Juvenile nasopharyngeal angiofibroma is tumour almost exclusively seen in adolescent males, constituting less than 1% of all neoplasms in head and neck. They are benign and locally spreading and are highly vascular in nature and thus prove to be a surgical challenge because of its complex anatomical location. Here, we present a case report of a 18-year-old male presenting with a mass in his left nasal cavity, with recurrent epistaxis and nasal obstruction. Computed tomography imaging revealed a non-encapsulated lobulated heterogeneous mass lesion in the naso-pharynx and left posterior choana of the nasal cavity, extending to pterygopalatine and infratemporal fossa, masseter space of left side. The approach to its surgical management was a combined multi-disciplinary effort of otorhinolaryngology surgeons and maxillofacial surgeons.
Case Report
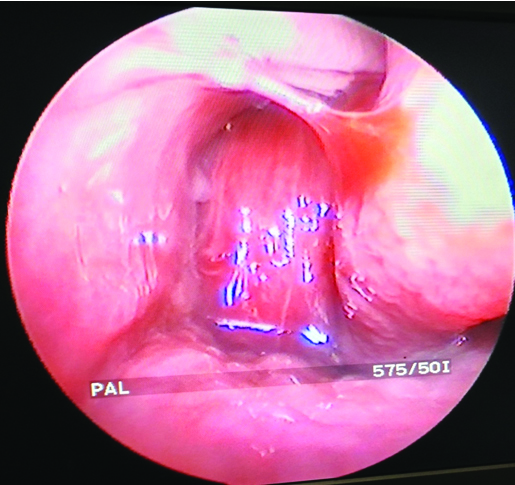
A 18-year-old male presented with chief complains of nasal obstruction which was unilateral (left), progressive, epistaxis, continuing nasal discharge since two months, with a mass in his nasal cavity. He had intermittent headache which used to be relieved by simple analgesics with nasal bleeding episodes that lasted for 10-15 minutes actively and serous discharge pervasive over a two month period. On presentation, he had one episode of painless epistaxis, loosing approximately 40-50 ml of blood, for which he was referred to our centre. Past history reveals no episodes of nasal bleeding before two months but intermittent nasal discharge. Patient had no clinical pallor but mouth breathing was evident, specifically complained during sleep. Endoscopic examination of the nose reveals that the mass was congested, compressible, filling the left inferior and middle meatus, extending back filling the choana with active serous discharge with tinges of blood clots, probably from previous nasal bleed [Table/Fig-1]. There was no tenderness on palpation and no external facial deformity. Probe test revealed no attachments in the nasal cavity. On posterior rhinoscopy the mass could be seen extending to nasopharynx in the region of fossa of rosenmuller and beyond.
Endoscopic examination of nose showing the mass.
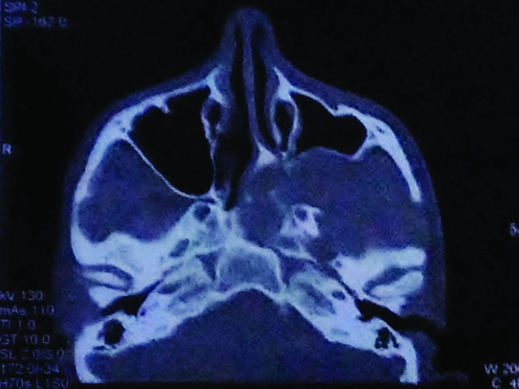
The oro-dental examination was normal. General examination revealed no significant abnormality. Routine haematological investigations were found to be within the normal limits. Fine-needle aspiration was carried out with caution in an operating room and revealed only blood. Computed tomography revealed a non-encapsulated lobulated heterogeneous soft tissue dense mass lesion taking significant enhancement on Intra Venous (IV) contrast injection, in naso-pharynx and left posterior choana of the nasal cavity, extending upto pterygopalatine and infratemporal fossa, masseter space of left side and involving the pterygoid muscles; ipsilateral sphenoid sinus and posterior ethmoid cells were also infiltrated. There was anterior bowing of posterior wall of ipsilateral maxillary sinus. The osteomeatal complex was invaded with erosion of the middle and inferior turbinate [Table/Fig-2].
Computed tomography view.
Post-operative period was uneventful. The patient was discharged after three days. On follow up nasal endoscopy was done after 15 days and after three months. Nasal cavity was healthy and no signs of recurrence was seen.
Surgical Procedure
The surgery was done under general hypotensive anaesthesia with patient in supine reverse Trendelenberg [1] position and intraoral delivery of endotracheal tube.
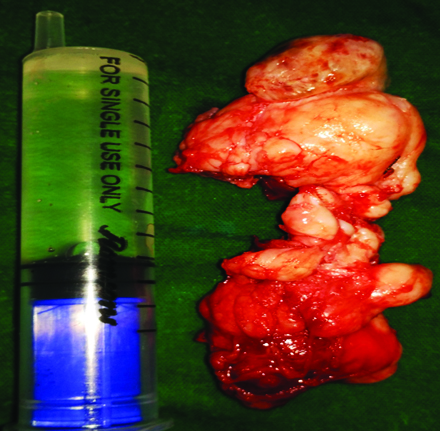
The surgical approach chosen was midfacial degloving approach with Le Fort Type 1 osteotomy, with maxillary downfracture and delivery of the tumour, refixation and soft tissue closure. After removal of the tumour [Table/Fig-3], the site of origin was carefully inspected with a flexible fibre-optic endoscope and revealed no remnant tumour tissue or significant bleeding vessels. It was packed with a patch of gel foam.
Discussion
Juvenile Nasopharyngeal Angiofibroma (JNA) is a rare tumour presenting mostly in adolescent males. Hippocrates described this tumour in the fifth century AD, but Friedberg first used the term angiofibroma in 1940 [2]. The average age of presentation of this tumour is 14 years. The reason for exclusivity in males is hypothesised as androgen dependence of the tumour [3]. JNA originates within the sphenopalatine foramen, and further spreads locally into the pterygopalatine fossa, nasal cavity and paranasal sinuses. Patients usually present with a triad of progressive nasal obstruction, recurrent epistaxis and mass in the nasal cavity and nasopharynx. It has potency to cause proptosis, affecting both the orbit and with intracranial extension, eventually leading to cranial nerve palsies and loss of vision [4].
However, advanced stages of the tumour can present as locally invasive causing facial dysmorphism, Eustachian tube obstruction causing conductive hearing loss, and diplopia that occurs secondary to erosion of superior orbital fissure and due to third and sixth nerve palsy, intraorbital extension leading to proptosis, or rarely anosmia, recurrent otitis media and eye pain [1]. The most common site of initiation is posterolateral wall of the nasopharynx, precisely at the trifurcation of the sphenoidal process of the palatine bone, the roof of the pterygoid process and the horizontal process of the vomer [2]. Differential diagnosis includes antrochonal polyp, rhinosporidiosis, sinonasal malignancy chordoma, nasopharyngeal cyst and pyogenic granuloma.
The origin of JNA is from a hamartomatous nidus of vascular tissue in the region of the sphenopalatine foramen, which is being stimulated during early pubertal period by endogenous androgenic hormones [5,6].
Radiographic findings suggestive of the disease is the anterior bowing of the posterior wall of maxillary sinus of same side (Holman Miller Antral Sign) which is considered as pathognomonic by some. Diagnosis of an angiofibroma essentially includes preoperative CT-scan, with MRI and Magnetic Resonance Angiography (MRA).
Coronal CT provides good hard tissue imaging to show invasion of the cancellous bone of the sphenoid. They are critical in the staging of the tumour, peri-tumour anatomy, and extension, based on which treatment options can be planned weighing prognosis. For detecting intracranial extension of the tumour into soft tissues of the skull base; MRI is far more superior to CT. Hence, in adequate setups, it is better to carry out both procedures for deciding the operative approach and prognosis [7]. MRI is even more important postoperatively to show any residual or recurrent tumour and monitor the effects of radiotherapy.
Recurrence results from deeper extension of the tumour resulting in residual tissue after surgery. Commonly, the vascular supply to JNAs is primarily from distal Internal Maxillary Artery (IMA) branches, particularly the sphenopalatine, descending palatine and posterior superior alveolar branches. JNAs may also be supplied by the ascending pharyngeal artery. So, preoperative embolization of feeder vessels i.e., super selective embolization of external carotid artery can be done to reduce blood loss without significant neurological complications [8]. There is no definite benefit of transarterial over direct tumoural embolization [9].
Histologically, JNAs originate from myofibroblasts. The tumour usually spreads submucosally and is non-encapsulated. It is composed of intricate mixture of stellate and staghorn blood vessels with variable vessel wall thickness ranging from single layer of endothelium to variable smooth muscle coat, irregular fibrous stroma (loose, oedematous to dense, acellular) positive stains include c-Kit/CD117, androgen receptor (75%) [10].
Surgery remains the main stay in management [11]. Endoscopic nasal microsurgery is a viable approach with prospectively lesser postoperative morbidity and intraoperative blood loss, but it is advocated only for limited lesions. But for larger tumours, approaches such as transpalatal, lateral rhinotomy and midfacial degloving have been suggested. Preoperative embolisation of tumour is recommended with all of these approaches to limit the intraoperative blood loss [4].
The advantage of endoscopic approach over open surgery is a shorter mean duration of surgery [12]. Complications of the surgical approach used in our case were mild midfacial pain following two months after surgery which gradually subsided and nasal synechiae which was managed with intranasal stents and nasal douching.
Conclusion
JNA, occuring almost exclusively in adolescent males is a benign, rare tumour of the nasopharynx. Clinically, it can be diagnosed with a sustainable set of features as recurrent epistaxis, nasal obstruction and mass in the nasal cavity.
The size as percieved of the nasopharyngeal tumour is not necessarily in accordance with the real tumour extension and size, it can be only the "tip of the iceberg".
A contrast CT is pathognomonic for the diagnosis of JNA and allows accurate staging of the tumour which is necessary for choosing the surgical technique, estimating prognosis and reporting results. MRI and angiography are also preferred as collateral diagnostic techniques for surgical planning.
Open surgery was preferred over endoscopic in our case due to lateral extension of the tumour to infratemporal fossa. Radiotherapy must be reserved for inoperable cases, for recurrences or for patients who refuse surgery because of various reasons.
[1]. Available from https://en.wikipedia.org/wiki/Nasopharyngeal_angiofibroma [Google Scholar]
[2]. Mehmet A, Orhan S, Suphi M, Juvenile nasopharyngeal angiofibroma: Radiological evaluation and pre-operative embolizationKBB Forum 2006 5:58-61. [Google Scholar]
[3]. Antonelli AR, Cappiello J, Di Lorenzo D, Donajo CA, Nicolai P, Olandi A, Diagnosis, staging, and treatment of juvenile nasopharyngeal angiofibroma (JNA)Laryngoscope 1987 97:1319-25. [Google Scholar]
[4]. Alves FRA, Granato L, Soares M, Lambert E, Surgical approaches to juvenile nasopharyngeal angiofibroma - case report and literature reviewIntl. Arch. Otorhinolaryngol 2006 2(10):162-66. [Google Scholar]
[5]. McDaniel RK, Houston GD, Juvenile nasopharyngeal angiofibroma with lateral extension into the cheek: Report of caseJ Oral Maxillofac Surg 1995 53:473-76. [Google Scholar]
[6]. Harrison DF, The natural history, pathogenesis, and treatment of juvenile angiofibroma. Personal experience with 44 patientsArch Otolaryngol Head Neck Surg 1987 113:936-42. [Google Scholar]
[7]. Lloyd G, Howard D, Phelps P, Cheeseman A, Diver J, Juvenile angiofibroma: Modern imaging and its influence on the surgical treatment of juvenile angiofibromaJ Laryngol Otol 1999 113(2):127-34. [Google Scholar]
[8]. Elhammady MS, Johnson JN, Peterson EC, Aziz-Sultan MA, Preoperative embolization of juvenile nasopharyngeal angiofibromas: Transarterial versus direct tumoural punctureWorld Neurosurg 2011 76(3-4):328-34. [Google Scholar]
[9]. Available from http://www.pathologyoutlines.com/topic/nasalangiofibroma.html [Google Scholar]
[10]. Oliveira JA, Tavares MG, Aguiar CV, Azevedo JF, Sousa JR, Almeida PC, Comparison between endoscopic and open surgery in 37 patients with nasopharyngeal angiofibromaBraz J Otorhinolaryngol 2012 78(1):75-80. [Google Scholar]
[11]. Mair EA, Battiata A, Casler JD, Endoscopic laser assisted excision of juvenile nasopharyngeal angiofibromaArch Otolaryngol Head Neck Surg 2003 129:454-59. [Google Scholar]
[12]. Radkowski D, McGill T, Healy GB, Ohlms L, Jones DT, Angiofibroma. Changes in staging and treatmentArch Otolaryngol Head Neck Surg 1996 122(2):122-29. [Google Scholar]