Emphysematous Pyelonephritis with Human Immunodeficiency Virus Infection
Kamal V. Kanodia1, Aruna V. Vanikar2, Shruti P. Gandhi3, Pranjal R. Modi4, Hargovind L. Trivedi5
1 Professor, Department of Pathology, Laboratory Medicine, Transfusion Services and Immunohematology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases and Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Asarwa, Ahmedabad, India.
2 Professor and Head, Department of Pathology, Laboratory Medicine, Transfusion Services and Immunohematology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases and Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Asarwa, Ahmedabad, India.
3 Associate Professor, Department of Radiology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases and Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Asarwa, Ahmedabad, India.
4 Professor, Department of Urology and Transplantation, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases and Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Asarwa, Ahmedabad, India.
5 Professor, Department of Nephrology and Transplantation Medicine and Director, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases and Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Asarwa, Ahmedabad, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kamal V. Kanodia, Professor, Department of Pathology, Lab Medicine, Transfusion Services and Immunohematology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases and Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Asarwa, Ahmedabad, India.
E-mail: kamalkanodia@yahoo.com
Diabetes mellitus, Kidney, Western blot
A 42-year-old female, known case of type 2 diabetic on oral hypoglycemic treatment for last two years, presented in emergency with acute left flank pain of four days duration. She had a history of low-grade fever for five days. On examination, her blood pressure was 130/90 mmHg and pulse rate was 100/minute with tenderness in her left flank region. On investigation, her Haemoglobin (Hb) was 9.1 gm/dl; Total Leukocyte Count (TLC), 18.6×103/μl with 87% neutrophils; platelet count, 2.36×105/μl, random blood sugar 545 mg/dl; serum acetone was absent, serum creatinine, 1.86 mg/dl and serum potassium 3.6 mEq/l. She was reactive for HIV-1 by ELISA and Western blot. A routine urine examination by dipstick showed trace albumin; microscopic examination revealed 40-42 pus cells/high power field and no organism was isolated on culture. Her blood culture was negative. Ultrasonography of abdomen showed features of Left Kidney (LK) Emphysematous Pyelonephritis (EPN). Computed Tomography (CT) [Table/Fig-1] showed an enlarged and oedematous left kidney with multiple pockets of air in the pelvicalyceal system, renal parenchyma, perinephric region and ureter, suggestive of EPN Class 3A. She was treated with intravenous antibiotics, insulin and Percutaneous Nephrostomy (PCN). However, PCN did not relieve her symptoms and an emergency nephrectomy of her LK was carried out on the next day. The specimen was sent for histopathological examination.
Multiple air collections in renal parenchyma and perinephric region suggestive of emphysematous pyelonephritis (computed tomography).

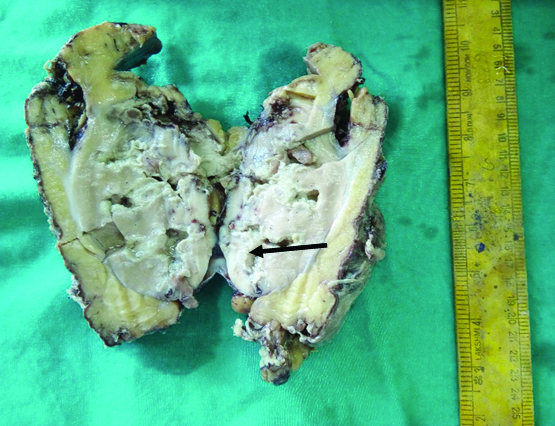
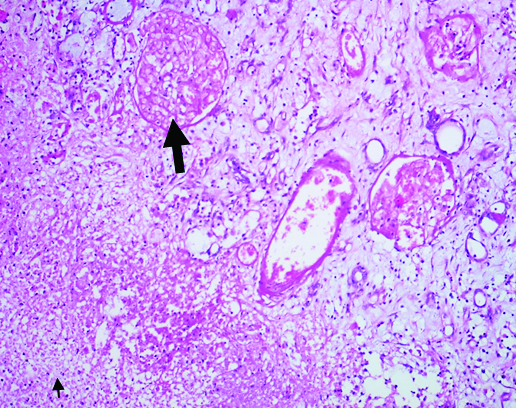
On gross examination left kidney weighed 480 gram and measured 14×9×7 cm3. Outer surface showed large areas of haemorrhage and necrosis. Cut surface showed patchy areas of haemorrhage and necrosis in the cortex and medulla [Table/Fig-2]. Microscopy showed extensive corticomedullary necrosis, focal haemorrhage and overlying marked infiltration with neutrophils, cell debris, few foamy macrophages and lymphocytes in the parenchyma [Table/Fig-3]. There were very few viable glomeruli that showed mild mesangial prominence with fairly open capillary lumina lined by membranes of normal thickness. Bowman capsules were unremarkable. Tubules revealed mild degenerative changes. Interstitium was mildly prominent for focal oedema and leucocytic infiltration. Blood vessels were unremarkable. She was discharged two weeks after surgery. On follow up of three months she had no complaints and is on anti-retroviral therapy.
Gross specimen of left kidney shows patchy areas of hemorrhage and necrosis in the cortex and medulla.
Cortical necrosis (↑) focal hemorrhage and overlying marked infiltration with neutrophils, cell debris and lymphocytes (↑) (H&E, x100).
EPN is a necrotizing parenchymal and perirenal infection commonly due to Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Pseudomonas, Enterobacter, and rarely due to yeasts [1,2]. EPN has been reported in renal transplant recipients and in patients with polycystic kidney disease [3-5]. However, it has been rarely reported in coexisting HIV infections [2,6]. The pathophysiology of EPN remains unclear, however, some factors that are implicated in development of the disease proposed are high tissue glucose concentration, presence of bacteria capable of fermenting glucose (hence the gas production), decreased tissue perfusion alterations in host defense mechanisms and in case of non-diabetic patients, urinary tract obstruction [7].
The analysis of gas formed in EPN revealed nitrogen (60%), hydrogen (15%), carbon dioxide (5%), and oxygen (8%) [1,2,7]. The mechanism of gas formation is still unclear, however it has been suggested that mixed acid fermentation or rapid tissue catabolism and impaired transport of the end products at the inflammatory site contributes to gas formation [7].
The mortality of EPN is 20% to 30% and in the absence of prompt diagnosis and an early start of treatment, the disease carries a mortality rate of up to 78% [7]. The differential diagnosis usually depends on the location of the gas. If the gas is limited to the collecting system the aetiology is usually infective, recent instrumentation or fistula to the bowel [8]. Our patient had poor prognosticators including CT class 3A, diabetes and HIV, yet recovered completely due to early intervention and prompt management.
Authors’ Contributions
KV analyzed the patient data and was a major contributor in writing the manuscript. AV and KV performed the histological examination of the patient’s kidney and edited the manuscript. SG performed the radiological examination. PM did surgical management. All authors read and approved the final manuscript.
[1]. Huang JJ, Tseng CC, Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesisArch Intern Med 2000 160:797-805. [Google Scholar]
[2]. Perez CE, Botero-Garcia CA, Sanchez FM, Emphysematous pyelonephritis in patients infected with human immunodeficiency virus: case reportInfect 2016 20(2):101-06. [Google Scholar]
[3]. Ortiz A, Petkov V, Urbano J, Contreras J, Alexandru S, Garcia-Pérez A, Emphysematous pyelonephritis in dialysis patient after embolization of failed allograftUrology 2007 70:372.e17-19. [Google Scholar]
[4]. Arai S, Makino T, Okugi H, Hasumi M, Shibata Y, Hatori M, A case of emphysematous pyelonephritis in a renal allograftTransplantation 2006 81:296-97. [Google Scholar]
[5]. Tseng CC, Wu JJ, Wang MC, Hor LI, Ko YH, Huang JJ, Host and bacterial virulence factors predisposing to emphysematous pyelonephritisAm J Kidney Dis 2005 46:432-39. [Google Scholar]
[6]. Mohamed Ashif PA, Sandeep P, Sasidharan PK, Emphysematous pyelonephritis in a patient infected with the human immunodeficiency virusSaudi J Kidney Dis Transpl 2012 23:1046-50. [Google Scholar]
[7]. Salati SA, Emphysematous pyelonephritis: a case reportJ Pioneer Med Sci 2014 4(4):174-76. [Google Scholar]
[8]. Huang JJ, Chen KW, Ruaan MK, Mixed acid fermentation of glucose as a mechanism of emphysematous urinary tract infectionJ Urol 1991 146(1):148-51. [Google Scholar]