Rectus Sheath Haematoma Secondary to Enoxaparin Injection- A Rare Case Report
Sidharth Agarwal1, Yamanur P Lamani2, Bhimanagouda V Goudar3, Eshwar B Kalburgi4, Bheemappa K Bhavi5
1 Intern, Department of General Surgery, BVVS S Nijalingappa Medical College and HSK Hospital and Research Centre, Navanagar, Bagalkot, Karnataka, India.
2 Associate Professor, Department of General Surgery, BVVS S Nijalingappa Medical College and HSK Hospital and Research Centre, Navanagar, Bagalkot, Karnataka, India.
3 Professor, Department of General Surgery, BVVS S Nijalingappa Medical College and HSK Hospital and Research Centre, Navanagar, Bagalkot, Karnataka, India.
4 Professor and Head, Department of General Surgery, BVVS S Nijalingappa Medical College and HSK Hospital and Research Centre, Navanagar, Bagalkot, Karnataka, India.
5 Assistant Professor, Department of General Surgery, BVVS S Nijalingappa Medical College and HSK Hospital and Research Centre, Navanagar, Bagalkot, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sidharth Agarwal, Room No. 55, Kedar Boy’s Hostel No. 2, S Nijalingappa Medical College and HSK Hospital and Research Centre, Navanagar, Bagalkot-587103, Karnataka, India.
E-mail: sidhu.agarwal@gmail.com
Rectus sheath haematoma is a well-documented condition with an elusive diagnosis. It is an uncommon complication of anti-coagulation therapy, which can have a mortality of upto 25%. The patient discussed here is a 40-year-old female who was on Inj. Enoxaparin, who developed severe abdominal pain and hypovolemia after three days of treatment. Ultrasonography and CT scan showed a large rectus sheath haematoma on the right side, which was crossing the midline towards the left side. Inj. Enoxaparin was stopped and the patient was posted for surgery. In surgery, all clots were evacuated and inferior epigastric vessels were ligated. Patient recovered well following surgery. Here, this report presents forward a case of rectus sheath haematoma secondary to enoxaparin injection, its presentation and its surgical management.
Anticoagulation therapy, Mannitol, Muscle haematoma
Case Report
A 40-year-old female presented to the neuro physician with complains of headache, giddiness, vomiting and loose stools and altered sensorium since past one day. On examination, deviation of angle of mouth towards right, weakness of left upper and lower limbs, GCS 8/15 and an extensor plantar reflex was seen.
CT scan showed bilateral diffuse cerebral oedema. Suspecting a cerebrovascular stroke and increasing intracranial tension, the patient was intubated and started on Inj. Mannitol (150 ml i.v. Q4H) and antibiotics. As the patient was intubated, she was sedated using Inj. Midazolam till fifth day of treatment, when she was extubated. Inj. Dexomethasone (8 mg iv QD) and intravenous fluids were also started. The patient was extubated on fifth day and was started on Inj. Enoxaparin 60 mg subcutaneously BD on sixth day.
On the eighth day of treatment (day 3 on enoxaparin) patient complained of sudden development of abdominal pain. This was accompanied by tachycardia and sudden fall in blood pressure. The general surgery department was consulted for the above complaints. On examination, the patient was found to have extreme tenderness, and a vague mass was felt in the right iliac fossa, suprapubic region and left iliac fossa with positive Carnett’s sign and Fothergill sign. Repeat complete blood count, ultrasonography abdomen and pelvis, and CT scan abdomen and pelvis were advised.
Blood count reports showed a drop in haemoglobin level from 14.6 gm% at the time of admission to 7.1 gm% on the fourth day of enoxaparin treatment. Platelet count which was 353,000 cells/cu mm on admission had fallen to 252,000 cells/cu mm on the day of pain and then fell to 183,000 cells/cu mm the next day. Prothrombin time was 16 sec (Reference Range {RR}: 12-15 sec), control: 13 sec (RR: 13 sec), INR 1.20. Activated partial thromboplastin time: 30 sec (RR: 21-28 sec), control: 22 sec (RR: 22 sec). Clotting time: 3 min (RR: 1-6 min), bleeding time: 6 min (RR: 5-10 min).
The ultrasonography abdomen and pelvis showed a focal thick walled heterogeneous pelvic collection in the infra-umbilical region.
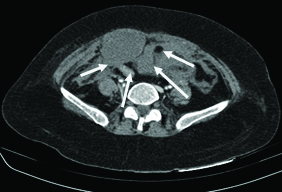
CT scan abdomen and pelvis showed a large (15.3 cm3 x 12.2 cm3 x 7.4 cm3) collection, approximately 720 ml, heterogeneous hyper dense collection in the right infra-umbilical anterior abdominal wall, proximally limited to the rectus sheath in epigastric region. Inferiorly extended to preperitoneal space of abdominal cavity crossing the mid line and extending to left side. There was extension into suprapubic region posterior to pubic symphisis and in prevesical region. Compression of bowel loops and bladder was also seen. The reports were suggestive of a Grade III rectus sheath haematoma [Table/Fig-1].
CT scan showing right rectus sheath haematoma.
Fluid aspiration cytology report from the infra-umbilical region showed few scattered polymorphs with abundant red blood cells in the background with no evidence of malignant cells.
Following investigations Inj. Enoxaparin was immediately stopped and Inj. Tranexamic acid was started. Two units of whole blood were transfused. Inj. Noradrenaline and Inj. Dopamine were started along with IV fluid resuscitation. The patient was also started on antibiotics.
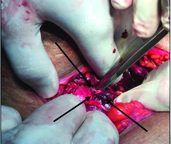
Once fit for surgery, patient was taken for exploration. Abdomen was opened through a right inguinal crease incision. All clots were evacuated and the inferior epigastric vessels were severed and ligated [Table/Fig-2]. Another two units blood transfusion was also done. Inotropic support was withdrawn two days after surgery. Recovery following surgery was uneventful.
Showing ligation of inferior epigastric vessels. Vessels held by forceps.
Discussion
Rectus sheath haematoma is bleeding into the rectus sheath due to damage to superior or inferior epigastric arteries or its branches or to the muscle itself. It is a well documented condition with deceitful diagnosis [1], which can be fatal. It is an uncommon but well documented complication of anticoagulation therapy [2]. It is two-three times more common in females, with an ultrasonographical incidence of 1.8% in hospitalized patients with abdominal pain [3]. An overall mortality of 4% and 25% for rectus sheath haematoma secondary to anticoagulation therapy has been reported.
Anticoagulants like enoxaparin are commonly used for conditions like cerebrovascular thrombosis, unstable angina, non Q wave myocardial infarction, acute ST segment elevation myocardial infarction and for treatment and prophylaxis for deep vein thrombosis. Enoxaparin is a subcutaneously administered low molecular weight heparin. Heparin induced immune microangiopathy is thought to be the cause of bleeding incidences associated with its administration.
Patient usually gives a peculiar history of sudden, severe, unilateral abdominal pain which aggravates on movement. Ecchymosis may sometimes present as a late feature. On examination, tenderness may be present along with a palpable abdominal lump. Fothergill and Carnett’s signs are usually positive [1]. There may also be unexplained tachycardia or hypotension, fall in haematocrit, peritoneal or bladder irritation, abdominal distension or abdominal cramping. A thorough history and examination are impeccable for diagnosis.
A few other conditions that rectus sheath haematoma needs to be differentiated from are appendicitis, sigmoid diverticulitis, inferior wall myocardial infarction, perforated ulcer, ovarian cyst torsion, intestinal obstruction, tumours and hernias [4].
Ultrasonography abdomen and pelvis is usually the first radiological investigation to be sent but, CT scan should always be considered as the choice of diagnostic modality, as it is believed to have 100% sensitivity [5]. Also, in 1996, Berna JD et al., used the CT scan finding to grade rectus sheath haematomas into three types depending on their severity and also put forward their therapeutic implications [6].
Treatment ranges over a wide range from conservative to surgical depending upon the CT scan reports [6]. Usually rectus sheath haematoma is a self limiting condition and can be managed conservatively [2,7]. For patients on oral anticoagulants; conservatively, reversal can be done with phytonadione plus fresh frozen plasma. Very few cases who are haemodynamically unstable with a large haematoma may require surgical intervention. Surgical interventions include embolization [8] of the bleeding vessels and ligation [9] of bleeding vessels. In this case, surgical intervention was preferred because of the large haematoma, presence of peritoneal signs and the severe haemodynamic compromise.
Conclusion
Patients on anticoagulation therapy should be closely observed and any complains of pain abdomen should be thoroughly investigated. Doctors should have a high level of suspicion and clinical examination skills. Subcutaneous injections should be administered by trained medical or nursing staff and they should be well aware of the possible complications.
[1]. Maharaj D, Ramdass M, Teelucksingh S, Perry A, Narayansingh V, Rectus sheath haematoma: a new set of diagnostic featuresPostgrad Med J 2002 78(926):755-56. [Google Scholar]
[2]. Berna JD, Zuazu I, Madrigal M, García-Medina V, Fernández C, Guirado F, Conservative treatment of large rectus sheath hematoma in patients undergoing anticoagulant therapyAbdom Imaging 2000 25:230-34. [Google Scholar]
[3]. Klingler PJ, Westscher G, Glaser K, Tschmelitsch J, Schmid T, Hinder RA, The use of ultrasound to differentiate rectus sheath haematoma from other acute abdominal disordersSurg Endosc 1999 13(11):1129-34. [Google Scholar]
[4]. Turkoglu E, Guven H, Gurer B, Comoglu S, Abdominal wall haematoma in cardioembolic stroke due to enoxaparine therapy: a report of two casesCase Reports 2009 2009(jun11 2):bcr0220091566 [Google Scholar]
[5]. Moreno GA, Aguayo JL, Flores B, Soria T, Hernandez Q, Ortiz S, Ultrasonography and computed tomography reduce unnecessary surgery in abdominal rectus sheath hematomaBr J Surg 1997 84:1295-97. [Google Scholar]
[6]. Berna JD, Garcia-Medina V, Guirao J, Garcia-Medina J, Rectus sheath hematoma: diagnostic classification by CTAbdom Imaging 1996 21:62-64. [Google Scholar]
[7]. Kapan S, Turhan AN, Alis H, Kalayci MU, Hatipoglu S, Yigitbas H, Rectus sheath haematoma: three case reportsJ Med Case Rep 2008 2:22 [Google Scholar]
[8]. Holmes SJ, Yale SH, Mazza JJ, Rectus sheath hematoma as a cause of acute abdominal painAm Fam Phys 2001 64:1681 [Google Scholar]
[9]. Ducatman BS, Ludwig J, Hurt RD, Fatal rectus sheath hematomaJ Am Med Assoc 1983 249:924-25. [Google Scholar]