Postoperative steroid (systemic/topical) after Endoscopic Sinus Surgery (ESS) has been considered as the standard medical treatment for the control of the disease in AFRS. Although most of the patients get benefitted by medical treatment, recurrence has been noticed in significant proportion of patients even in the immediate postoperative period. Again steroids are claimed to have promising results for the management of AFRS but prolonged use of systemic steroid is not always advised because of its systemic toxicity and some patients also do not respond to it. Considering the aetiology of AFRS, antifungals (Itrconazole) have been tried in the past decade by different authors which aimed at declining the recurrence rate and acts by inhibiting the fungal growth in the postoperative period as described in the past literature [1]. In the current study, we have compared the efficacy between steroid and the Itraconazole in preventing the recurrence of the disease in patients with AFRS.
Materials and Methods
This prospective study was conducted in the Department of Otorhinolaryngology at VMMC and Safdarjung Hospital, New Delhi, India, from October 2013 to February 2015. Total 60 patients with AFRS with nasal polyposis, diagnosed by Bent-Kuhn’s criteria [2] were included in the study. All patients of AFRS between the age group of 5-60 years were included in the study. Patients with revision surgery and those have been suffered from chronic systemic illness were excluded, anticipating systemic toxicity of steroid and itraconazole.
Patients were divided into two groups; Group A and Group B each containing 30 patients each. Sino-Nasal Outcome Test (SNOT-20) scoring was calculated for each preoperative patient. Haematological evaluation (complete blood count, absolute eosinophil count) immunological (Serum IgE) and intradermal skin test for fungal Aspergillus species were carried out. AEC >500 mm3 was considered as elevated level. Preoperative non contrast Computed Tomography (CT) nose and paranasal sinus (CT scan with 3 mm axial and coronal cuts) was performed for each patient. Diagnostic nasal endoscopy was done in each patient for the assessment of nasal mass, nasal polyp, allergic mucin, and nasal discharge and were staged using Kupferberg endoscopic staging for fungal sinusitis. Patients were given a course of antibiotics, antihistaminic and systemic steroid for one week prior to ESS. All the patients were undergone Functional Endoscopic Sinus Surgery (FESS) by single surgeon. Intra-operatively nasal swabs were taken for cytological evaluation of charcot-layden crystals, fungal hyphae, allergic mucin, mast cells, eosinophils and basophil. The specimen (allergic mucin, debris, polyp) were sent for fungal microscopy, fungal culture and sensitivity and histopathological evaluation. Postoperatively all the patients were subjected to antibiotic and antihistaminic for one week. Patients of Group A (containing 30 patients), systemic steroid (oral prednisolone) was continued for one month and afterwards topical steroid (nasal spray) was continued till six months after surgery. In Group B (containing 30 patients), oral itraconazole (100 mg BID) was continued for six months after the surgery. Patients were followed at the end of first, third, and sixth months after surgery. At each visit, subjective and objective assessments [Sino-Nasal Outcome Test (SNOT-20) and Kupferberg endoscopic staging] were carried out. AEC and serum total IgE were repeated again at first, third and sixth months and compared with the preoperative values. Repeat NCCT nose and paranasal sinuses were done at the end of six months to look for recurrence of disease.
Statistical Analysis
Preoperative and postoperative data collected were compared with paired t-test.
Results
Description of the patients’ data has been demonstrated in [Table/Fig-1]. Of 30 patients in Group A, 20 were males and 10 were female. Similarly in Group B, 18 were males and 12 were females. Majority of patients in our study population were in the age group of 21-30 years i.e., 24 (40%), 14 (23.3%) patients were in the age group of 11-20 years, 12 (20.0%) in 41-50 years and 10 (16.7%) in the age group of 31-40 years. A total of 26 (43.3%) patients were suffering from disease for one to two years, 20 (33.3%) and 14 (23.3%) had a duration of symptoms for <one year and three to five years respectively. Nasal obstruction, nasal discharge and headache were found in 56 (93.3%), 32 (53.9%) and 16 (26.7%) of patients respectively. Four (6.7%) of the patients had decreased vision and 2 (3.3%) patients had proptosis in the preoperative period. Nasal discharge and allergic mucin were present in 42 (70.0%) and 40 (66.7%) patients respectively. Characteristic heterogeneous density in CT scan finding was present in all 60 (100%) patients. Nineteen cases (63.3%) were found positive for intradermal skin test for fungal Aspergillus species. Of 30 patients in Group A, two patients were absconded after three months of follow up and three patients in Group B had presented with deranged liver enzymes were excluded from the study.
Comparison of patients’ data between the two groups.
| Clinical characteristic | Group A | Group B |
|---|
| No of patients | 30 | 30 |
| Male | 20 | 18 |
| Female | 10 | 12 |
| Mean follow up period | 6 months | 6 months |
| Range | 3-8 months | 4-9 months |
| Pretreatment AEC | 532 μg/l | 578 μg/l |
| Post-treatment AEC | 482 μg/l | 438 μg/l |
| No of patients with normalized AEC | 0 | 0 |
| Pretreatment IgE | 886.20 IU/ml | 935 IU/ml |
| Post-treatment IgE | 620.00 IU/ml | 570 IU/ml |
| No of patients with normalized IgE | 18 | 20 |
| Pretreatment mean SNOT score | 52 .5 | 55.7 |
| Post-treatment mean SNOT score | 34.3 | 29.5 |
| Pretreatment Kupferberg’s endoscopic grading (Grade 4) | 100% | 100% |
| Post treatment Kupferberg’s endoscopic grading (Grade 0) | 7(23.33%) | 8(26.66%) |
| Recurrence of nasal polyp | 9(32.14%) | 7(25.92%) |
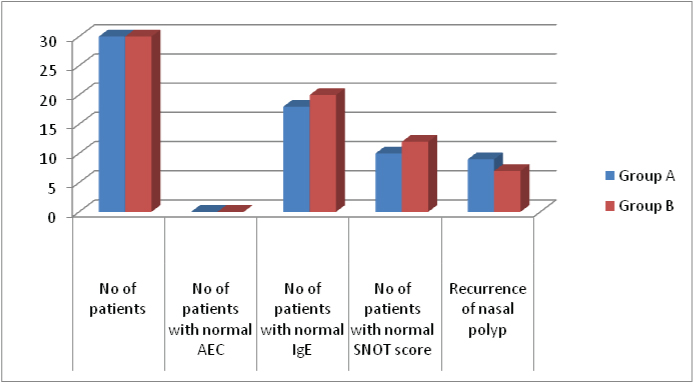
Ten (16.66%) cases from Group A and 8 (13.33%) from Group B had presented with elevated AEC in the preoperative period and it almost remained unchanged at the end of six months. The average pretreatment and post-treatment scores of AEC the patients in Groups A was 532 μg/l and 482 μ/l respectively. Similarly the corresponding values were in Group B were 578 μ/l and 438 μ/L respectively (p=0.912).
Of 60 cases, 44 cases (20 cases of Group A and 24 cases of Group B) presented with raised serum IgE in the preoperative period. At the end of one months, 18 patients in Group A and 20 patients in Group B had normal IgE level (p=0.80). The mean pre-operative serum IgE level in patients of Group A was 886.20 IU/ml and at first postoperative follow up, it was found to be 620 IU/ml which remained almost same till six months of follow-up. Again in Group B, the mean preoperative serum IgE was 935 IU/ml and at the end of one month it was 632 IU/ml and at the end of six months it was lowered to 570 IU/ml (p=0.555).
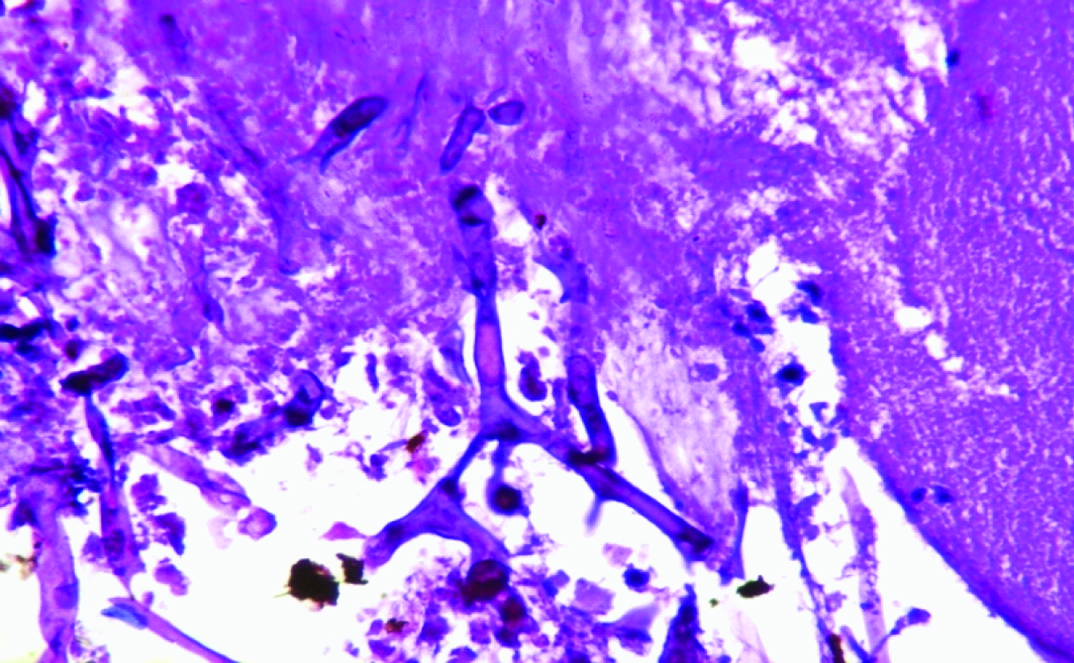
In the nasal smear eosinophil and allergic mucin were the most consistent findings with the frequency of 58 (96.7%) and 54 (90%) respectively. Fungal hyphae were present in only 8 (13.3%) patients and Charcot-Leyden crystals were present in only 6 (10.0%) patients. Of 60 patients, 46 patients (20 patients from Group A and 26 patients from Group B) were positive for KOH mount. A total of 42 (91.4%) had Aspergillus flavus grown on culture [Table/Fig-2]. Aspergillus niger was present in only 2 (4.3%) patient. Schizophyllus commune was seen in 2 (4.3%) of the patient. All samples sent for histopathological evaluation were found to be consistent with nasal polyp with inflammation and PAS stain for fungal pathology was positive in 8 (13.3%) cases. The mean SNOT score in Group A was 52.5 in the preoperative period and was achieved to 35.4 at the end of one month and at the end of six months, it was decreased to 34.3. Again in Group B, the mean SNOT score was 55.7 in the preoperative period and at the end of one month it was 38.3 and at the end of 6 month it was found to be 29.5. Almost, 35% (10) of the patients in Group A and 42% (12) in Group B had cases of group were clinically asymptomatic at the end of six months and there was no significant difference noted (p=0.536).
H&E section showing pauci septate hyphae suggestive of Aspergillus flavus (400x).
Considering the Kupferberg endoscopic grading all 60 patients was endoscopic grade 4 preoperatively. In Group A, endoscopic Grade 0 was achieved in 7 (23.33%) patents at the end of one month and remained unchanged at third follow up. Similarly, in Group B, 8 (26.66%) of patients presented with endoscopic Grade 0 at the end of six months (p=0.686). No statistical co-relation was found between KOH mount and serum total IgE or between KOH and AEC (p>0.05). Nine (32.14%) patients in Group A and 7 (25.92%) patients in Group B had recurrence of nasal polyps at the end of six months (p=0.707) as shown in the [Table/Fig-3].
Comparison of AEC, IgE, SNOT and recurrence of disease between Group A and Group B, treated with steroid and itraconazole respectively in the postoperative period.
Discussion
Management of AFRS is often considered a challenge to the rhinologist in spite of its specific clinical, radiological and histopathological findings. Although Bent-Kuhn’s criteria [2] is considered as the gold standard for clinical diagnosis for AFRS, yet it is difficult to produce it in routine clinical practice as majority of patients who exhibit classical features like presence of allergic mucin, IgE mediated hypersensitivity and eosinophilia fail to show positive fungal cultures [3,4]. Also neither positive fungal culture confirms the diagnosis of allergic fungal sinusitis nor a negative culture rule out the disease as fungi can grow as saprophyte in a diseased sinus. Again there are variety of the mycology laboratories which differ in tissue handling which influence the positive fungal culture [5]. Similarly, treatment of AFRS is divergent as different treatment protocols have been adopted in the past decade to overcome most frequently encountered complication i.e., recurrence of disease. Steroids (systemic/topical) have been claimed to increase the cure rates of AFRS by decreasing the recurrence rate with reduction in mucosal stage of disease and systemic IgE levels [6,7]. In spite of the encouraging postoperative results, a significant proportion of the patients usually present with recurrence of disease even in the early postoperative period as described by Marple BF et al., which was ranged from 10% to nearly 100% [8]. Shubert NS and Goetz DW also reported the long term clinical outcome of 67 patients following initial surgical therapy for AFRS [9].
But prolonged course with high dose of systemic steroid needed for the treatment of AFRS is not always feasible because of its unavoidable systemic toxicity and some patients also do not respond to the standard treatment. Keeping in mind the aetiological factor, antifungal treatment (itraconazole) have been tried in patients with AFRS aimed at better control of the disease by declining the recurrence rate of AFRS. Itrconazole by inhibiting enzyme lanosterol 14-alpha-demethylase decreases the synthesis of ergosterol and later considered as vital component of the fungal cell membrane hence reduces the fungal load in the postoperative period and itraconazole has the best activity against Aspergillus and black moulds that typically causes fungal sinusitis. Again antifungals cannot be prescribed for prolonged period of time because of the derangement of hepatic enzymes usually seen in higher therapeutic doses [9] for the treatment of AFRS. In the present study we have limited the dose if itraconazole (100 mg BID) expecting for lesser side effects and only 2 (6.6%) patients presented with deranged hepatic enzymes at the end of three month of treatment.
In the current study, patients treated with steroid and itraconazole had significant improvement in the symptoms and endoscopic grading at the end of six months. Patients of both the groups had significant reduction of SNOT scores at the end of six months. Although the difference between them was found to be insignificant (p=0.143) still symptomatic control of disease in the itraconazole group was better than that of the steroid group. Again it has been noted that there was significant improvement of the mean SNOT score noticed in both the groups at the end of one month and at the subsequent follow up the score almost remain unchanged. Improvement in the Kupferberg endoscopic grading was almost parallel in patients of both the groups and no significant difference in the endoscopic grade was noticed between them (p= 0.750).
Similarly, declining in the IgE level was found in both the groups and there was no direct correlation between the Kupferberg endoscopic grading and the serum IgE level. Denning DW et al., reported that the patients with allergic fungal sinusitis treated with oral itraconazole 200 mg twice daily demonstrated decrease in total IgE and oral steroid requirements [10]. Chan KO et al., also demonstrated the efficacy of itraconazole in refractory AFRS found significant clinical improvement in 28% of cases [11]. Itraconazole can not only decrease the fungal colonization but also can be considered as steroid sparing agent with decreasing the inflammation and polyposis [12].
Limitation
Although itraconazole can be a better treatment option for symptomatic control and endoscopic clearance of AFRS, large study population with long term follows up may be required for a better result.
Conclusion
Itraconazole can be considered as an effective treatment alternative to the steroid for postoperative management of AFRS. Although there was no significant difference noted between two groups, patients treated with itraconazole had a better symptomatic relief and endoscopic clearance of disease. A large study population with a long term follow up may be required for a better outcome.