Temporary Blindness after Inferior Alveolar Nerve Block
Animesh Barodiya1, Rishi Thukral2, Shaila Mahendra Agrawal3, Anshul Rai4, Siddharth Singh5
1 Senior Resident, Department of Dentistry, All India Institute of Medical Sciences, Bhopal, Madhya Pradesh, India.
2 Senior Resident, Department of Dentistry, All India Institute of Medical Sciences, Bhopal, Madhya Pradesh, India.
3 Professor, Department of Oral and Maxillofacial Surgery, Modern Dental College and Research Institute, Indore, Madhya Pradesh, India.
4 Assistant Professor, Department of Dentistry, All India Institute of Medical Sciences, Bhopal, Madhya Pradesh, India.
5 Senior Lecturer, Department of Oral and Maxillofacial Surgery, Hitkarini Dental College, Jabalpur, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Animesh Barodiya, G-108, Chinar Dream City, Hoshangabad Road, Bhopal-462026, Madhya Pradesh, India.
E-mail: anim4391@gmail.com
Inferior Alveolar Nerve Block (IANB) anaesthesia is one of the common procedures in dental clinic. This procedure is safe, but complications may still occur. Ocular complications such as diplopia, loss of vision, or ophthalmoplegia are extremely rare. This case report explains an event where due to individual anatomic variation of the sympathetic vasoconstrictor nerve and maxillary and middle meningeal arteries, intravascular administration of anaesthetic agent caused unusual ocular signs and symptoms such as temporary blindness.
Anaesthetics, Anatomic variation, Ocular complications
Case Report
A 30-year-old patient came to the Department of Dentistry, All India Institute of Medical Sciences, Bhopal, India, with chief complaint of pain and swelling in right lower back tooth region. Patient was diagnosed as having pericoronitis with relation to right lower third molar. Extraction of same tooth was planned under local anaesthesia.
Before administrating anaesthetic agent, patient’s vital signs were assessed and they were within normal limits. There was no history of any systemic illness. Local anaesthesia sensitivity testing was done by injecting 0.1 ml of local anaesthetic solution subcutaneously in forearm, which was negative.
IANB anaesthesia of right side was given to the patient using a long (30 mm) 27-gauge needle. Aspiration was negative. Within one minute of injecting 1.8 ml of 2% lidocaine with adrenaline (2% Lignox, Indoco Pharmaceuticals), the patient complained of discomfort on the same side of the face. He reported blurring of vision with right eye followed by complete vision loss. A physical examination showed no changes in the vital signs and patient was conscious.
An ocular motility test was performed by instructing the patient to move his eye in all the directions indicated normal eye movement of both the eyes. Patient was asked to read nearby charts with both the eyes separately on which, it was found that there was normal vision of left eye and no vision on affected side. Movement of the facial muscles was normal, indicated that the facial nerve function was intact, and there was no blanching or burning sensation of oral mucosa at the site.
Thus, we diagnosed the condition as temporary blindness during IANB anaesthesia. The patient was informed of this condition and monitored. All the symptoms disappeared within 30 minutes after the initial symptom.
Discussion
One of the most common procedures in dentistry is the administration of local anaesthetic agent. Local anaesthetic agents administered carefully taking care of anatomic landmarks, and within recommended limits, have been considered to be safe.
Even after taking all the precautions and taking care of anatomic landmarks side effects and complications of IANB anaesthesia may occur. They include allergic reaction, vasoconstriction, interactions with other medications, haematoma, pain during injection, burning sensation, paresthesia, trismus, infection, oedema, momentary tissue blanching and facial nerve paralysis [1].
Some side effects occur less commonly and thus are difficult to explain. In rare cases the symptoms can be related to ocular function, such as temporary or permanent blindness, diplopia, ophthalmoplegia, myosis, ptosis [2–5]. Diplopia being the most common among them [6]. The relationship between maxillary artery and the branches of the mandibular nerve is highly variable [7]. In 1972, Rood JP had described the arterial route of the local anaesthetic agent to the eye after IANB [8].
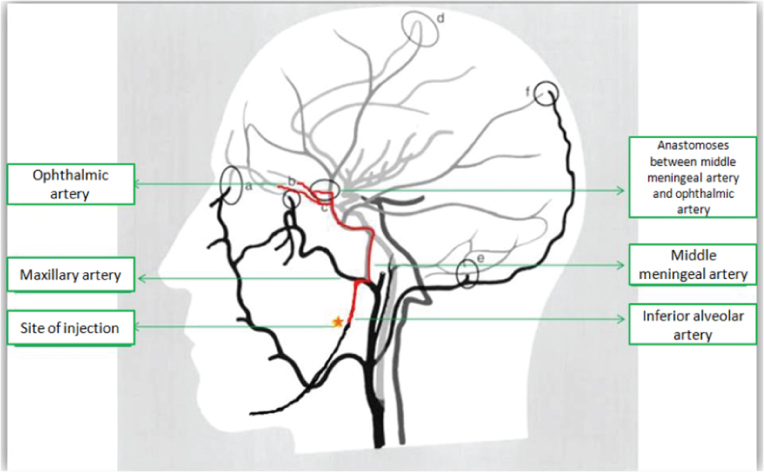
During IANB although initial aspiration may be negative, minor movement of the patient or the needle during administration may result in intravascular injection [9]. As the anaesthetic agent is administered under pressure intravascularly, the solution is forced back up the inferior alveolar artery allowing flow to the middle meningeal artery. The middle meningeal artery is branch of the first part of maxillary artery it runs upwards deep to the lateral pterygoid muscle and while entering into skull through foramen spinosum, it gives off many orbital branches [10]. These orbital branches pass through the superior orbital fissure or through separate canals in the great wing of the sphenoid, to anastomose with the lacrimal, retinal or other branches of the opthalmic artery [Table/Fig-1]. The central retinal artery of the retina is a small branch of opthalmic artery. The anaesthetic solution passing from the middle meningeal artery to the opthalmic artery may then reach the eye through the central retinal artery, causing loss of vision and loss of the papillary light reflex.
Point C shows anastomoses between middle meningeal artery and the ophthalmic artery.
The diagnosis is made only when the vision and eye movement returns to normal, shortly after local anaesthetic administration. Tomazzoli-Gerosa L et al., suggested that ocular complications are mostly temporary, lasting from minutes to hours. As in this case patient vision returned to normal after some time [11]. Permanent complications, such as severe visual acuity and blindness are uncommon.
In this case, we did not report a wrong technique during injection; anatomic variation can be taken into consideration as one of the possible causes of these complications.
Van der Bijl P and Meyer D suggested the following management guidelines [12]:
Reassure patients that these complications are usually transient in nature;
The affected eye should be covered with gauze dressing to protect the cornea for the duration of anaesthesia;
Functional monocular vision will be restored by covering the affected eye; The patient should be escorted home by a responsible adult, since monocular vision is devoid of distance-judging capability;
If the ocular complications last longer than six hours, patients should be referred to an ophthamologist for evaluation.
Conclusion
This case report explains a case of unilateral temporary blindness after IANB. This adverse effect may develop from intravascular injection of anaesthetic agent into inferior alveolar artery and backflow of anaesthetic agent into internal maxillary artery and ophthalmic artery. Thorough knowledge of pterygomandibular space anatomy and careful aspiration before injecting can avoid such type of complications.
[1]. Scott J, Moxham B, Downie I, Upper lip blanching and diplopia associated with local anaesthesia of the inferior alveolar nerveBDJ 2007 202(1):32-33. [Google Scholar]
[2]. Wilkie G, Temporary uniocular blindness and ophthalmoplegia associated with a mandibular block injection. A case reportAustralian Dental Journal 2000 45(2):131-33. [Google Scholar]
[3]. Clarke JR, Clarke DJ, Hysterical blindness during dental anaesthesiaBr Dent J 1987 162:267-68. [Google Scholar]
[4]. Blaxter PL, Britten MJA, Transient amaurosis after mandibular blockBr Med J 1967 1:681-84. [Google Scholar]
[5]. Rishiraj B, Epstein JB, Fine D, Nabi S, Wade NK, Permanent vision loss in one eye following administration of local anaesthesia for a dental extractionInt J Oral Maxillofac Surg 2005 34:220-23. [Google Scholar]
[6]. Aguado-Gil J-M, Barona-Dorado C, Lillo-Rodríguez J-C, De la Fuente-González D-S, Martínez-González J-M, Occular complications following dental local anaesthesiaMed Oral Patol Oral Cir Bucal 2011 16(5):e688-93. [Google Scholar]
[7]. Pretterklieber ML, Skopakoff C, Mayr R, The human maxillary artery reinvestigatedActa Anat 1991 142:281-87. [Google Scholar]
[8]. Rood JP, Ocular complication of inferior dental nerve block. A case reportBr Dent J 1972 132:23-24. [Google Scholar]
[9]. Lee CK, Ocular complication after inferior alveolar nerve blockDental bulletin 2006 11(8) [Google Scholar]
[10]. Warwick R, Williams PL, Gray’s Anatomy 1978 35th ednLondonLongman:629-36.:997-1010. [Google Scholar]
[11]. Tomazzoli-Gerosa L, Marchini G, Monaco A, Amaurosis and atrophy of the optic nerve: An unusual complication of mandibular nerve anaesthesiaAnn Ophthalmol 1988 20:170-1. [Google Scholar]
[12]. Van der Bijl P, Meyer D, Ocular complications of dental local anaesthesiaSadj 1998 53(5):235-38. [Google Scholar]