Preventive Training among Medical Interns in Mexico City and Its Association with Needlestick and Sharp Injuries – A Cross Sectional Study
Victor Hugo Garcia1, Katja Radon2
1 Alumnus, Master of International Occupational Safety and Health Program, Ludwig-Maximilians-Universität, Munich, Germany.
2 Professor, Center for International Health, Institute for Occupational, Social and Environmental Medicine, University Hospital Munich (LMU).
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Victor Hugo Garcia, Almacenes 114 Chiapas G-126, Tlatelolco, Mexico City, Mexico.
E-mail: drgarciachavez@comunidad.unam.mx
Introduction
Medical students are a vulnerable group for the acquisition of blood borne pathogens due to their lack of experience. In Europe and Asia preventive training programs have reduced accidental exposures.
Aim
The aim of the study was to compare the lifetime prevalence of Needlestick and Sharp Objects Injuries (NSIs) among medical interns who received preventive training versus those without such training in Mexico City.
Materials and Methods
In 2013, a cross-sectional study was performed applying an anonymous self-administrated questionnaire. The study population included 467 medical students, male and female, at the end of their internship. The lifetime prevalence of NSI was estimated and compared between students who had received preventive training and those who did not.
Results
The overall lifetime prevalence of NSI was 58%. Lifetime prevalence was higher in students without preventive training compared to those who had such a training (68% vs 51%; p value= 0.002). NSI Lifetime prevalence was not associated with sex, age or place of birth. The task most commonly associated with the latest NSI in trained and untrained students was withdrawing blood.
Conclusion
NSI are frequent accidents among medical students in Mexico City, especially during blood taking. Training units on how to prevent NSI should be encouraged in Mexican medical colleges.
Healthcare personel, Medical students
Introduction
Biological hazards are an important occupational health problem in healthcare workers. This includes infections like e.g., HIV/AIDS, hepatitis A to C, flu, and typical childhood infections (measles, rubella, etc.,). Some of them are blood-borne diseases and the risk of acquiring them increases substantially if the healthcare worker suffers Needlestick or Sharp Injury (NSI). Medical students are a particular group of healthcare workers. They need special attention due to their lack of experience and due to the fact that they are in many countries not covered by the occupational accident insurance [1–7].
Blood accidental exposure in medical students has been investigated in many countries. The most common exposure is percutaneous exposure by needlestick injuries [1–7]. The lifetime prevalence of NSI at the end of training has been estimated to be almost 60% in Germany, USA and Palestine [4,6,8]. Also, high under reporting has been pointed out in these studies.
The activities and risk factors associated with NSI are less frequently studied. Different authors used different questionnaire instruments. Therefore, task and risk factors considered are not directly comparable. Among tasks, suturing and venipuncture are commonly reported as being more frequently associated with NSI [6–9]. Lack of experience and lack of awareness are personal characteristics consistently found to be related to NSI [10,11].
Training programs about NSI prevention among health care workers have shown benefits in reducing the frequency of these accidents and in increasing the appropriate report and following post exposure [12–14].
Reliable data of occupational injuries among medical students from Mexico is not available. The aim of this study was to compare the lifetime prevalence of needlestick and sharp object injuries among medical students by training status at the end of their internship in Mexico City.
Materials and Methods
In 2013 we conducted a cross-sectional study using a self-administered questionnaire in Spanish answered by medical students from one college in Mexico City. The questionnaire consisted of six parts: demographic information (5 items), work related conditions (3 items), health conditions (19 items), NSI (6 items), risk perception (10 items) and use of universal precautions including training related to prevention (11 items). Questions were formulated based on pre-existent questionnaires and literature (10-11). The questions were back-translated to English to correct interpretation bias. We conducted a pre-test in Spanish with 20 healthcare workers to check the comprehension of the questions and answers. For the current paper we present the analysis of NSI life-time prevalence comparing students who received training on measures to prevent NSI to those who did not receive such training.
The survey was performed after the final exam of the study program, just at the end of the internship to avoid recall bias. Of the 695 medical students 473 (68%) answered the questionnaire. Of them, six students had to be excluded from the final analyses as they did not report whether they had received training on preventive measures or not.
For this research needlestick and sharp object injury was defined as a wound, laceration or puncture made with a needle, surgical material or other sharp object related to medical practice. In addition, number of NSI was assessed (1, 2, or more than 2 NSI).
The study program of this medical college does not include a mandatory program for prevention of NSI. Professors were free to include it in their lessons, usually before the beginning of the hospital practices. Training status of the students was based on self-reports.
The declaration of Helsinki was closely followed. Approval for this study was obtained from Ethics Research Committee at Mexico. The students received verbal information about the research and verbal instructions to answer the written questionnaire. Informed consent to participate was given through checking the informed consent box on the anonymous questionnaire. Students dropped the completed questionnaires in a box to ensure anonymity of the response.
Statistical Analysis
After double data entry process error check was performed. Data were analysed using EPI Info™ 7.1.3 software. Nominal and ordinal data were presented as absolute and relative frequencies. Independence in the life-time prevalence of NSI (did or did not suffer NSI) between students who had received preventive training and those who did not was assessed using Chi-square tests. Odds ratios with 95% Confidence Intervals (CI) were calculated by unadjusted logistic regression for NSI by training status. Sex, age and place of birth were discarded as potential confounders after analysing their independence with NSI prevalence and training status by Chi-square tests.
Results
Seventeen of the 467 questionnaires were partially filled. They were managed as missing data in the descriptive analysis [Table/Fig-1,2 and 3] and excluded for the logistic regression [Table/Fig-4]. A total of 282 (60.4%) of the participants were female. The mean age of the students was 23.9 years (SD=1.3 years). Almost 91.9% students were born in the metropolitan area of Mexico city and just three students were foreigners (data not shown). About 57% of the students had received theoretical and practical training in NSI prevention and were assigned to the trained group. Training status was statistically independent of age, sex and place of birth [Table/Fig-1].
Demographic characteristics by needlestick injury prevention training status.
| Missingdata | UntrainedN= 198n (%) | Missingdata | TrainedN= 269n (%) | p-valueChi squaretest |
|---|
| Sex |
| Male | 0 | 74 (37.4%) | 0 | 111 (41.3%) | 0.40 |
| Female | 124 (62.6%) | 158 (58.7%) |
| Age (years) |
| 20-23 | 6 | 84 (43.8%) | 4 | 105 (39.6%) | 0.30 |
| 24-25 | 90 (46.9%) | 142 (53.6%) |
| 26-34 | 18 (9.4%) | 18 (6.8%) |
| Place of birth |
| Metropolitanarea of Mexicocity | 6 | 178 (92.7%) | 5 | 241 (91.3%) | 0.33 |
| Outsidemetropolitanarea | 14 (7.3%) | 23 (8.7%) |
Lifetime prevalence of needlestick injury (NSI) by demographic characteristics.
| Missing data | NSI lifetimeprevalenceN= 272n (%) | p-valueChi-squaretest |
|---|
| Sex |
| Male | 0 | 100 (54.4%) | 0.15 |
| Female | 172 (63.2%) |
| Age (years) |
| 20-23.9 | 6 | 112 (60.0%) | 0.56 |
| 24-25.9 | 136 (58.6%) |
| 26-34 | 18 (50.0%) |
| Place of birth |
| Metropolitan area of Mexico City | 6 | 249 (59.6%) | 0.07 |
| Outside metropolitan area | 18 (50.0%) |
Relative and absolute frequencies of the tasks done at the moment of the latest needlestick injury by training status.
| Missing data | Untrained | Missing data | Trained | p-valueChi-squaretext |
|---|
| N= 135 | N= 137 |
|---|
| n (%) | n (%) |
|---|
| Clean/collectmaterials | 0 | 6 (4.4%) | 1 | 18 (13.2%) | 0.04 |
| Suture | 19 (14.0%) | 25 (18.4%) |
| Recappingthe needle | 27 (20.0%) | 22 (16.1%) |
| Venipuncture/blood sampling | 62 (46.0%) | 61 (44.9%) |
| Delivery the needlefrom personto person | 9 (6.7%) | 6 (4.4%) |
| Other task | 12 (8.9%) | 4 (3.0%) |
Results of the unadjusted logistic regression model for needlestick prevalence with training status and potential confounders.
| OR | 95% | CI |
|---|
| Training status |
| Untrained/Trained | 2.1 | 1.4 | 3.2 |
| Sex |
| Female/ Male | 1.3 | 0.9 | 1.9 |
| Age (years) |
| 24-25/ 20-23 | 1.0 | 0.7 | 1.5 |
| 26-34/ 20-23 | 0.7 | 0.3 | 1.4 |
| Place of birth |
| Outside/Metropolitanarea of Mexico City | 0.6 | 0.3 | 1.2 |
OR- Odds Ratio; CI- Confidence Interval
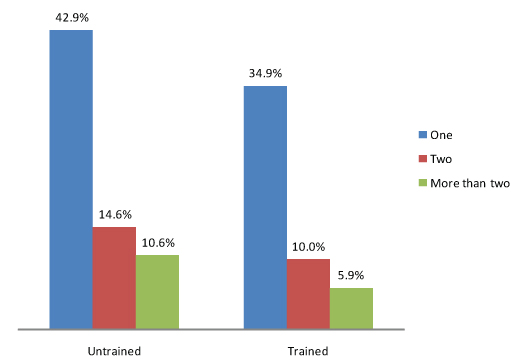
The overall lifetime prevalence of NSI was 58.2%. It was not statistically associated with age, sex or place of birth [Table/Fig-2] but was higher in the group who did not receive training (68% vs 51% p Chi-square= 0.002) [Table/Fig-5].
Number of Needlestick Injuries (NSI) by training status.
p-value of Chi-square test=0.002.
In the logistic regression model, excluding those with missing data for sex, age, place of birth or NSI prevalence, untrained students were twice as likely to have suffered NSI than the trained group (OR 2.1 95% CI 1.4-3.2) [Table/Fig-4]. In addition, female students were slightly more likely to report NSI (1.3; 0.9-1.9). Odds ratio for NSI lifetime prevalence and training status adjusted for sex was 2.1 (95% CI 1.4-3.1), equal to the crude odds ratio.
The most common task done at the moment of the latest NSI in trained and untrained students was venipuncture and blood sampling. Distribution of the task related to the latest NSI was different among trained and untrained students [Table/Fig-3].
Discussion
In this study, we found a high lifetime prevalence of NSI in Mexican medical students at the end of their internship (58.2%). This was not statistically significantly related to sex, age or place of birth. Untrained students were at higher risk to report NSI than those who received training about NSI prevention (OR 2.1 95% CI 1.4-3.2).
Among the strengths of the study was that we could invite all medical interns of the main medical school of Mexico city to participate in the study. The response was relatively high, reducing the likelihood of selection bias. To the best of the authors’ knowledge, the sample size of this study was higher than in previous studies allowing a statistical power of 98%. Potential confounders (age, sex and place of birth) were addressed and assessed with Chi-square independence test so that a good internal validity can be assumed. The questionnaire was face validated and a pilot test indicated a high face and content validity of the instrument. Preventive training is usually given before the students start hospital practices so that reporting bias is unlikely.
The overall lifetime prevalence found in this study was similar to those found in medical interns in Palestine (58%) [6], recent graduates in the USA (59%) [4] and among medical students in the last year of medical training in Germany (59%) [8]. Other studies in Europe found considerably lower lifetime prevalence in medical students in their fifth year of training (Germany 36%) [5] and in their last year of training (Austria 44%, Germany 41% and UK 16%) [10]. Overall, NSI prevention seems to be more effective in Europe than in the Americas and Palestine. These data indicate that NSI still are a relevant problem in medical students. Therefore, primary prevention is of uppermost importance. One option is the use of safety needles in the healthcare setting. This equipment is still not available in many Mexican hospitals. In addition, the evidence that these devices prevent NSI is so far limited [15].
The higher risk found in untrained students was consistent with the experiences in reduction of NSI after preventive training of medical students in Singapore [13] and nursing students in Taiwan [16]. This highlights the importance of training in the NSI prevention as other researchers had pointed out [17] since it still represents the main way of blood and body fluid exposure among trainees [18].
Independent of training status, the tasks most commonly performed at the moment of the NSI was blood sampling, this is consistent with other studies from Germany [5,8] and Sri Lanka [7] where the main activities at the time of the NSI were blood withdrawing and suturing. Reason for that might be that these tasks are typical procedures done by the medical students. Therefore, preventive training units should focus on these procedures and on how to prevent NSI in these situations.
Limitation
Recall bias and differential reporting between trained and untrained students cannot be completely rule out. Due to the cross-sectional study we have to consider that some of the NSIs in the trained group might have happened before the training session about NSI prevention.
Conclusion
NSI are frequent accidents among medical students in Mexico city, especially during blood taking. Untrained students are in higher risk of suffering NSI than those having received a training unit on how to prevent NSI. Models of preventive training applied in Europe and Asia should be replicated to reduce NSI lifetime prevalence in next generations. In addition, the use of safety devices should be encouraged in Mexican hospitals.
OR- Odds Ratio; CI- Confidence Interval
[1]. Rabbitts JA, Occupational exposure to blood in medical studentsS Afr Med J 2003 93(8):621-4. [Google Scholar]
[2]. Kobets AJ, Perlotto J, Angoff NR, An intervention with third-year medical students to encourage the reporting and management of occupational exposuresAcad Med 2012 87(9):1199-204. [Google Scholar]
[3]. Kwee SA, Ka’anehe L, Occupational exposures and knowledge of universal precautions among medical studentsHawaii Med J 1999 58(2):21-23. [Google Scholar]
[4]. Sharma GK, Gilson MM, Nathan H, MA M, Needlestick injuries among medical students: incidence and implicationsAcad Med 2009 84(12):1815-21. [Google Scholar]
[5]. Deisenhammer S, Radon K, Nowak D, Reichert J, Needlestick injuries during medical trainingJ Hosp Infect 2006 63(3):263-67. [Google Scholar]
[6]. Al-Dabbas M, Abu-Rmeileh NM, Needlestick injury among interns and medical students in the occupied Palestinian territoryEast Mediterr Health J 2012 18(7):700-06. [Google Scholar]
[7]. Liyanage IK, Caldera T, Rwma R, Liyange CK, De Silva P, Karunathilake IM, Sharps injuries amongmedical students in the Faculty of Medicine, Colombo, Sri LankaInt J Occup Med Environ Health 2012 25(3):275-80. [Google Scholar]
[8]. Wicker S, Nürnberger F, Schulze JB, Rabenau HF, Needlestick injuries among German medical students: time to take a different approach?Med Educ 2008 42(7):742-45. [Google Scholar]
[9]. Moon CS, Hwang JH, Lee CS, Park KH, Kim ES, Exposure to blood and body fluid among medical students in KoreaAm J Infect Control 2010 38(7):582-83. [Google Scholar]
[10]. Salzer HJ, Hoenigl M, Kessler HH, Stigler FL, Raggam RB, Rippel KE, Lack of risk-awareness and reporting behavior towards HIV infection through needlestick injury among European medical studentsInt J Hyg Environ Health 2011 214(5):407-10. [Google Scholar]
[11]. Saleem T, Khalid U, Ishaque S, Zafar A, Knowledge, attitudes and practices of medical students regarding needlestick injuriesJ Pak Med Assoc 2010 60(2):151-56. [Google Scholar]
[12]. Zafar A, Habib F, Hadwani R, Ejaz M, Khowaja K, Khowaja R, Impact of infection control activities on the rate of needlestick injuries at a tertiary care hospital of Pakistan over a period of six years: An observational studyBMC Infect Dis 2009 9:78 [Google Scholar]
[13]. Seng M, Lim JW, Sng J, Kong WY, Koh D, Incidence of needlestick injuries among medical students after implementation of preventive trainingSingapore Med J 2013 54(9):496-500. [Google Scholar]
[14]. Mehrdad R, Meshki M, Pouryagub G, Effects of training course on occupational exposure to bloodborne pathogens: a controlled interventional studyInt J Prev Med 2013 4(11):1236-42. [Google Scholar]
[15]. Lavoie MC, Verbeek JH, Pahwa M, Devices for preventing percutaneous exposure injuries caused by needles in healthcare personnelCochrane Database Syst Rev 2014 9(3):CD009740 [Google Scholar]
[16]. Yang YH, Liou SH, Chen CJ, Yang CY, Wang CL, Chen CY, The effectiveness of a training program on reducing needlestick injuries/sharp object injuries among soon graduate vocational nursing school students in southern TaiwanJ Occup Health 2007 49:424-29. [Google Scholar]
[17]. Bhattarai S, Smiriti KC, Pradhan PMS, Lama S, Rijal S, Hepatitis B vaccination status and Needle-stick and Sharps-related Injuries among medical school students in Nepal: a cross-sectional studyBMC Research Notes 2014 7:774 [Google Scholar]
[18]. Hajjaji Darouiche M, Chaabouni T, Jmal Hammami K, Messadi Akrout F, Abdennadher M, Hammami A, Occupational blood exposure among health care personnel and hospital traineesInt J Occup Environ Med 2014 5(1):57-61. [Google Scholar]