Oncogenic Osteomalacia: An Approach to Diagnosis with a Case Report
Biswajit Dey1, Debasis Gochhait2, Hema Subramanian3, Madhusudhanan Ponnusamy4
1 Senior Resident, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India.
2 Assistant Professor, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India.
3 Junior Resident, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India.
4 Assistant Professor, Department of Nuclear Medicine, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Debasis Gochhait, Assistant Professor, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry-605006, India.
E-mail: publicationmail@rediffmail.com
Oncogenic osteomalacia, also known as tumour induced osteomalacia, is a rare paraneoplastic syndrome caused by mesenchymal tumours secreting Fibroblast Growth Factor-23 (FGF-23). The characteristic biochemical findings include hypophosphatemia and low 1,25-dihydroxy vitamin D. The differential diagnosis for hypophosphatemia are varied. We present a case of oncogenic osteomalacia in a 29-year-old female, who presented with complaints of generalized diffuse bone pain and walking difficulty for six months duration. Thus, we have discussed the approach to diagnosis in such a case.
Fibroblast growth factor-23, Phosphaturic mesenchymal tumour, Scintigraphy
Case Report
We present the case of a 29-year-old female arriving with an antalgic gait, who presented with complaints of generalized diffuse bone pain and walking difficulty for six months duration. She had no prior history of fall or trauma and her dietary milk intake was adequate. Her childhood was uneventful with normal developmental milestones. She was taking over-the-counter painkillers for the same.
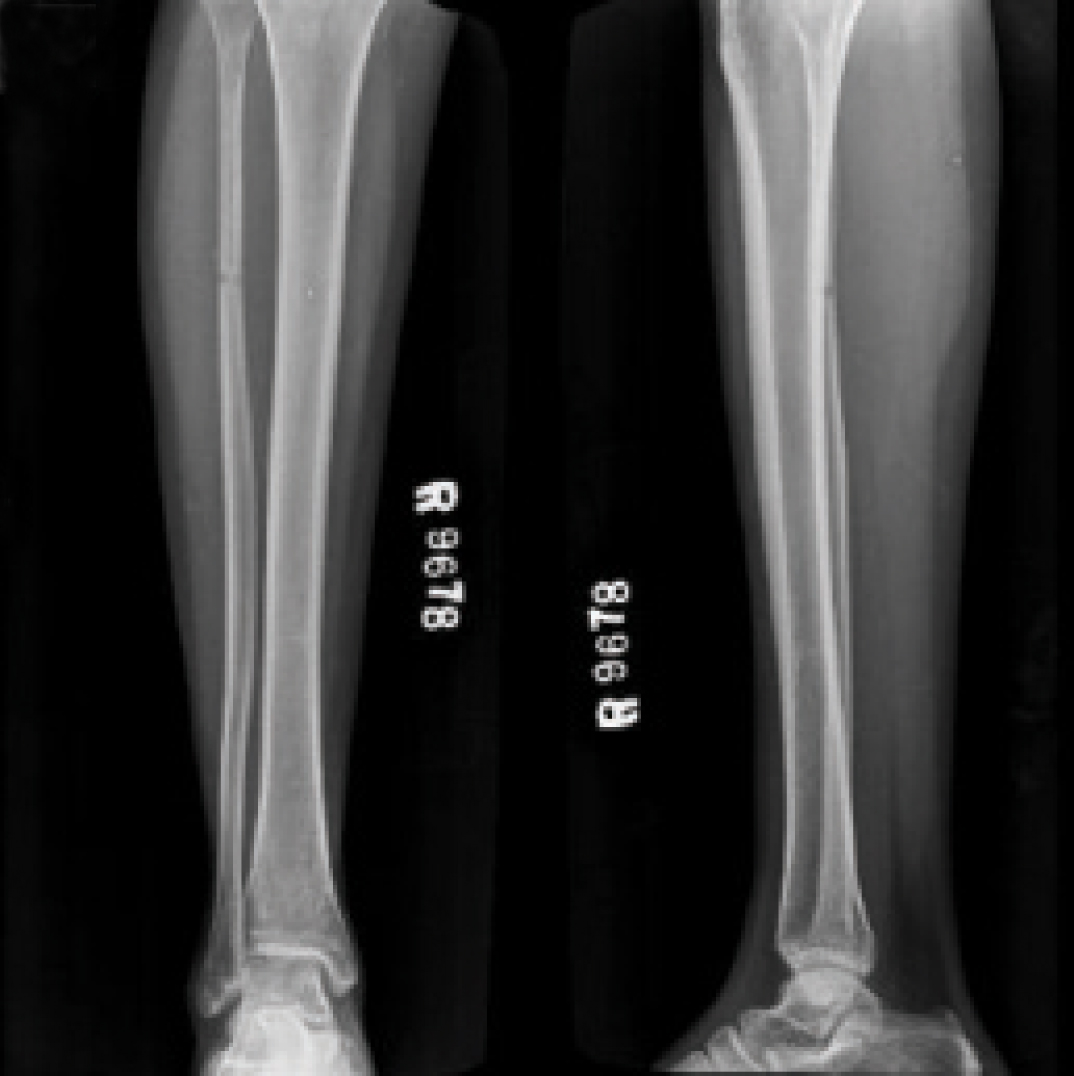
Biochemical paramaters showed serum calcium of 8.1 mg/dl (Normal Range (NR), 9–11), phosphate of 1.3 mg/dl (NR, 2.5– 4.5), albumin of 4.5 g/dl (NR, 3.5–5.5), alkaline phosphatase of 528 IU/l (NR, 40–150), creatinine of 0.9 mg/dl (NR, 0.7–1.2), intact parathormone of 52.9 pg/ml (NR, 9–52) and 25-hydroxyvitamin D 22.91 ng/ml (NR, 30–100 ng/ml). Baseline investigations revealed hypophosphatemia along with mild hypocalcaemia and high normal parathormone levels. These findings, in addition to the Looser’s zone seen on right fibular xeroradiography [Table/Fig-1] pointed to the diagnosis of hypophosphatemic/phosphopenic osteomalacia. Her Tubular Reabsorption of Phosphate (TRP) was 73.4% (NR, 85-95%) and ratio of maximum rate of renal tubular reabsorption of phosphate to glomerular filtration rate (TmPO4/GFR) was 1.0 (NR, 2.7– 4.4). Thus renal wasting of phosphate was confirmed by low TRP and TmPO4/GFR. Absent urinary sugars and protein ruled out the possibility of renal Fanconi syndrome being the cause of phosphaturia. Her serum C-terminal FGF-23 level was 257 RU/ml (NR, 0–150). An elevated serum FGF-23 level confirmed its role in renal phosphate wasting in this case. Absence of similar complaints among her family members negated the possibility of the heritable forms of phosphopenic osteomalacia, namely Autosomal Recessive Hypophosphatemic Rickets (ARHPR), Autosomal Dominant Hypophosphatemic Rickets (ADHPR) and X-Linked Dominant Hypophosphatemic Rickets (XLHPR). Hence, the suspicion of a tumour producing FGF-23 arose, warranting extensive anatomical and functional radioimaging of the body in order to localise the offending lesion.
Looser’s zone seen on right fibular xeroradiography.
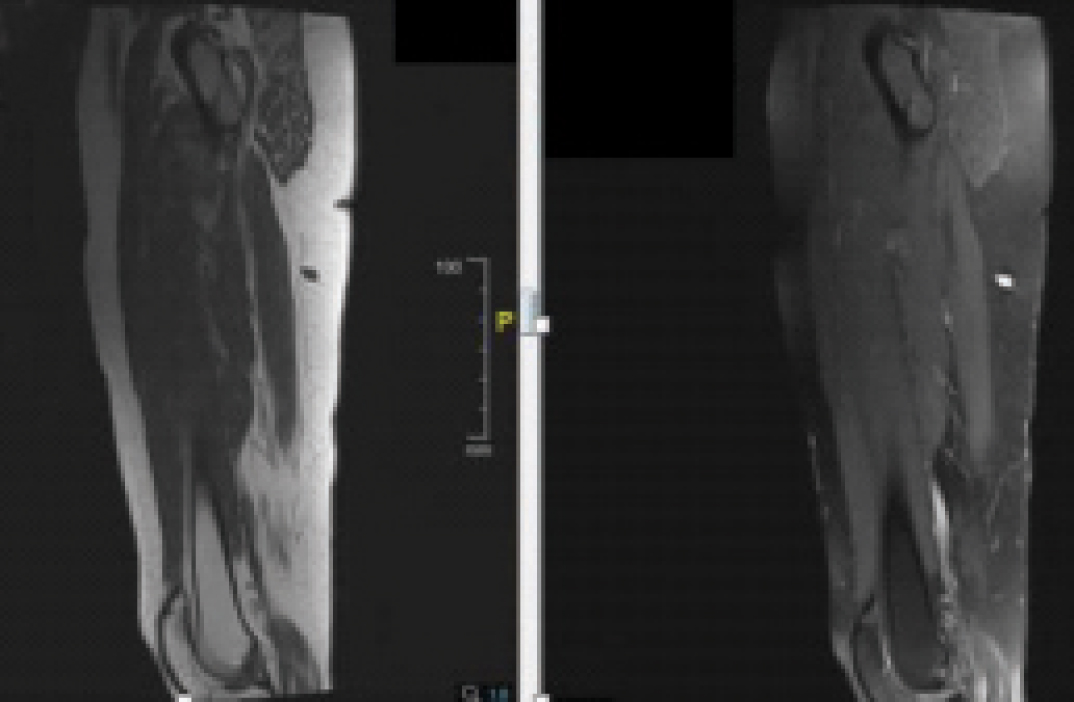
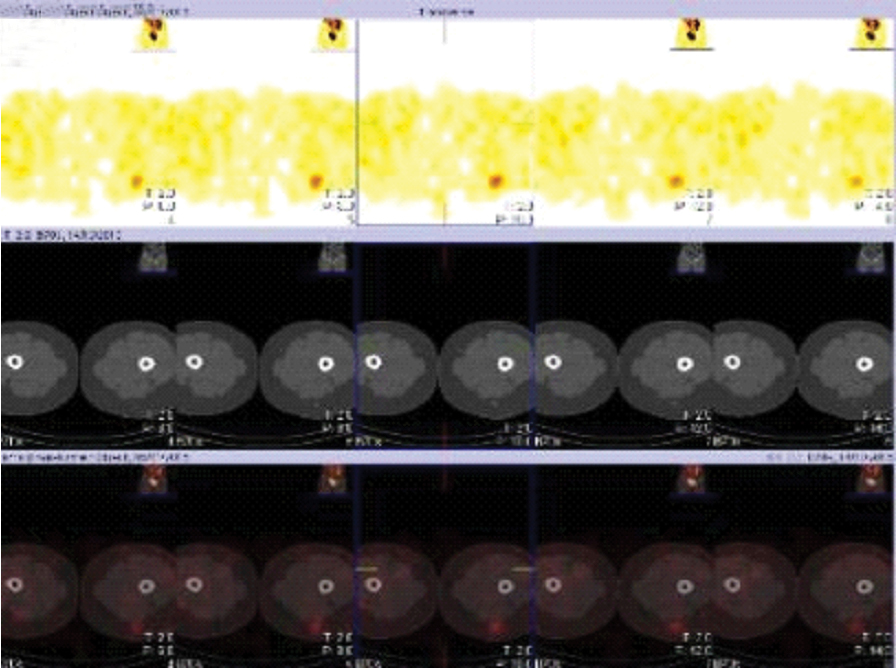
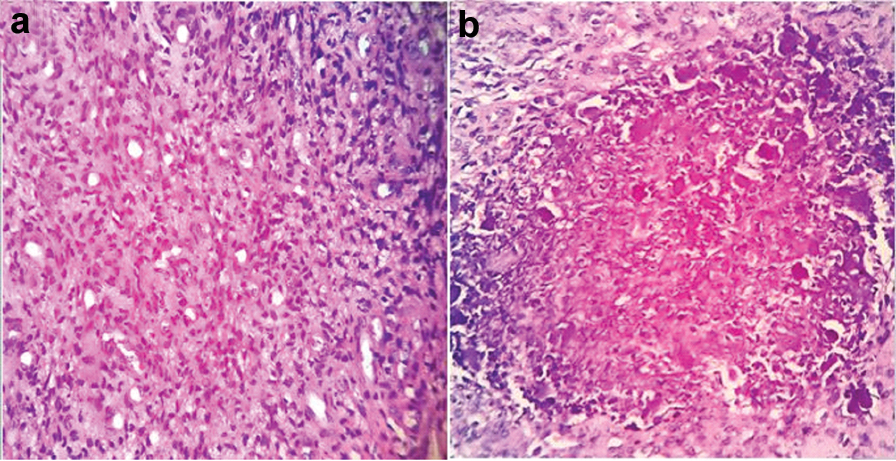
Bone scan revealed multiple old healed fractures. Magnetic Resonance Imaging (MRI) thigh showed a well-defined T1 hypointense, T2 hyperintense lesion in the subcutaneous plane of left posterior thigh [Table/Fig-2], which corresponded spatially with the octreotide receptor scintigraphy scan featuring increased uptake in the thigh lesion [Table/Fig-3]. It was subcentimetric in size. Lesion was excised by ultrasonographic aid. Histopathological sections from the specimen revealed two tiny circumscribed unencapsulated spindle cell lesions separated by fibroadipose tissue and each measuring 0.7 cm in greatest dimension. The bland appearing streaming, spindle cells were arranged with vessels in a haemangiopericytomatous pattern, amidst which were foci of speckled grungy/blotchy calcification and hyalinised collagen [Table/Fig-4]. Mitosis was inconspicuous. Correlating with clinical, biochemical and radiological findings, a histopathological diagnosis of Phosphaturic Mesenchymal Tumour of the Mixed Connective Tissue Type (PMTMCT) was made.
MRI thigh showed a well-defined T1 hypointense, T2 hyperintense lesion in the subcutaneous plane of left posterior thigh.
Octreotide receptor scintigraphy scan showed increased uptake in the thigh lesion.
a) Bland appearing streaming, spindle cells arranged with vessels in a haemangiopericytomatous pattern (H&E, 40X); b) Foci of speckled grungy/blotchy calcification (H&E, 40X).
The serum calcium and phosphorus levels were monitored after excision. Serum calcium was 9.2 mg/dl (NR, 9– 11) and serum phosphorus was 2.7 mg/dl (NR, 2.5– 4.5), which proved confirmatory for the diagnosis of oncogenic osteomalacia. The patient is currently asymptomatic and is on regular follow up.
Discussion
Oncogenic osteomalacia, also known as tumour induced osteomalacia, is a rare paraneoplastic syndrome caused by mesenchymal tumours [1]. These tumours secrete proteins known as phosphatonins which include FGF-23, FGF-7, secreted frizzled-related protein 4 and matrix extracellular phosphoglyco protein [1]. However, FGF-23 is the only clinically relevant protein amongst them [2]. FGF-23 acts by inhibiting the sodium-phosphate renal co-transporters and suppresses 1 -hydroxylase activity [3]. As a result, there is decreased renal resorption and increased urine excretion of the phosphate [3]. Thus, the biochemical findings include hypophosphatemia and low 1,25-dihydroxy vitamin D [1,2].
Most of the oncogenic osteomalacia tumours are located either in bone or soft tissue [1]. The tumours are mostly solitary and usually benign in nature [3,4]. These tumours are common in middle-aged individuals, although the age range can vary considerably, with male-to-female ratio of 1.2:1 [3,4]. Oncogenic osteomalacia usually presents with progressive, generalised bone pain and muscle weakness, and radiology reveals signs of osteopaenia such as Looser’s zone or multiple fractures [1]. However, symptoms are often non-specific leading to delay in diagnosis [3]. The present case is a 29-year-old female, who presented with generalized diffuse bone pain and right fibular xeroradiography showed Looser’s zone.
The differential diagnosis for hypophosphatemia can be classified into acquired and genetic causes. Most of the acquired causes of hypophosphatemia are due to direct renal tubular damage by drugs or toxins. Renal Fanconi syndrome, haematological malignancies, total parenteral nutrition, organ transplant, refeeding syndrome, correction of diabetic ketoacidosis and dietary deficiency are other disorders implicated with hypophosphatemia [3]. In the present case, renal Fanconi syndrome was ruled out based on absent urinary sugars and protein. Genetic diseases such as ARHPR, ADHPR and XLHPR may have an onset in childhood or may be associated with a positive family history [1]. In the present case, negative family history ruled out the possibility of the heritable forms of phosphopenic osteomalacia, namely ARHPR, ADHPR and XLHPR. Hence, the suspicion of a tumour producing FGF-23 arose.
The tumours causing oncogenic osteomalacia are usually very small, slow-growing, and difficult to locate [1]. Whole-body Tc-99m sestamibi scanning, octeotride scintigraphy, 18F-fluorodeoxyglucose (FDG) Positron Emission Tomography (PET), whole body MRI and computed tomography are used for localization of these tumours [1,2]. It is difficult to recommend one modality over another, and the choice primarily depends on availability [2]. In the present case octeotride scintigraphy revealed a subcentimetric lesion in the subcutaneous plane of left posterior thigh.
Approximately 340 cases of oncogenic osteomalacia have been reported [1]. The prototypical causative tumours are phosphaturic mesenchymal tumours [3]. About 70% to 80% of these are PMTMCT [4]. Osteoblastoma-like tumours, ossifying fibrous-like tumours and non-ossifying fibrous-like tumours are the other subtypes [5]. Histologically, these tumours are characterized by bland appearing spindle shaped to stellate cells, hyalinised to myxoid appearing matrix which undergoes calcification in a flocculent fashion also described as grungy calcification eliciting a giant cell response of the osteoclast type [4]. Haemangiopericytoma-like pattern of capillary network is classically seen in almost all the cases [4]. Mitosis figures are absent. Immunohistochemically, the tumour cells are positive for FGF-23 and vimentin [2]. The blood vessels are identified by CD34 however, the tumour cells are negative for CD34 [2]. Lymphatic vessels are identified by expression of the lymphatic endothelial cell marker lymphatic vessel endothelial hyaluronan receptor-1 (LYVE-1) [6]. Usually PMTMCTs are benign with less than 13% being recurrent or metastatic [6].
Oncogenic osteomalacia has a good prognosis because the responsible tumour is usually benign [1]. Surgical removal of the tumour results in dramatic improvement [2]. In the present case, there was normalization of the metabolic dysfunction post excision of the subcentimetric lesion.
Conclusion
Oncogenic osteomalacia is a rare paraneoplastic syndrome caused by mesenchymal tumours with characteristic biochemical findings of hypophosphatemia and low 1,25-dihydroxy vitamin D. Proper diagnosis requires a thorough clinical history, biochemical parameters, assessment of renal tubular phosphate and imaging studies to identify the cause. It has a good prognosis as surgical removal of the tumour results in dramatic improvement.
[1]. Pithankhuakul K, Ratanasuwan T, Thanakit V, Sukhantanak B, Kiatisevi P, Oncogenic osteomalacia caused by phosphaturic mesenchymal tumours in the proximal and shaft of the tibia: A case reportJ Orthop Surg (Hong Kong) 2014 22:257-62. [Google Scholar]
[2]. Sahoo J, Balachandran K, Kamalanathan S, Das AK, Patro DK, Halanaik D, Tumour(s) induced osteomalacia-A curious case of double troubleJ Clin Endocrinol Metab 2014 99:395-98. [Google Scholar]
[3]. Chong WH, Molinolo AA, Chen CC, Collins MT, Tumour-induced osteomalaciaEndocr Relat Cancer 2011 18:R53-R77. [Google Scholar]
[4]. Folpe AL, Fanburg-Smith JC, Billings SD, Bisceglia M, Bertoni F, Cho JY, Most osteomalacia-associated mesenchymal tumours are a single histopathologic entity: An analysis of 32 cases and a comprehensive review of the literatureAm J Surg Pathol 2004 28:1-30. [Google Scholar]
[5]. Weidner N, Santa Cruz D, Phosphaturic mesenchymal tumours. A polymorphous group causing osteomalacia or ricketsCancer 1987 59:1442-54. [Google Scholar]
[6]. Hannan MF, Athanasou NA, Teh J, Gibbons CLMH, Shine B, Thakker RV, Oncogenic hypophosphataemic osteomalacia: Biomarker roles of fibroblast growth factor 23, 1,25-dihydroxyvitamin D3 and lymphatic vessel endothelial hyaluronan receptor 1Eur J Endocrinol 2008 158:265-71. [Google Scholar]