Tuberculosis of Acromioclavicular Joint
Archit Agarwal1, Amish Bhandari2, Rajesh Maheshwari3
1 Senior Resident, Department of Orthopaedics, Himalayan Institute of Medical Sciences, Dehradun, Uttrakhand, India.
2 Junior Resident, Department of Orthopaedics, Himalayan Institute of Medical Sciences, Dehradun, Uttrakhand, India.
3 Professor and Head, Department of Orthopaedics, Himalayan Institute of Medical Sciences, Dehradun, Uttrakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Archit Agarwal, 89, Ram Vihar, Near ONGC Hospital, Dehradun-248003, Uttrakhand, India.
E-mail: dr.architagarwal@gmail.com
Tuberculosis (TB) arthritis accounts for approximately 1%–3% of all cases of TB and for approximately 10%–11% of extra pulmonary cases. Isolated acromioclavicular joint TB has been reported rarely with varied presentations as case series of one to three cases none of them being large studies. In our case, patient presented with pain in left shoulder since one month. Patient was investigated and was diagnosed to have acromioclavicular joint TB on basis of positive Acid Fast Bacilli (AFB) stain and cytology. Patient recovered well with antitubercular therapy. Thus, it is important to send Ziehl-Neelsen (ZN) stain in all cases in an endemic country like India.
Acid fast bacilli, Isoniazid, Shoulder girdle
Case Report
A 30-year-old female presented to emergency department complaining of pain and swelling at the left shoulder for one month. Pain had increased in intensity and was localized to the left shoulder anteriorly. Pain increased on movement of the shoulder and was relieved with analgesics. There was no history of constitutional symptoms. No past history of TB or any contact with individuals suffering from TB was present. The patient belonged to a low socioeconomic status and had history of living in overcrowded condition.
On examination, there was mild swelling present over the anterior aspect of the left shoulder which did not appear to be inflamed. There was tenderness present at the acromioclavicular joint but there was no warmth present. Full passive range of motion was present at the shoulder but was painful. No scars or sinus were seen. Patient appeared to be suffering from low grade subcutaneous infection.
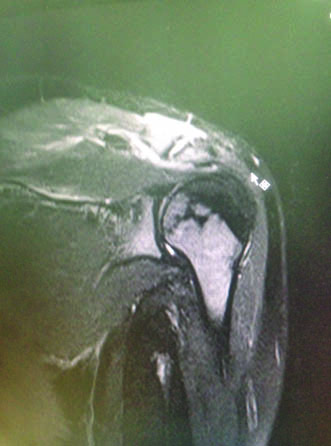
Blood investigations were carried out. Erythrocyte Sedimentation Rate (ESR) was elevated at 39 mm/h, haemoglobin- 8.91 g/dl, total leucocyte count of- 14000/cumm, neutrophils- 80%, lymphocytes 15%, C-reactive protein was 93.01. Montoux was read as 11 mm of induration. On X-Ray of shoulder, no obvious bony pathology was seen. MRI was done and showed focal collection in the trapezius muscle attachment at lateral third of clavicle and acromion process with subcutaneous oedema. Contrast MRI was done which showed collection in trapezius muscle, extending from subcutaneous tissue to acromioclavicular joint [Table/Fig-1].
Contrast MRI showing involvement of acromioclavicular joint.
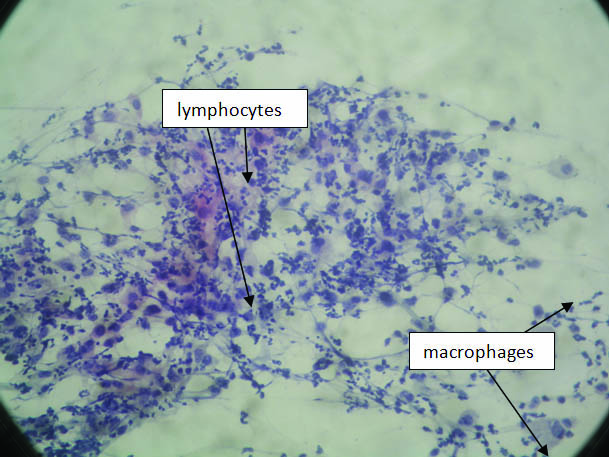
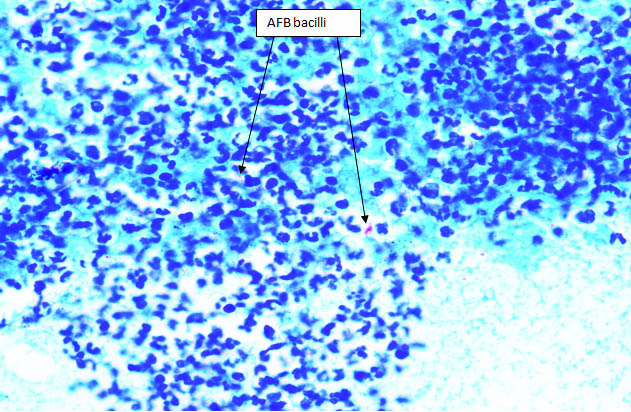
On aspiration of anterior aspect of shoulder at acromioclavicular joint, thick brown coloured pus was found which was sent for culture sensitivity cytopathology and ZN stain. Incision and drainage was done and the wound was left open for pus to drain. There was no growth in culture. The cytology examination of pus showed acute on chronic inflammation comprising of polymorphs with lymphocytes, eosinophils, macrophages, histiocytes and plasma cells [Table/Fig-2]. On ZN stain, few acid fast bacilli were seen [Table/Fig-3]. The patient was started on a multidrug anti-tubercular therapy considering it to be case of acromioclavicular joint TB. The amount of pus discharge reduced over the following two weeks. Wound healed with secondary intention.
Cytopathology examination of pus.
AFB bacilli seen in ZN stain.
Patient was advised to do active shoulder mobilisation. Patient continued treatment with four drugs for three months: Rifampicin (RIF) (600 mg OD), Isoniazid (INH) (300 mg OD), Pyrazinamide (PZA) (1500 mg OD), Ethambutol (EMB) (800 mg OD). Later this was changed to INH and RIF for a further nine months. On follow up visits, ESR showed a consistently decreasing trend. At final one year follow up since the initial presentation ESR was normal and the patient had regained full range of motion.
Discussion
India continues to remain as on the High Burden Country (HBC) list for TB by WHO in the post-2015 era. India, Indonesia and China had the largest number of cases: 23%, 10% and 10% of the global total, respectively [1]. Such is the burden on our healthcare; it is therefore obvious that TB can have varied presentations. Therefore, TB should be considered as a differential diagnosis in all atypical presentations and final diagnosis should be made after histopathological confirmation [2].
TB arthritis accounts for approximately 1%–3% of all cases of TB and for approximately 10%–11% of extra pulmonary cases [3]. Patients and clinicians often overlook subtle findings such as early limitation of range of motion and minimal swelling when diagnosing TB arthritis. As the disease progresses the symptoms worsen [4]. Haematogenous spread of bacilli from infected visceral focus often leads to osteoarticular TB [5]. A positive biopsy showing the typical tubercles remains the ‘gold standard’ for diagnosis [5]. ZN staining is the easiest and quickest diagnostic test. Even though it has a limited sensitivity (46%–78%), specificity is virtually 100% [6]. ZN staining requires 105 bacilli/ml. Osteoarticular TB is a pauci-bacillary disease and is ZN stain positive [6].
TB of the acromioclavicular joint was first reported in 1950 [7]. In a series of 1,074 unusual lesions of TB, there was just one case of acromial end of clavicle involvement. There was cold abscess along with a sinus [8]. In the present case, sinus formation may have occurred if the patient had presented later. Scrofuloderma (involvement of the skin overlying a contiguous TB focus) arising from an underlying infection of the acromioclavicular joint in an immunocompetent female adult has been reported [9].
Antitubercular therapy has proved to be effective over the years. Debridement has been used along with antitubercular therapy to give better and faster results. Richter R et al., published their work spanning more than 25 years [10]. They treated 11 cases with tuberculous osteoarthritis out of which just one had acromioclavicular joint focus. They also used antitubercular therapy along with surgical intervention as done in the present case. In cases of multidrug resistant tuberculosis, second line anti tubercular drugs has been useful [11].
TB can mimic almost any type of lesion. In absence of pulmonary lesions, TB may not come to mind as the first diagnosis [12]. In a retrospective study, out of 16 patients of glenohumeral tubercular osteoarthritis 14 were misdiagnosed as frozen shoulder. The mean prediagnostic time period to come to a correct diagnosis was 14.5 months and it was concluded that TB should be considered in cases of longstanding shoulder pain [13]. Therefore, it is not necessary to have active TB or history of TB in a patient suffering from shoulder girdle TB. It is important to realize that osteoarticular TB can be a primary and isolated lesion [14]. Absence of systemic symptoms, indolent course of disease and nonspecific symptoms make diagnosis difficult. TB of the knee joint is also reported to have been a belated diagnosis due to lack of familiarity of the disease [15]. Therefore, TB should be considered as a differential diagnosis in all atypical presentations.
A triad of radiographic findings (Phemister’s triad) is characteristic of tubercular arthritis: severe periarticular osteoporosis, peripherally located osseous erosions and gradual narrowing of the interosseous space [16]. This was not present in the current case because the joint was not destroyed by the time the patient was diagnosed.
Several other atypical sites of osteoarticular TB have been reported for example talus, calcaneum, ulna and radius. In 83% of these cases, the most common symptom of presentation was long-standing pain and functional loss just as in the current case [17]. It is also stated that low socioeconomic status and crowded living conditions were a risk factor for osteoarticular TB even in vaccinated people [17].
Conclusion
The most common presentation of patients with shoulder girdle TB is long-standing pain which is followed by restricted range of motion. It can be said that in a HBC such as India, TB should be considered as a differential diagnosis so early diagnosis can be made and residual problems avoided. For early diagnosis, ZN staining and fluid cytology should always be done as it is cheap, fast and easily available.
[1]. World Health Organization. Global tuberculosis report 2015. World Health Organization; 2015 [Google Scholar]
[2]. Agarwal A, Maheshwari R, Maheshwari R, Tubercular osteomyelitis clavicle: A case reportJournal of Orthopaedic Case Reports 2014 4(4):52-53. [Google Scholar]
[3]. Haldar S, Ghosh P, Ghosh A, Tuberculous arthritis—the challenges and opportunities: Observations from a tertiary centerIndian Journal of Rheumatology 2011 6(1):62-68. [Google Scholar]
[4]. Agathangelidis F, Boutsiadis A, Fouka E, Karataglis D, Concomitant acromioclavicular and miliary tuberculosisBMJ case reports 2013 2013:bcr2013010026 [Google Scholar]
[5]. Tuli SM, Tuberculosis of the skeletal system: Bones, joints, spine and bursal sheaths 2004 Jaypee Brothers Publishers:167-68. [Google Scholar]
[6]. Vardhan V, Yanamandra U, Diagnosis of osteoarticular tuberculosisIndian J of Rheumatology 2011 6(1):87-94. [Google Scholar]
[7]. Taub SJ, Friedman IA, Dibble JB, Tuberculosis of the acromioclavicular joint with subscapular bursitis and effusionIll Med J 1950 2013:357-60. [Google Scholar]
[8]. Tuli SM, Sinha GP, Skeletal tuberculosis "Unusual" lesionsIndian Journal of Orthopaedics 1969 3(1):5 [Google Scholar]
[9]. Tan WP, Tang MB, Tan HH, Scrofuloderma from the acromioclavicular joint presenting as a chronic ulcer in an immunocompetent hostSingapore Medical Journal 2007 48(9):e243-45. [Google Scholar]
[10]. Richter R, Hahn H, Nübling W, Köhler G, Shoulder girdle and shoulder joint tuberculosisZeitschrift fur Rheumatologie 1984 44(2):87-92. [Google Scholar]
[11]. Suárez-García I, Noguerado A, Drug treatment of multidrug-resistant osteoarticular tuberculosis: A systematic literature reviewInternational Journal of Infectious Diseases 2012 (16):e774-78. [Google Scholar]
[12]. Basanagoudar PL, Gupta PN, Bahadur R, Dhillon MS, Tuberculosis of the clavicle presenting as an expansile lytic lesion: A case reportActa Orthopaedica Belgica 2001 67(5):505-09. [Google Scholar]
[13]. Li JQ, Tang KL, Xu HT, Li QY, Zhang SX, Glenohumeral joint tuberculosis that mimics frozen shoulder: A retrospective analysisJournal of Shoulder and Elbow Surgery 2012 21(9):1207-12. [Google Scholar]
[14]. Kapukaya A, Subasi M, Bukte Y, Gur A, Tuzuner T, Kilnc N, Tuberculosis of the shoulder jointJoint Bone Spine 2006 73(2):177-81. [Google Scholar]
[15]. Erdem H, Baylan O, Simsek I, Dinc A, Pay S, Kocaoglu M, Delayed diagnosis of tuberculous arthritisJapanese Journal of Infectious Diseases 2005 58(6):373 [Google Scholar]
[16]. Resnick D, Niwayama G, Diagnosis of bone and joint DisorderVol.42nd edW.B. Saunders Publication:2678-85. [Google Scholar]
[17]. Rafiqi K, Yousri B, Arihi M, Bjitro C, Aboumaarouf M, El Andaloussi M, Unusual locations of osteoarticular tuberculosis in children: A report of 12 casesOrthopaedics and Traumatology: Surgery and Research 2013 99(3):347-51. [Google Scholar]