Paediatric primary liver tumours are the third largest group of solid abdominal neoplasms in children next to neuroblastoma and Wilms tumour [1]. Childhood liver tumours have received great attention because of their vast histologic variety, uncertainty about pathogenesis and classification and difficulties in treatment [2]. Hepatic tumours account for about 0.5% to 2% of all paediatric neoplasms [3]. A 50 to 60% of primary liver tumours in children are malignant in which hepatoblastoma is most common followed by hepatocellular carcinoma [4]. Undifferentiated embryonal sarcoma of liver is the third most common malignant paediatric liver tumours [5]. In children, benign tumours constitute only 30% of liver tumours and most are epithelioid haemangioendothelioma, followed by mesenchymal hamartoma [6]. The present study was done to study the incidence of paediatric liver tumour in our institute for a period of five years and to study the clinical behaviour, alpha fetoprotein correlation and the histopathological features of paediatric liver tumours and to compare them with other studies.
Materials and Methods
This retrospective study was conducted in Institute of Child Health, Madras Medical College, Chennai, India after getting approval from the institutional ethical committee, wherein the tumour board records and medical records of patients treated for paediatric liver tumours for a period of five years from 2003 to 2008 were retrospectively reviewed, including both resected specimens and biopsies. Details regarding the surgery, clinical features, chemotherapy and follow up were collected. Gross characteristics such as weight of specimen, external surface, tumour size and cut surface were noted retrospectively from the histopathology registers. Sections were taken from the tumour, tumour liver interface and from the adjacent normal parenchyma. The bits were routinely processed, cut and stained with haematoxylin and eosin. The histological features were studied under light microscope. Other details like age, sex, onset, duration, size and site were also noted. Clinicopathological correlation was done.
Results
A total number of 39 cases of paediatric liver tumours were detected during the five years, out of which 20 were resected specimens and 19 were small biopsies. Among these tumours, 32 (82%) were malignant and 7 (18%) were benign. The male to female ratio was 1:1.1. The clinical characteristics are shown in [Table/Fig-1].
Clinical characteristics of paediatric liver tumours.
| Histologic subtype | No of cases | Percentage | M/F | Age (years) |
|---|
| <1 | 1-5 | >5 |
|---|
| Hepatoblastoma | 28 | 71.8 % | 13/15 | 16 | 11 | 1 |
| Epithelioid haemangioendothelioma | 6 | 15.4 % | 1/5 | 3 | 3 | 0 |
| Hepatocellular carcinoma | 2 | 5.1 % | 2/0 | 0 | 0 | 2 |
| Undifferentiated embryonal sarcoma | 2 | 5.1 % | 2/0 | 0 | 0 | 2 |
| Hepatocellular adenoma | 1 | 2.6 % | 1/0 | 0 | 0 | 1 |
| Total | 39 | 100 % | 19/20 | 19 | 14 | 6 |
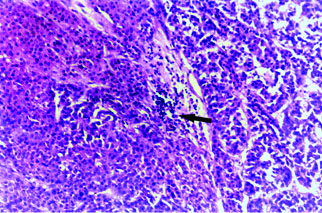
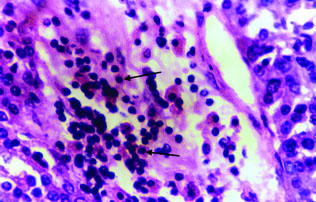
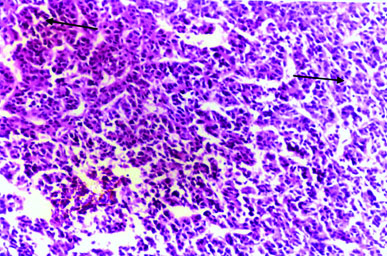
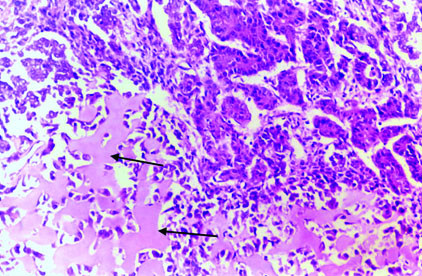
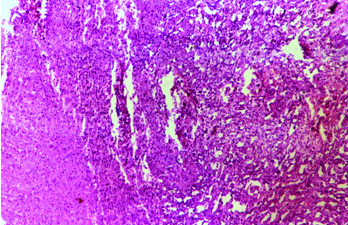
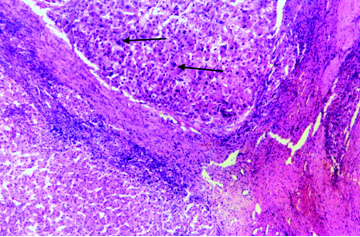
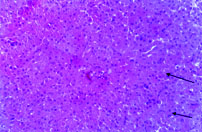
Hepatoblastoma was the most common liver tumour accounting for 28 cases (71.8%). In our study, age range for hepatoblastoma was four months to six years in 28 out of 39 cases of paediatric liver tumour, and accounted for 53.5% with peak incidence between the age group of two months to 24 months. In our study, the average diameter of hepatoblastoma was 8 cm (range: 3-14 cm). The weight of surgically resected specimens ranged from 300 to 1400 grams. Histology of most of these cases (25 cases, 89.4%) was pure epithelial (12 cases of pure fetal type, 12 cases of mixed fetal and embryonal type and one case of macrotrabecular type). The others were mixed epithelial and mesenchymal (three cases). None of our cases was of small cell undifferentiated or anaplastic types. In our study, hepatoblastoma with predominant foetal pattern was most common, in which the neoplastic cells were typically arranged in cords or plates in two to three cell thickness or in a sheet like configuration [Table/Fig-2]. Extramedullary haematopoiesis was noted in fetal area in predominant cases of hepatoblastoma [Table/Fig-3]. An acinar or pseudo glandular pattern was noted in embryonal areas [Table/Fig-4]. Osteoid was noted in all three cases of mixed hepatoblastoma [Table/Fig-5], immature spindle cells noted in one case and calcification in other case, in our study. In epithelioid haemangioendothelioma, the lesion was composed of vascular channels lined by a single continuous layer of plump endothelial cells in a supporting fibrous stroma. The area was well separated from normal liver parenchyma [Table/Fig-6].
Hepatoblastoma. Foetal liver cells with area of extra medullary haematopoiesis (arrow). (H&E, x100).
Hepatoblastoma. Foetal liver cells with area of extra medullary haematopoiesis showing lymphocytes and normoblasts (arrow). (H&E, x400).
Hepatoblastoma. Embryonal liver cells with focal acinar pattern (arrow). (H&E, x100).
Mixed Hepatoblastoma. Foetal epithelial cells and osteoid (arrow). (H&E, x100).
Epithelioid haemangioendothelioma. Normal liver with tumour portion having dilated vascular channels lined by endothelial cells. (H&E, x100).
The second most common primary tumour was epithelioid haemangioendothelioma accounting for six cases (15.4%) with female predominance (male to female ratio of 1:5). We had two cases of hepatocellular carcinoma and two cases of undifferentiated embryonal sarcoma, all of which occurred in males of 5 to 10 years age group.
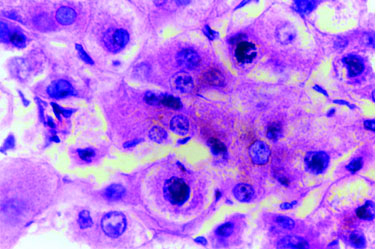
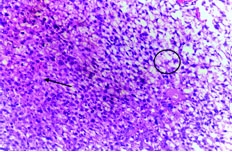
One case showed Hepatocellular carcinoma arising in a background of cirrhosis [Table/Fig-7,8]. Undifferentiated embryonal sarcoma was composed of a mixture of spindled and stellate cells in a myxoid stroma. The tumour cells exhibited a bubbly light pink cytoplasm [Table/Fig-9].
Hepatocellular carcinoma. Tumour shows pleomorphic, hyperchromatic nuclei with prominent nucleoli (arrow) with surrounding cirrhotic liver. (H&E, x100).
Hepatocellular carcinoma. Tumour shows pleomorphic, hyperchromatic nuclei with prominent nucleoli and abnormal mitotic figure. (H&E, x 450).
Undifferentiated embryonal sarcoma. Spindle to stellate cells in a myxoid stroma (arrow) and the tumour cells having bubbly light pink cytoplasm (circle). (H&E, x100).
Only one case of benign tumour (hepatocellular adenoma) was reported at six years in male patient in right lobe. Hepatocellular adenoma in our study presented as pedunculated mass measuring as 6 cm from inferior aspect of right lobe. Hepatocellular adenoma composed of sheets of tumour cells in trabeculae, two cells thick separated by compressed sinusoids and there were no fibrous septa or portal tracts within tumour tissue. The tumour cells were the same size or slightly larger than the normal hepatocytes [Table/Fig-10].
Hepatocellular adenoma. The tumour cells (arrow) are slightly larger resembling normal hepatocytes arranged in two to three cells thick trabeculae without areas of portal triad. (H&E, x100).
Out of a total of 39 cases, 22 cases involved the right lobe of liver, eight cases involved left lobe and 9 cases involved both lobes of liver.
In this study, AFP was done for 31 cases and correlation was done by comparison of mean value of AFP among the different tumour groups [Table/Fig-11]. A total of 22 cases of hepatoblastoma showed serum AFP level ranging from 280 to 60,000 ng/ml (about 20-4285 times that of normal). Serum AFP level was not done in six cases of hepatoblastoma. One case of epithelioid haemangioendothelioma showed 79 times of normal serum AFP (1108 ng/ml), not done in two cases and normal level in three cases. In both cases of hepatocellular carcinoma, serum AFP level was elevated, around 2140 times of normal. Serum AFP level was normal in one case of hepatocellular adenoma and in two cases of undifferentiated embryonal sarcoma.
Alpha fetoprotein levels in various paediatric liver tumours.
| Diagnosis | Mean AFP Level (ng/ml) | N | Std. Deviation |
|---|
| Hepatoblastoma | 42480.27 | 22 | 88187.448 |
| Hepatocellular carcinoma | 24977 | 2 | 7103.595 |
| Haemangioendothelioma | 279.98 | 4 | 552.017 |
| Hepatocellular adenoma | 1 | 1 | - |
| Undifferentiated embryonal sarcoma | 20.5 | 2 | 0.707 |
| Total | 31796.19 | 31 | 75933.441 |
In this study, follow up was available in six cases of hepatoblastoma and one case each of epithelioid haemangioendothelioma, hepatocellular carcinoma and undifferentiated embryonal sarcoma. Maximum three year follow up without tumour recurrence was available in two cases of hepatoblastoma. In both the cases, complete excision of the tumour and adjuvant chemotherapy (preoperative in one case and postoperative chemotherapy in other case) was given. Both cases were epithelial hepatoblastomas, in which one was purely fetal and other was combined fetal and embryonal and both cases were confined to the left lobe.
In all six cases of hepatoblastoma with longer survival more than one year, all were stage I tumour (resectable and limited to one lobe and complete excision of tumour was done in all six cases). A three year follow up without any recurrence in one case of hepatocellular carcinoma was available, in which preoperative chemotherapy, followed by complete excision of tumour was done. One year follow up without any recurrence in one case of undifferentiated embryonal sarcoma was seen, in which complete excision and postoperative chemotherapy was given. Only with medical treatment without any surgical treatment, three year survival was seen in one case of epithelioid haemangioendothelioma.
Discussion
Childhood liver tumours have received great attention because of their vast histologic variety, uncertainty about pathogenesis and classification and difficulties in treatment [2]. Hepatoblastoma accounts for 79% of all paediatric liver tumours and more than 90% manifest within four years of age. The histologic appearances of most of these tumours are epithelial [8–10]. These findings were also relatively similar to this study, in which hepatoblastoma accounted for 71.8% of all paediatric liver tumours and more than 90% within five years of age and 89.4% of these tumours were pure epithelial.
Undifferentiated embryonal sarcoma of liver was recognised as a clinicopathological entity by Stocker and Ishak in 1978 on the basis of an Armed Forces Institute of Pathology series of 31 cases. Histogenesis of this tumour remains undetermined though the possibility of being a malignant counterpart of mesenchymal hamartoma was raised by Stocker and Ishak [11]. Histological, histochemical (Periodic acid-Schiff staining for PAS positive globules) and Immunohistochemical studies (negative staining for all differentiated tumours) are necessary to distinguish it form other primary mesenchymal hepatic malignancies [12–14]. In these five years, we had two cases of undifferentiated embryonal sarcoma of the liver in eight and nine-year-old boys, which were diagnosed by positivity for PAS positive globules and by immunohistochemistry.
There were two cases of hepatocellular carcinoma in our study; age presentation in one case was nine years and 10 years in other. Yen Hsuan Ni studied 55 cases of hepatocellular carcinoma between the years of 1964 to 1989, in which the age range was three to 17 years; mean age was 9.7 years [4]. One case of hepatocellular adenoma at six years was reported in the present study.
In this study, two cases of undifferentiated embryonal sarcoma reported, age at presentation was eight years in one and nine years in other case. Mistry RC et al., reported two cases of undifferentiated embryonal sarcoma, both were nine-year-old at presentation [15]. Serum alpha-fetoprotein level was increased in hepatoblastoma and in hepatocellular carcinoma, normal in hepatocellular adenoma and in undifferentiated embryonal sarcoma. Serum AFP level was increased in few cases of epithelioid haemangioendothelioma.
The main mode of treatment for paediatric malignant liver tumour is resection of tumour. In unresectable tumours and in large tumours, preoperative chemotherapy was given, followed by surgical resection. Postoperative chemotherapy reduces incidence of recurrence after surgical resection. In this study, follow up was available only in nine cases, in which one was epithelioid haemangioendothelioma, remaining were malignant paediatric liver tumours. In all eight malignant paediatric liver tumours, complete resection of tumours was done and adjuvant therapy in the form of preoperative chemotherapy in some cases and postoperative chemotherapy in some cases. Yen Hsuan Ni et al., reported 71 cases of hepatocellular carcinoma, in which he observed only two long term survivors among 49 patients who could be followed more than five years, both received surgical resection [4]. Wei Jaco Chen et al., reported 55 cases of primary malignant tumour of liver in infants and children, he observed 60% resectable rate and 40% survival rate for hepatoblastoma but for hepatocellular carcinoma, the resectability was less than 10%. He observed no difference in survival time between those who had chemotherapy and those who did not. Early diagnosis and complete excision of tumour remains the only way to long-term survival [1]. Mistry et al., reported two cases of undifferentiated embryonal sarcoma in which one was alive four years after surgery and one died 16 months after surgical resection [15].
Metastatic liver tumours in children are rare and reports are scanty. Neuroblastoma is the most common tumour metastasizing to the liver in children followed by leukemia and lymphoma [16–18].
Limitation
This study is limited by its smaller sample size (39 cases) and the alpha fetoprotein values were not available for all the cases. This study is also limited by details regarding the post treatment follow up of these patients which were not available.
Conclusion
In this study, hepatoblastoma was the most common paediatric liver tumour (71.8%) with male to female ratio of 1:1.1 in contrast to male preponderance in the literature, the most common histological subtype being epithelial type composed of fetal and embryonal cell types. This was followed by epithelioid haemangioendothelioma (15.4%), hepatocellular carcinoma and undifferentiated embryonal sarcoma accounted for 5.1% each. Peak incidence of hepatoblastoma was between birth to one year and only one hepatoblastoma was reported above five years of age. Serum AFP level was increased in hepatoblastoma and in hepatocellular carcinoma, normal in hepatocellular adenoma and in undifferentiated embryonal sarcoma. Serum AFP level was increased in few cases of epithelioid haemangioendothelioma. Main mode of treatment for paediatric malignant hepatic tumour was surgical resection whenever possible and preoperative chemotherapy for large tumours to reduce size before surgery and also for unresectable tumours. Postoperative chemotherapy is used to reduce incidence of recurrence.
There has been a substantial improvement in survival of patients with paediatric liver tumours over 30 years. Through better understanding of pathological diagnosis, refined surgical staging, newer and more effective radiological techniques and standardized multimodal therapies, a substantial number of children diagnosed with this highly malignant tumour can expect to survive the disease.