Immediate Placement of Zirconia Implants in Teeth with Periapical Lesions: A Case Report
Nizar A Ahmed1, Caroline Annette Jacob2, Preetham Prasad Nittla3
1 Senior Lecturer, Department of Periodontics, Thai Moogambigai Dental College, Chennai, Tamil Nadu, India.
2 Senior Lecturer, Department of Periodontics, Saveetha Dental College, Chennai, Tamil Nadu, India.
3 Senior Lecturer, Department of Prosthodontics, Saveetha Dental College, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Caroline Annette Jacob, Senior Lecturer, Department of Periodontics, Saveetha Dental College, No 102 PH Road, Chennai-77, Tamil Nadu, India.
E-mail: caroline_jacob@ymail.com
This case report records the replacement of two failed endodontically treated mandibular molars with one piece zirconia implants in a patient with metal hypersensitivity. The two molars were atraumatically extracted and curetted to remove any remnants of a periapical granuloma. Immediate implant placement with primary stability was achieved using one piece WhiteSky® Bredent zirconia implants which were restored after four months with a zirconia crown. One year follow up revealed successful osseointegration with optimal form and function.
Failed endodontic therapy, Mandibular molars, Metal hypersensitivity, Periapical infection, Zirconia dental implants
Case Report
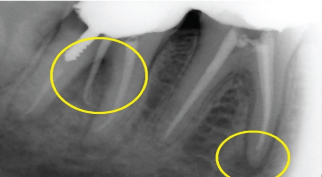
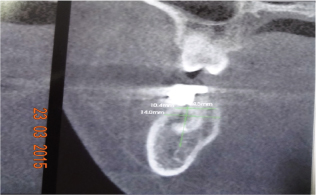
A 29-year-old female patient reported to the dental operatory with the chief complaint of pain in relation to the right lower back tooth region. The pain was sudden in onset and aggravated during mastication. The patient also gave a history of a metal allergy that presented as erythema on wearing artificial jewellery. Clinical examination in relation to teeth #46 and 47 revealed tenderness on percussion. Both teeth were endodontically treated one year prior to presentation and rehabilitated with Porcelain Fused Metal (PFM) crowns with no gingival recession [Table/Fig-1,2]. Radiographic examination revealed recurrent caries beneath the crowns with mild root resorption and an associated periapical lesion in relation to tooth #46. There was also Grade III furcation involvement of tooth #47 [Table/Fig-3] Adequate bone height and width were present as verified using CBCT [Table/Fig-4]. The poor prognosis of re-endodontic treatment was explained and the patient wanted a more definitive treatment. The teeth were hence decided to be extracted and immediately replaced with one piece zirconia implants.
Preoperative lateral view of teeth #46 and 47.

Preoperative occlusal view of teeth #46 and 47.

Periapical radiolucency in relation to the mesial root of tooth #46 and presence of Grade III furcation involvement in tooth #47. The vertical component of the furcation can be observed in this RVG by inserting a guttapercha point.
Adequate bone width and height determined by CBCT.
Surgical Procedure
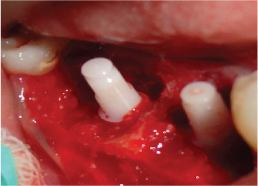
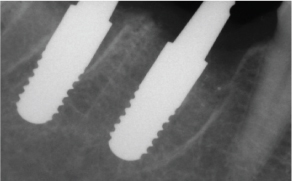
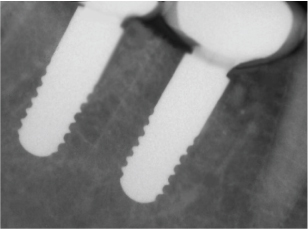
Thorough ultrasonic scaling and maintenance was performed prior to extraction and implant placement. Under 1:2,00,000 adrenaline in local anaesthetic (Lignox®), atraumatic extraction was performed using a periotome in relation to teeth #46 and 47. The extraction sockets were thoroughly debrided using bone curettes to remove the granulation tissue. The osteotomy sites were prepared using a pilot drill followed by verification using direction indicators. Sequential drilling was done up to the final dimension of the implant and two 4.5x10 mm WhiteSKY® Bredent Medical zirconia implants [Table/Fig-5] were placed in relation to teeth #46 and 47 [Table/Fig-6]. Primary stability was achieved at 35 Ncm. Particulate bone graft (OsseoGraft, Advanced Biotech, Chennai) was placed to fill the void between the implant and the tooth socket. The graft was held in place with HealiGuide membrane (Advanced Biotech, Chennai) and the site was approximated with 3-0 black silk sutures. It was decided to place the abutment in infra-occlusion and place the crown at a later stage. The immediate postoperative radiograph revealed parallel and well seated implants [Table/Fig-7]. Postoperative homecare instructions were given which included tooth brushing, 0.12% chlorhexidine rinse and postoperative medication: amoxicillin 500 mg and metronidazole 400 mg thrice daily for five days along with paracetamol for three days. Sutures were removed after seven days, at which time adequate wound healing was seen. Impressions were made after four months and subsequently zirconia crowns were loaded in relation to teeth #46 and 47. Since, the implant in relation to tooth #46 was placed more apically [Table/Fig-7] in relation to the adjacent natural tooth #45; an FP2 type of prosthesis was placed. [Table/Fig-8] The occlusion for both crowns were verified with 12 μ thick articulating paper. One year postoperative review revealed no evidence of mobility, paresthesia, bone loss or a peri-implant lesion. The peri-implant soft tissue around the site showed no signs of inflammation. Postoperative radiograph shows an appreciable gain in the alveolar bone height due to Guided Bone Regeneration (GBR) [Table/Fig-9].
4.5x10 mm one piece zirconia implant.

One piece WhiteSky® zirconia implants placed in relation to teeth #46 and 47.
Implant parallelism seen in teeth #46 and 47 when compared to tooth #45. Implant in tooth #46 is positioned apically in relation to tooth #45.
Restoration of teeth #46 and 47 using zirconia crowns. An FP2 type of prosthesis can be noted in tooth #46.

One year post operative radiograph.
Discussion
Zirconia implants are being considered for their advantages of aesthetics, lack of galvanic reactions [1] and lesser risk of inflammation as compared to the accidental introduction of titanium particles in the osteotomy site [2]. Twenty years of evidence has suggested that zirconia based implants are highly biocompatible [3,4] and also possess favourable physical properties [5]. There have been evidences of zirconia being able to withstand long term loads [6], implying that they appear to be satisfactory to use in case of posterior teeth as well.
Allergic reactions to titanium has not been much documented in dental literature. Placing permanent metallic dental implants in allergic patients can cause either Type 1 or Type 4 hypersensitivity reaction [7]. Sicilia A et al., in 2008 studied the prevalence of titanium allergy in 1500 continuous patients and estimated a low prevalence at 0.6% of all subjects evaluated [7]. The patient in this case report had a history of metal allergy that presented as erythema on wearing artificial jewellery. A clinical report by Egusa H et al, demonstrated the presence of facial eczema as a result of titanium dental implants. The condition was resolved on removal of the dental implant [8]. There are no case reports reporting zirconia implant placement in a patient with known metal allergy. As the patient did not want any metallic implants; it was decided to use a one piece zirconia implant. The lack of a microgap in single piece implants compared to two-piece dental implants ensures minimal microleakage and bacterial colonization that could result in marginal bone loss [9].
Conventional protocols regarding implant placement and loading in areas of a periapical infection dictate that implants be delayed several months post extraction in order to prevent infection of the implant surfaces that may result in failure [10,11]. However, in waiting for the resolution of the lesion; inadvertent bone loss tends to occur, compromising aesthetics and function [12]. The amount of crestal bone resorption after extraction of tooth can extend upto 23% over a six month period thereby compromising hard and soft tissue architecture [13,14]. Findings from a systematic review suggests that implants can be placed into sites with periodontal and periapical infections [15].
In this report, a thorough surgical debridement was performed prior to the placement of the dental implant. GBR was also done in order to fill up the tooth socket-dental implant gap. These procedures were in accordance with the evidence found in the systematic review by Waasdorp JA et al, [15]. A multi centre randomized controlled trial also failed to observe any clinical differences between implant survival, complications and marginal bone level changes when loading single implants immediately, early or conventionally [16]. A systematic review and meta-analysis that reviewed the protocols for immediate placement and loading/restoration of single implants in molar sites provided encouraging results of over 99% and 97.9% implant survival rates respectively [17]. Studies performed both retrospectively and prospectively also appear to support immediate implant placement even in areas of a periapical pathology. A retrospective analysis (mean follow up period of 67.3 months) of 418 immediately placed implants exhibiting a periapical pathology demonstrated a cumulative survival rate of 97.8% [18]. Another retrospective study compared the survival rates of immediate implants with and without periapical pathologies [19]. Of the 922 implants, 285 were placed into sockets with periapical radiolucencies (mean follow up period of 19.75 months). The success rates between the study and control group was 97.5% and 98.7% respectively which was statistically insignificant. Interestingly, a statistically higher failure rate was found for implants placed adjacent to retained teeth with a periapical lesion. In a prospective controlled clinical trial, 13 immediate implants were placed in a site exhibiting a periapical pathology against 16 immediate implants in healthy sites. In both groups, primary stability was achieved with no differences seen between the clinical and radiographic parameters [20]. Jung RE et al placed immediate implants in sites with and without a periapical pathology with a 100% survival rate, five years post placement [21]. It is also important to note that these studies have emphasized on eliminating the pathology both mechanically and chemotherapeutically while advocating GBR where required [15]. Zirconia-implant surfaces also tend to accumulate fewer bacteria as compared to titanium surfaces [22,23]. This could prevent an inflammatory gingival response that could exacerbate a previous periapical lesion. A decrease in the bacterial load encourages the formation of a biological width and a mucosal seal that could prevent any apical migration of bacteria [9,24,25].
Conclusion
The placement of immediate zirconia implants may be beneficial in areas of previous periapical infection; provided, a thorough surgical debridement of the infected site is supplemented with GBR, adequate antibiotic coverage and maintenance.
[1]. Tschernitschek H, Borchers L, Geurtsen W, Nonalloyed titanium as a bioinert metal-A reviewQuintessence International 2005 36(7-8):523-30. [Google Scholar]
[2]. Sterner T, Schutze N, Saxler G, Jakob F, Rader CP, Effects of clinically relevant alumina ceramic, zirconia ceramic and titanium particles of different sizes and concentrations on TNF-alpha release in a human macrophage cell lineBiomed Tech (Berl) 2004 49(12):340-44. [Google Scholar]
[3]. Ichikawa Y, Akagawa Y, Nikai H, Tsuru H, Tissue compatibility and stability of a new zirconia ceramic in vivoJ Prosthet Dent 1992 68(2):322-26. [Google Scholar]
[4]. Degidi M, Artese L, Scarano A, Perrotti V, Gehrke P, Piattelli A, Inflammatory infiltrate, microvessel density, nitric oxide synthase expression, vascular endothelial growth factor expression, and proliferative activity in peri-implant soft tissues around titanium and zirconium oxide healing capsJ Periodontol 2006 77(1):73-80. [Google Scholar]
[5]. Piconi C, Maccauro G, Zirconia as a ceramic biomaterialBiomaterials 1999 20(1):1-25. [Google Scholar]
[6]. Kohal RJ, Wolkewitz M, Tsakona A, The effects of cyclic loading and preparation on the fracture strength of zirconium-dioxide implants: An in vitro investigationClin Oral Implants Res 2011 22(8):808-14. [Google Scholar]
[7]. Sicilia A, Cuesta S, Coma G, Arregui I, Guisasola C, Ruiz E, Titanium allergy in dental implant patients: a clinical study on 1500 consecutive patientsClinical Oral Implants Research 2008 19(8):823-35. [Google Scholar]
[8]. Egusa H, Ko N, Shimazu T, Yatani H, Suspected association of an allergic reaction with titanium dental implants: A clinical reportThe Journal of Prosthetic Dentistry 2008 100(5):344-47. [Google Scholar]
[9]. Borgonovo AE, Fabbri A, Vavassori V, Censi R, Maiorana C, Multiple teeth replacement with endosseous one-piece yttrium-stabilized zirconia dental implantsMed Oral Patol Oral Cir Bucal 2012 17(6):e981-87. [Google Scholar]
[10]. Quirynen M, Gijbels F, Jacobs R, An infected jawbone site compromising successful osseointegrationPeriodontology 2000 2003 33:129-44. [Google Scholar]
[11]. Rosenquist B, Grenthe B, Immediate placement of implants into extraction sockets: implant survivalThe International journal of oral & maxillofacial implants 1996 11(2):205-09. [Google Scholar]
[12]. Covani U, Ricci M, Bozzolo G, Mangano F, Zini A, Barone A, Analysis of the pattern of the alveolar ridge remodelling following single tooth extractionClin Oral Implants Res 2011 22(8):820-25. [Google Scholar]
[13]. Carlsson GE, Persson G, Morphologic changes of the mandible after extraction and wearing of dentures. A longitudinal, clinical, and x-ray cephalometric study covering 5 yearsOdontologisk revy 1967 18(1):27-54. [Google Scholar]
[14]. Atwood DA, Coy WA, Clinical, cephalometric, and densitometric study of reduction of residual ridgesThe Journal of Prosthetic Dentistry 1971 26(3):280-95. [Google Scholar]
[15]. Waasdorp JA, Evian CI, Mandracchia M, Immediate placement of implants into infected sites: A systematic review of the literatureJournal of Periodontology 2010 81(6):801-08. [Google Scholar]
[16]. Grandi T, Guazzi P, Samarani R, Tohme H, Khoury S, Sbricoli L, Immediate, early (3 weeks) and conventional loading (4 months) of single implants: Preliminary data at 1 year after loading from a pragmatic multicenter randomised controlled trialEuropean Journal of Oral Implantology 2015 8(2):115-26. [Google Scholar]
[17]. Atieh MA, Payne AG, Duncan WJ, de Silva RK, Cullinan MP, Immediate placement or immediate restoration/loading of single implants for molar tooth replacement: a systematic review and meta-analysisInt J Oral Maxillofac Implants 2010 25(2):401-15. [Google Scholar]
[18]. Fugazzotto P, A retrospective analysis of immediately placed implants in 418 sites exhibiting periapical pathology: Results and clinical considerationsInt J Oral Maxillofac Implants 2012 27(1):194-202. [Google Scholar]
[19]. Bell CL, Diehl D, Bell BM, Bell RE, The immediate placement of dental implants into extraction sites with periapical lesions: A retrospective chart reviewJournal of Oral and Maxillofacial Surgery : Official Journal of the American Association of Oral and Maxillofacial Surgeons 2011 69(6):1623-27. [Google Scholar]
[20]. Siegenthaler DW, Jung RE, Holderegger C, Roos M, Hammerle CH, Replacement of teeth exhibiting periapical pathology by immediate implants: A prospective, controlled clinical trialClin Oral Implants Res 2007 18(6):727-37. [Google Scholar]
[21]. Jung RE, Zaugg B, Philipp AO, Truninger TC, Siegenthaler DW, Hammerle CH, A prospective, controlled clinical trial evaluating the clinical radiological and aesthetic outcome after 5 years of immediately placed implants in sockets exhibiting periapical pathologyClin Oral Implants Res 2013 24(8):839-46. [Google Scholar]
[22]. Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A, Bacterial adhesion on commercially pure titanium and zirconium oxide disks: An in vivo human studyJ Periodontol 2004 75(2):292-96. [Google Scholar]
[23]. Rimondini L, Cerroni L, Carrassi A, Torricelli P, Bacterial colonization of zirconia ceramic surfaces: an in vitro and in vivo studyInt J Oral Maxillofac Implants 2002 17(6):793-98. [Google Scholar]
[24]. Depprich R, Naujoks C, Ommerborn M, Schwarz F, Kubler NR, Handschel J, Current findings regarding zirconia implantsClin Implant Dent Relat Res 2014 16(1):124-37. [Google Scholar]
[25]. Van Dooren E, Calamita M, Calgaro M, Coachman C, Ferencz JL, Pinho C, Mechanical, biological and clinical aspects of zirconia implantsEur J Esthet Dent 2012 7(4):396-417. [Google Scholar]