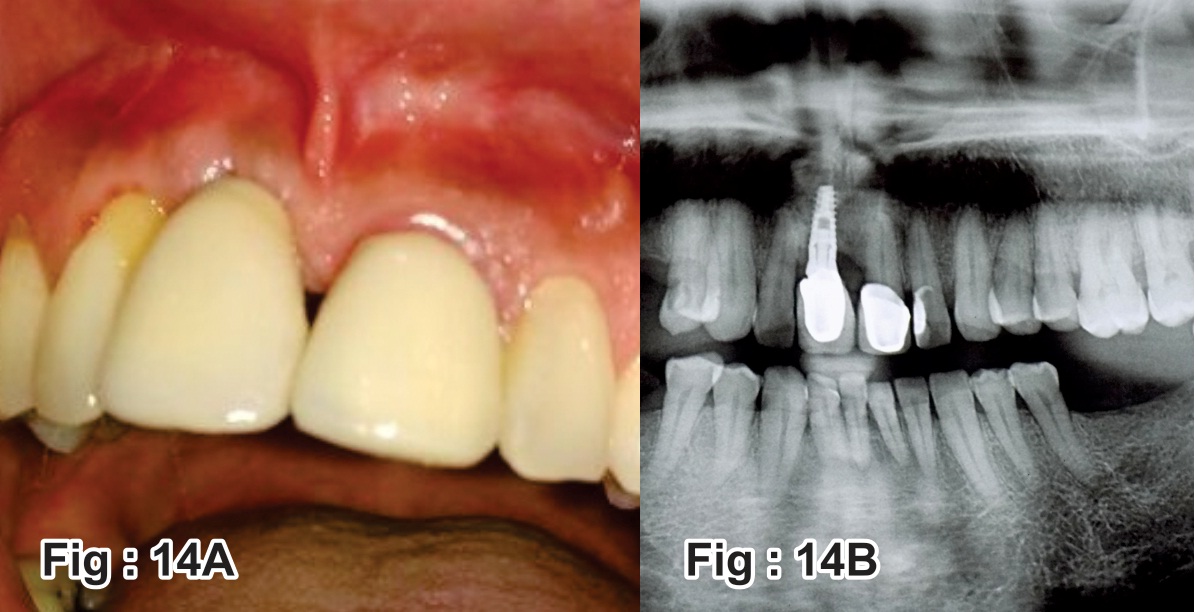
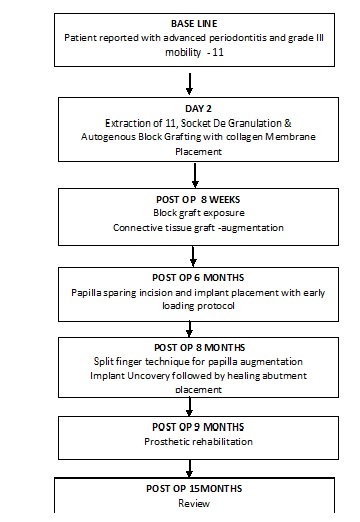
At the end of four weeks, prosthetic rehabilitation was carried out. In order to restore white aesthetics, 21 were prepared minimally to receive a ceramic crown to close the diastema and a permanent metal ceramic restoration was cemented to the implant in relation to tooth #11. At the end of six months, implant was clinically stable and radiographically revealed adequate bone to implant contact and the patient was highly satisfied with the aesthetic and functional outcome [Table/Fig-14a,b,15]. The summary of the treatment procedure is shown in figure [Table/Fig-16].
Shows preoperative clinical and radiographic views.

Shows recipient site preparation in relation to tooth #11.
Shows donor site after harvesting cortico- cancellous block graft in relation to teeth #46, 47.

Shows cortico-cancellous block graft stabilization in the recipient site.
Shows xenogenoic collagen membrane adaptation.
Shows graft exposure at the end of eight weeks.
Shows soft tissue augmentation for covering the graft exposure and augmenting keratinised mucosa with connective tissue graft.
Shows connective tissue graft stabilisation using cross-mattress sutures.

Shows papilla sparing incision and integrated cortico-cancellous graft after six months.
Shows endosseous titanium implant with dimensions 3.5 x 11.5 mm placed achieving adequate primary stability.
Shows adequate attached mucosa eight weeks following implant placement.

Shows papilla recreation incision following Misch split finger technique and suturing to adjacent papillae.

Shows clinical and radiographic views at the end of 15 months.
Shows final aesthetic outcome.

Shows the summary of the entire treatment procedure.
Discussion
With the advent of surgical advances in socket/ridge augmentation, teeth with poor periodontal prognosis are no longer a compromise to aesthetics and function of dentition [2]. The therapeutic approaches considered for implant site development is decided based on the location and topography of defect [3].
Successful treatment of localised ridge defects can be achieved with autogenous intraoral bone grafts as it is highly predictable with very less chances of rejection [4]. Further cortico-cancellous block grafts have proved their efficacy in vertical and lateral ridge augmentation [5,6], the benefits of choosing the edentulous site as donor avoids patient associated morbidity which occurs with conventional ramus and symphyseal grafting [7]. Adding to the afore said facts the embryonic origin of intraoral grafts being the same i.e., intramembranous, offers less resorption, early revascularisation and better potential for incorporation into the recipient site, credited to the similarity in the protocollagen and increased amounts of bone morphogenic protein [8]. The shortcomings of cortico-cancellous blockgrafts are graft exposure which was noticed in current case and resorption [9,10].
Moreover, the associated lack of keratinised tissue, necessitated soft tissue augmentation, hence an autogenous CTG was used to augment the mucosa during management of graft exposure [11]. The CTG has a better chance of survival than free grafts over a less vascularised area [12]. Factors which play a pivotal role in successful soft tissue augmentation include stability of the graft and early revascularisation.
The ideal goal following implant placement in the anterior zone is to recreate the soft tissue drape and maintain the interdental papillae as stated by Kois [13]. The morphological and histological characteristics of peri impant tissue pose a major limitation for papillae reconstruction [14]. Misch’s split finger technique appears to provide very high success rates especially in single tooth replacements as observed in this case report by creation of an optimal emergence profile with ideal inter implant tissue [1]. The prosthetic rehabilitation included additional porcelain fused metal crown in relation to adjacent central incisor in order to manage the midline diastema.
Conclusion
This article proposes a sequential and staged surgical management of a deficient edentulous site in the anterior maxilla, in spite of the long duration of treatment the clinical outcomes, restoration of the pink and white aesthetics was achieved and patient related outcome were highly satisfactory.
[1]. CE Misch, The split finger technique for creation of interimplant papilla: A pilot studyContinium 2001 :1-3. [Google Scholar]
[2]. U Kuchler, T von Arx, Horizontal ridge augmentation in conjunction with or prior to implant placement in the anterior maxilla: a systematic reviewInternational Journal of Oral & Maxillofacial Implants 2014 29:14-24. [Google Scholar]
[3]. H Chansoria, S Chansoria, D Jain, Localised ridge augmentation with autogenous block bonegraft for the restoration of maxillary anterior teethIOSR Journal of Dental and Medical Sciences (IOSR-JDMS) 2014 1(13):73-76. [Google Scholar]
[4]. T Von Arx, D Buser, Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: a clinical study with 42 patientsClinical Oral Implants Research 2006 17(4):359-66. [Google Scholar]
[5]. RE Marx, Biology of bone graftsOMS Knowledge Update 1994 :1 [Google Scholar]
[6]. KP Rao, S Pagadala, Localized ridge augmentation using autogenous block [6]bone graft followed by dental implant placementJournal of Orofacial Sciences 2012 4(2):148 [Google Scholar]
[7]. JA Leonetti, R Koup, Localized maxillary ridge augmentation with a block allograft for dental implant placement: case reportsImplant Dentistry 2003 12(3):217-26. [Google Scholar]
[8]. H Kumar, M Verma, AK Lamba, F Faraz, Rahul Kriti Restoration of maxillary anterior defect using autogenous block graft and optimizing the aesthetics using zirconia restorationIntl J Oral Implantology & Clinical Res 2011 2(3):165-170. [Google Scholar]
[9]. JP Fiorellini, ML Nevins, Localized ridge augmentation/preservation: A systematic reviewAnnals of Periodontology 2003 8(1):321-27. [Google Scholar]
[10]. P Proussaefs, J Lozada, The use of intraorally harvested autogenous block grafts for vertical alveolar ridge augmentation: a human studyInt J Periodontics Restorative Dent 2005 25(4):351-63. [Google Scholar]
[11]. F Khoury, A Happe, The palatal subepithelial connective tissue flap method for soft tissue management to cover maxillary defects: a clinical reportInt J Oral Maxillofac Implants 2000 15(3):415-18. [Google Scholar]
[12]. KS Al-Hamdan, Aesthetic soft tissue ridge augmentation around dental implant: Case reportThe Saudi Dental Journal 2007 23:205-09. [Google Scholar]
[13]. JC Kois, JY Kan, Predictable periimplant gingival aesthetics: surgical and prosthodontic rationalesPract Proced Aesthet Dent 2000 13:691-98. [Google Scholar]
[14]. S Dhir, The peri-implant esthetics: An unforgettable entityJournal of Indian Society of Periodontology 2011 15(2):98 [Google Scholar]