GM is an uncommon chronic inflammatory disease of the breast which almost always mimics cancer in young individuals [1]. GM is a general term, which encompasses spectrum of pathological entities [2]. Aetiologically GM is divided into specific and non-specific types. The term “specific GM” is used when the aetiological factor can be identified [1]. These may be categorised as infectious causes like Mycobacterium tuberculosis, blastomycosis, cryptococcosis, histoplasmosis, actinomycosis, and filarial infection. Autoimmune process such as Wegener granulomatosis and giant cell arteritis. Foreign body reaction, duct ectasias, diabetes mellitus, sarcoidosis, and fat necrosis are other rare causes [1–3]. NGM is a condition for which no aetiological factors can be identified [1]. It is also known as Idiopathic Granulomatous Mastitis (IGM) or Granulomatous Lobular Mastitis (GLM) [3]. Among GM, TBM and NGM are important to be distinguished because they have overlapping clinical, radiological and cytological features and because their treatment differs considerably. They are often misinterpreted as carcinoma [4–6].
TBM is one of the rarest forms of extrapulmonary tuberculosis, as mammary tissue is inhospitable for the survival and multiplication of the bacilli [9]. Breast tuberculosis accounts for <0.1% of all breast lesions [5]. TBM may be the only manifestation of the disease or it may be a part of a systemic disease. TBM was first documented by Sir Astley Cooper in 1829 and called it scrofulous swelling of bosom [7,9]. World literature declares its incidence to be <1% [8,9]. In the Indian subcontinent, where tuberculosis is endemic, incidence of TBM may be as high as 4% [5,7,9,10]. Demonstration of the Acid Fast Bacilli (AFB) ensures definitive diagnosis [9]. Bacteriological culture and positive AFB by ZN stain though is the gold standard test for the diagnosis of tuberculosis, they are less sensitive in cases of TBM [9]. This may necessitate the use of expensive tests like PCR [5]. The optimal treatment of IGM is controversial. In most cases, steroid therapy has a good response. Wide surgical excision is advised in complicated cases, while TBM requires anti tubercular therapy for six months like pulmonary tuberculosis [11,12].
FNAC is a simple, noninvasive and patient friendly tool of investigation which provides accurate and early diagnosis [13]. It is the investigation of choice for any lump in the breast after the advent of triple test [8]. It plays a vital role in differentiating granulomatous diseases of the breast from carcinoma [9]. Its role in subtyping GM based on aetiology has been debated in the literature [2,14]. The likelihood of a definitive diagnosis at the primary level of FNAC avoids many other unnecessary and costly investigations [7]. In current literature, a clear cytological picture of various granulomatous diseases of the breast is rarely defined. Literature review discloses very few large case series which differentiates the various granulomatous diseases of the breast in terms of cytology [2,5]. Our attempt was to study and compare the clinical, radiological, and detailed cytological profile of various granulomatous conditions of the breast and pick up various clues which will promote a definitive diagnosis at FNAC level, to ensure early and effective treatment.
Materials and Methods
All the cases reported as GM in the Department of Cytopathology during the period between 2009 and 2016 were retrospectively searched from cytology files. The patient history and the cytology slides of all the cases were retrieved and studied. The histopathological slides of the available cases were reviewed and correlated with the cytological findings. The Institutional Ethical Committee Clearance was obtained for the study. In all cases, FNACs of the breast lump were performed by the pathologists using 22 or 23 gauge needle. FNAC of the axillary lymph node was done if it was well palpable. An average of six-eight stained slides were obtained in all cases, of which two smears each of haematoxylin and eosin stain and Leishman stain, one smear of ZN stain and one of PAS stain were found.
Patient details including age, sex, presenting symptoms, obstetrics history, relevant past medical history, and treatment history were collected from the case files. The radiological diagnoses when present were also recorded. The cytology slides of all the cases were examined by single pathologist for following parameters: presence of epithelioid cell, as granulomas or in singles, multi nucleated giant cells and their morphology, necrosis, caseous and non caseous, and type of background inflammation consisting of neutrophils, lymphocytes, and macrophages.
Results
Total 21 cases of GM were obtained over eight years. Of these, five cases were given a definitive diagnosis of TBM based on positive acid fast staining. The remaining 16 cases were labelled as NGM as they were AFB and PAS negative. Among the 16 NGM, four had histopathological correlation. None of our patients had a history suggestive of sarcoidosis, connective tissue disease, autoimmune disease, surgery for breast implants or any other infectious diseases. Microbiological cultures done on sinus/nipple discharge in six patients isolated no bacteria or fungal organisms. Thus, our study group consisted of only TBM and NGM patients. The shared feature among both NGM and TBM groups was that all the patients were females and presented with complaints of lump in breast.
In the NGM group, the youngest patient was 28-year-old and the oldest was 70-year-old. The mean age was 49 years. Majority of the patients belonged to 30–40 age group. The duration of symptoms varied from 15 days to two years. On examination, majority had firm to hard, ill defined lump, with an average size of about 4 cm x 3 cm. Out of 16 NGM patients’ majority, 10 (62.5%) complained of tenderness in the lump. Six (37%) had associated signs of inflammation in the form of redness, and raised temperature. Five (31%) had undergone prior Incision and Drainage (I&D) for breast abscess. One patient (6.25%) had an enlarged axillary lymph node. Two patients (12.5%) had draining sinus which developed after I&D. Four patients (25%) had clinical suspicion of malignancy with hard lump associated with nipple retraction and pued-u orange skin. Ultrasound and mammogram suggestive of malignancy was seen in 2 (12.5%) cases. Radiologically mastitis was diagnosed in 3 (18.75%) cases. One patient was pregnant (first trimester). One patient had a clinical diagnosis of fibroadenoma.
Among the TBM group, the youngest patient was 24-year-old and oldest was 45-year-old. The mean age was 34.5 years and most patients belonged to the 20–30 age group. The duration of their symptoms extended from 1 month to 10 months. The sizes of the lumps were smaller, with an average size of 2 cm x 2 cm. Interestingly, none of the patients complained of tenderness in the lump. Of the total five patients, 2 (40%) patients were known to have tuberculosis and were under treatment for the same. Two (40%) had an associated axillary lymphadenopathy. Three (60%) had multiple discharging sinuses either in the breast or axilla. Three (60%) had clinical suspicions of carcinoma breast. USG suggestive of mastitis was seen in 1 (20%) patient. The clinical picture has been summarised in [Table/Fig-1].
Clinical and radiological findings in NGM and TBM.
| Clinical Findings | NGM (n=16) | TBM (n=5) |
|---|
| No (%) | No (%) |
|---|
| Mean age (range) yrs | 49(28-70) | 34.5(24-45) |
| Duration of symptom | 15 days-2 years | 1 month-10 month |
| Mean size | 4 cm x 3cm | 2 cm x 2cm |
| Tenderness | 10(62.5%) | 0(0%) |
| Discharging sinus | 2(12.5%) | 3(60%) |
| Lymphadenopathy | 1(6.25%) | 2(40%) |
| Clinical suspicion of malignancy | 4(25%) | 3(60%) |
| Radiological Diagnosis | NGM | TGM |
| num(%) | num(%) |
| Malignancy | 2(12.5%) | nil |
| Mastitis | 3(18.7%) | 1(20%) |
NGM- Non-specific granulomatous mastitis, TBM- Tubercular mastitis
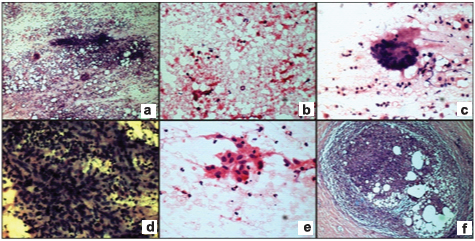
In the cytological smears of NGM, 14 (87.5%) smears showed ductal epithelial cells, many of them exhibiting reactive atypia. All the smears had epithelioid cells, either as epithelioid cell granulomas or as singly scattered intermixed with neutrophils [Table/Fig-2a]. Caseous necrosis, classically seen as a granular acellular eosinophilic material, was not seen in any of the smears. But necrotic material intermixed with degenerated neutrophils and apoptotic bodies were seen in 7 (43.7%) smears [Table/Fig-2b]. Giant cells, mostly foreign body type, were seen in 12 (75%) of the cases [Table/Fig-2a,c]. Epithelioid cell granulomas were seen in only 10 (62.5%) cases and singly scattered epithelioid cells were seen in 6 (37.5%) cases [Table/Fig-2d,e]. Histiocytes described as plump, elongated cell with dull nucleus were found in 13 (81.2 %) cases. Background inflammation was composed of neutrophils in 10 (62.5%) cases, lymphocytes in 2 (12.5%) and both cells were seen in 3 (18.75%) cases. One case did not show any background inflammation, and was composed of only epithelioid granulomas and foreign body giant cells. FNAC of the axillary lymph node of one patient yielded inadequate material. Histopathological slides of four cases showed granulomatous lobulitis with destroyed lobular architecture [Table/Fig-2f].
Photomicrography non-specific granulomatous mastititis showing: a) Epithelioid granulomas with foreign body giant cell in the background of neutrophils (H&E x100); b) Inflammatory necrosis admixed with neutrophils and apoptotic cells (H&E x100); c) Foreign body giant cell (H&E X400); d) Epithelioid granulomas admixed with neutrophils (H&E x400); e) Epithelioid cells singly scattered (H&E x400); f) Histopathological slide showing granulomatous lobulitis (H&E x100).
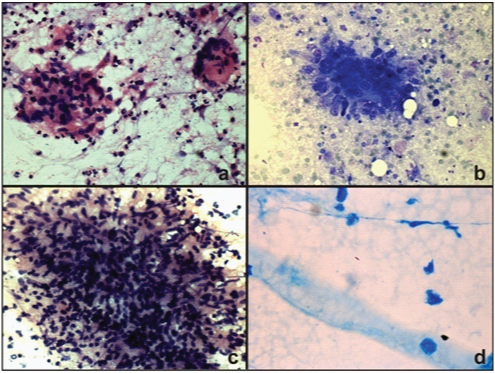
Of the five TBM smears, 2 (40%) cases had ductal epithelial cells, and 3 (60%) cases did not demonstrate any ductal epithelial cells. Epithelioid cells and giant cells, mainly Langhans and few foreign body types were present in 4 (80%) of the cases [Table/Fig-3a]. Epithelioid cell granulomas were seen in 4 (80%) of these. All the cases showed plump histiocytes either as singles or in clusters. Caseous necrosis was seen in 3 (60%) of cases [Table/Fig-3b] Background inflammation showed neutrophils in 1 (20%) case, and lymphocytes in 2 (40%) cases [Table/Fig-3c]. One case did not demonstrate any inflammatory cells or epithelioid cells but was composed entirely of caseous necrosis and few histiocytes in the periphery of the smear. All the five cases demonstrated AFB on ZN staining [Table/Fig-3d]. Smears from the axillary lymph node of one patient demonstrated granulomatous reaction while in case of other patient the material obtained was inadequate. The cytological findings are tabulated in [Table/Fig-4].
Photomicrography of tubercular mastitis showing, a) Epithelioid granuloma with Langhans giant cell (H&E, x100); b) Epithelioid granulomas in the background of caseous necrosis (Leishman stain, x400), c) Epithelioiod granuloma admixed with lymphocytes (H&E x400); d) Positive AFB (Ziehl–Neelsen, x1000).
Cytological findings in NGM and TBM.
| Cytological findings | NGM(n=16) | TBM(n=5) |
|---|
| No (%) | No (%) |
|---|
| Ductal cells | 14(87.5%) | 2(40%) |
| Epithelioid cells | 16(100%) | 4(80%) |
| Epithelioid cell granulomas | 10(62.5%) | 4(80%) |
| Caseous necrosis | nil | 3(60%) |
| Inflammatory necrosis | 7(43.7%) | 1(20%) |
| Foreign body giant Cells | 12(75%) | 2(40%) |
| Langhans giant Cells | nil | 4(80%) |
| Histiocytes | 13(81.2%) | 5(100%) |
| Neutrophils | 10(62.5%) | 1(20%) |
| Lymphocytes | 2(12.5%) | 2(40%) |
| Mixed (neutrophils+lymphocytes) | 3(18.75%) | nil |
Discussion
NGM and TBM constitute two rare causes of granulomatous disease of the breast. They interest many physicians due to their overlapping features and their resemblance to malignancy [2]. Both NGM and TBM is said to have low incidence [5,12]. In the tertiary care hospital where our study was conducted, NGM and TBM constituted 0.4% and 1.4% of the total breast lesions over eight years respectively. NGM is the diagnosis of exclusion and often requires biopsy for definitive diagnosis [4,5,15]. Tuberculosis, otherwise known as great mimicker requires demonstration of AFB. Demonstration of AFB in cytology smear of TBM requires the bacterial load to be 10,000 to 1,00,000/ml of the material and culture isolates organism only in 25% of the cases [7,9]. Since surgical intervention has no place in the treatment of the disease, biopsy would be an unnecessary procedure in both entities [15]. FNAC is a simple, noninvasive method which plays a vital role in differentiating GM from carcinoma breast [9]. Literature study reveals that FNAC along with special stain can diagnose TBM in 73% of cases. At times, ductal epithelial cells may demonstrate atypia in reaction to the inflammatory process in breast. In such situations, diagnosis may be difficult as malignancy can have an associated granulomatous reaction. This is where histopathology plays a role [8]. Conclusive diagnosis by FNAC will cut down the unnecessary investigative procedures and aid in early instigation of definitive therapy [7]. Though, both the entities have an overlapping cytological feature, our study highlights certain clinical and cytological differences which will aid definitive diagnosis at the preliminary level.
Clinical and Radiological Picture
NGM is said to be the disease of young to middle aged women, although literature reveals considerably wide age range of 11 to 83 years [5]. It is said to develop within a couple of years after giving birth and recent history of breastfeeding is often elicited [2,5]. In our study, patient ages ranged between 28 to 70 years with maximum number of patients aged between 30 to 40 and three women in the postmenopausal group. No recent history of breastfeeding could be elicited in any of our patients. Similarly study by Gupta RK did not reveal recent history of breastfeeding and last child birth was four to seven years ago in their patients [14]. While TBM can occur at any age, the documented age range in the literature varies from six months to 73 years [16]. Women of reproductive age are mainly affected due to frequent changes that the female breast undergoes during the childbearing period along with greater susceptibility to trauma and infection [9]. In our study, the maximum patients were aged between 20 and 30. Lactational periods have higher incidence of TBM as well. None of our patients were lactating at the time of presentation [16]. Thus, both the diseases affect women majorly in their reproductive age. In addition, our study revealed that TBM affects younger women as compared to NGM. A study by Kishore B et al., and Baharoon S et al., had similar findings [7,9]. However, in study by Seo HR et al., NGM patients were younger than TBM [5]. Similar to the literature, the duration of illness was highly variable in both the groups of our study, though it was comparatively shorter and TBM patients presented early [7,9].
NGM commonly presents as a unilateral and discrete hard breast lump [5]. Mass can vary from 0. 5 cm to as large as 9 cm. Mass may also be fixed to the underlying tissue associated with nipple retraction and sinus formation, raising suspicion of malignancy [3]. Likewise, majority of our patients had ill-defined firm to hard unilateral lump mainly in the outer quadrant. On an average, the lump was larger about the size of 4 cm x 4 cm. Four of them had clinical suspicion of malignancy. One had clinical diagnosis of fibroadenoma. TBM usually present with a solitary unilateral lump in breast. Multicentricity and bilateral lumps are rare occurring in less than 3% of patients [9]. Lumps may be ill-defined, well-defined and mobile, or hard and fixed to the parenchyma [9]. They may occur in any quadrant of the breast, with size varying from 1 cm to 8 cm. Patients may even present with ulceration of the skin or breast abscess [5]. In the present study, like NGM patients, TBM patients also presented with unilateral breast lump. Majority were mobile with an average size of 2 cm x 2 cm and occupying the central quadrant. Thus, the average size of the lump was smaller in TBM patients [17]. This is probably because they presented early in our cases. Lump was located mainly in the outer quadrant in NGM and central quadrant in TBM. This is supported by the fact that NGM is characterised by granulomatous lesion around the lobules and hence, unlikely to develop in the central quadrant while TBM can occur at any site as they are associated with ducts [3]. NGM is characterized by formation of micro abscess around the granulomatous response and hence presents with tenderness [2,5]. Significant number of NGM patients (62%) in our study complained of tenderness in the lump, whereas, none of the TBM patients had tenderness. In a study by Seo HR et al., 58% of IGM and 5% of TBM were associated with mastalgia [5]. Hence, eliciting history of tenderness of the lump may guide towards the right diagnosis.
Microabscess in NGM frequently brings the patients to clinics for abscess drainage [2,5]. About 31% of our patients gave a prior treatment history in the form of I&D, two among them developed discharging sinus after the procedure. This is often observed in many patients of NGM in the literature [2,3,5]. While spontaneous and persistent draining sinuses are typical of TBM [17]. Likewise, 40% of our patients in TBM group had persistent discharging sinus.
Tuberculous involvement of breast may occur via lymphatic, haematogenous, or contiguous seeding and rarely by direct inoculation of bacilli via the abraded nipple. The lymphatic route is the most likely route of breast involvement which occurs by retrograde extension from the axillary lymph node. This hypothesis is supported by the involvement of ipsilateral axillary nodes in 50% to 75% cases of TBM [8]. Correspondingly, 60% of TBM patients in our group had axillary lymphadenitis. Though rare, axillary lymphadenopathy can be seen in up to 15% of the patients with NGM [3]. It was seen only in 1 (16%) of our patients. In a study by Seo HR et al., the presence of axillary lymph nodes among IGM and TBM were 12% and 5% respectively [5].
Cytological Features
Cytology of the NGM is characterised by presence of non-caseating epithelioid granulomas, multinucleated giant cells with or without necrosis [18]. These findings overlap with that of TBM. Presence of epithelioid granulomas, along with caseous necrotic material, and Langhans giant cells are considered typical of TBM [5,17]. Our study also reflected these findings. NGM demonstrated epithelioid cells in 100% and TBM in 80% of smears. In NGM, epithelioid cell granulomas were seen in 65% of smears and in 37.5% smears epithelioid cells were seen singly scattered. Among TBM, epithelioid cell granulomas were demonstrated in all the cases. Study by Tse GMK et al., highlights that epithelioid cells when found in singles contribute towards the diagnosis of NGM [2]. Plump histiocytes were seen in 100% TBM and 81.2% of NGM smears. Our study is the first one to record the consistent presence of plump histiocytes in TBM. Multinucleated giant cells are common in granulomatous mastitis [17,18]. They were mostly foreign body type, seen in 75% NGM smears and Langhans giant cells seen in 60% of TBM smears. Caseous necrosis which appears as a ground glass eosinophilic material was only seen in TBM smears and absent in NGM smears [19]. This is another finding that is consistent with the findings in the existing literature [3,5,16]. Necrosis may also be a feature of NGM, but it is always associated with neutrophilic inflammation [2,5]. Our study demonstrated acute inflammatory necrosis composed of apoptotic and degenerated neutrophils in 43.7% of NGM smears. Majority of NGM smears showed neutrophils (62.5%), while majority of TBM smears (60%) had lymphocyte in the background. Our findings are supported by Tse GMK et al., who also found mainly neutrophils along with epithelioid granulomas in NGM smears [2]. In another study, lymphocytes predominance was found along with caseous necrosis in cytology smears of TBM [3].
Limitation
Limitations of the study were that all the cases of IGM diagnosed on cytology could be not followed up for histopathological diagnosis which is the gold standard test for IGM. All the cases of TBM were diagnosed based on positive AFB staining which is less sensitive test. PCR test which is sensitive and specific test for tuberculosis could not be performed due to financial constraints.
Conclusion
IGM and TBM are mimickers of malignancy and have overlapping features. With well elicited clinical history and careful search for specific cytological findings on FNAC smears these entities can be safely distinguished. Clinically young age of the patient, with shorter duration of illness presenting with breast lump mainly in the central quadrant, not associated with tenderness, points towards TBM. Tenderness in the breast lump which occupies the outer quadrant directs towards the NGM. Multiple and persistent discharging sinus is common in TBM while history of I&D is common in NGM. History of tuberculosis if often elicited in TBM patients, while no positive history is received from NGM patients. Axillary lymphadenopathy when present usually points towards TBM.
Cytologically epithelioid cells in singles and as granulomas are seen in both, but epithelioid cell granulomas are common in TBM and singly scattered ones are common in NGM. Caseous necrosis may be seen in TBM but are typically absent in smears of NGM. Multinucleated giant cells of foreign body are seen in NGM and Langhans type is seen in TBM. Predominance of neutrophils in the background favours NGMs and presence of lymphocyte favours TBM. In addition, use of special stains like ZN and PAS aids in accurate diagnosis.
NGM- Non-specific granulomatous mastitis, TBM- Tubercular mastitis