Eyelid tumours are relatively rare diverse group of diseases varied in their presentations and extent. These tumours require individually tailored distinct diagnostic and treatment considerations. Their management is usually not simple due to the functional and aesthetic importance of the eye and the periocular structures and also due to their unique metastatic behaviour. In this article, we share our experience of the cases of malignant tumours of the eyelid from a tertiary referral hospital located in a semi urban part of South India.
Case 1
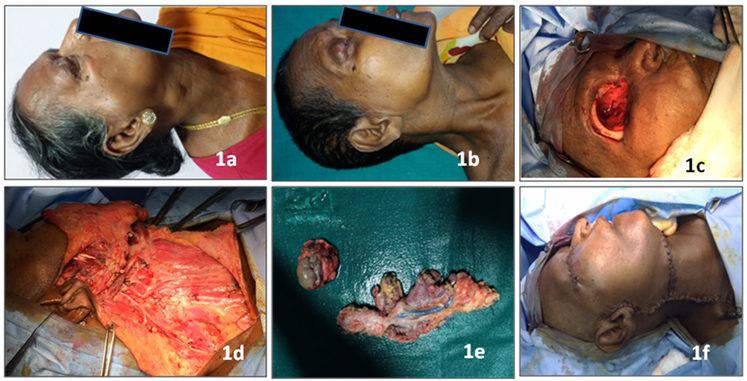
A 60-year-old female presented with right upper eyelid swelling associated with pain for nine months and redness and discharge from right eye for a month. She also had eye irritation, reduced vision and inability to open eye fully. Her past history was suggestive of surgery done four years back with excision and local flap reconstruction for squamous cell carcinoma in the right upper eyelid.
On examination, there was proptosis of right eye and right upper eyelid had a swelling of size 5x4 cm in the temporal aspect with ill-defined margins and overlying skin erythema. Posterior limit of the lesion could not be marked out. Conjunctival chemosis was present with corneal haziness. She also had preauricular matted lymph nodes with restricted mobility and discrete mobile level II and III cervical lymph nodes in the ipsilateral side.
Contrast Enhanced Computed Tomography (CECT) showed heterogeneously enhancing extraconal mass lesion 35x30x25 mm in the right upper eyelid causing mass effect pushing the globe and lateral rectus medially with loss of fat plane. Lacrimal gland could not be visualised separately. In addition, there was a homogenously enhancing mass lesion of 45x32x22 mm involving superficial lobe of parotid with loss of fat plane between the mass and the masseter muscle, extending superficial to zygomatic arch. Multiple significant enhancing right cervical lymph nodes were present in the levels Ib, II, III, IV, Va and Vb, largest being level II node of 18x12 mm size, showing heterogenous enhancement. Clinical diagnosis of recurrent squamous cell carcinoma of right upper eyelid with multiple ipsilateral metastatic cervical lymphadenopathy including preauricular lymph nodes was arrived at. After Fine Needle Aspiration Cytology (FNAC) confirmation, case was discussed in the multidisciplinary forum. It was decided to downsize the lesions with neoadjuvant chemotherapy in view of the extensive and rapidly progressive nature of the disease. Patient received three cycles of neoadjuvant chemotherapy with cisplatin and 5-fluoro uracil. There was a partial response and patient was then reassessed with Magnetic Resonance Imaging (MRI) and taken up for surgery. Right Orbital Exenteration (OE) with Extended Right Radical Neck Dissection (ERND) preserving the spinal accessory nerve along with total parotidectomy was carried out. Histopathological Examination (HPE) of postoperative specimen showed poorly differentiated squamous cell carcinoma with all margins negative for malignancy. Nine out of 19 lymph nodes examined were positive for metastases, including intra parotid lymph nodes. Postoperatively patient was treated with adjuvant chemotherapy and radiotherapy. On follow up of the patient until date (one year after surgery), she was free from disease [Table/Fig-1a-f].
1a: Right upper eyelid squamous cell carcinoma with preauricular and upper deep cervical lymph node metastasis. 1b: After induction chemotherapy; 1c: Intraoperative photograph of right Orbital Exenteration (OE); 1d: Intraoperative photograph showing Extended Radical Neck Dissection (ERND); 1e: Photograph of the specimen of OE and ERND; 1f: Immediate postoperative picture after primary closure.
Case 2
A 60-year-old female presented with complaint of a black nodular lesion in the left lower eyelid since two years, progressively increasing since six months. On examination, 15x10 mm hyper pigmented ulcerative nodular lesion was seen in the lateral third of left lower eyelid. A clinical diagnosis of pigmented Basal Cell Carcinoma (BCC) was made. Clinically there was no evidence of any regional lymphadenopathy. Edge wedge biopsy was suggestive of pigmented BCC. The lesion was excised with a 4 mm margin and lower eyelid defect was reconstructed with local rotational flap. HPE of excised specimen confirmed pigmented BCC with negative margins [Table/Fig-2a-d].
2a: Left lower eyelid basal cell carcinoma; 2b: Wide local excision intraoperative picture; 2c: Postoperative picture. 2d: Postoperative picture showing function preservation.

Case 3
A 55-year-old female was presented with pain, redness and watering of the left eye with history of defective vision for two months. On examination fleshy growth of 3x2 cm size in the temporal aspect of the palpebral conjunctiva of left upper eyelid extending into the bulbar conjunctiva and cornea causing ectropion and corneal ulceration with iris prolapse along with chemosis and nasal pterygium. Magnetic Resonance Imaging (MRI) showed mass lesion in the supero lateral aspect of the left orbit enmeshing superior rectus muscle, pushing the globe inferomedially with loss of fat plane. Lacrimal gland could not be identified separately from the mass. There was no cervical lymphadenopathy. Biopsy report was squamous cell carcinoma. After multidisciplinary consultation, orbital exentertion with temporalis muscle flap for socket fill up was done. Patient is on follow up for nine months with No Evidence of Disease (NED) [Table/Fig-3a-d].
3a: Left upper eyelid squamous cell carcinoma in the palpebral conjunctiva extending into the bulbar conjunctiva and cornea causing ectropion and corneal ulceration with iris prolapsed; 3b: Intraoperative photograph of left OE; 3c: Postoperative picture. 3d: Postoperative picture showing preservation of aesthesis.

Case 4
A 50-Year-old female was referred from ophthalmology department with history of wide excision and lid reconstruction for Malignant Proliferating Trichilemmal Tumour (MPTT) of left upper eyelid that she underwent two years ago. One year later, she presented with painful left preauricular swelling rapidly increasing in size for past two months. On examination, a hard irregular mass of size 4x3 cm. was present in the left preauricular area associated with overlying skin involvement. Pinna, post auricular area and external auditory canal were normal. Left level I and II cervical lymphadenopathy with the largest node measuring 2 cm was made out. A clinical diagnosis of metastatic lymphadenopathy was made considering the history of malignant tumour in the ipsilateral upper left eyelid and the presentation of nodular swellings in the regional drainage area of eyelid.
The patient was further evaluated with CECT head and neck, which revealed heterogenous mass lesion enhancing with contrast of 40x35 mm involving the superficial part of left parotid gland infiltrating adjacent part of the masseter. Multiple ipsilateral enlarged cervical lymph nodes, largest measuring 20x15 mm in level II was also made out. Chest X-ray was normal. FNAC of left pre auricular swelling was reported as showing features of metastatic lymphadenopathy and primary malignant tumour from parotid gland could not be ruled out. After multidisciplinary consultation, extended left radical parotidectomy with radical neck dissection with preservation of spinal accessory nerve and local flap reconstruction of the defect was done.
Postoperative period went uneventful. HPE of postoperative specimen was reported as mucoepidermoid carcinoma of high grade in the superficial lobe of parotid gland. Deep lobe was free of tumour. One out of 18 lymph nodes was positive for metastatic deposits. Due to the presence of high-risk features for recurrence, she was advised postoperative radiotherapy [Table/Fig-4a-d].
4a: Malignant parotid tumour in the left side as second primary cancer metachronous to left upper eyelid malignant proliferating trichilemmal tumour; 4b: Intraoperative photograph of extended left radical parotidectomy with radical neck dissection with preservation of spinal accessory nerve and local flap reconstruction; 4c: Immediate postoperative picture; 4d: After postoperative adjuvant radiotherapy.

All the patients recovered satisfactorily after surgery without any serious complications in the immediate postoperative period. Two patients who were at high risk for recurrence underwent postoperative adjuvant radiotherapy. It has to be mentioned that sight had been almost completely lost in the eyeballs of the patient which had presented clinical and radiological evidence of invasion of the extrinsic muscles and fat tissue of the orbit. All the patients had normal sight contra laterally.
Discussion
The eyelids are accessory visual structures with important function of protecting the eyes, composed of anterior and posterior lamellae which divide along the mucocutaneous lid margin. From anterior to posterior, the eyelid is composed of skin and subcutaneous tissue, orbicularis muscle, tarsus and conjunctiva [1]. The eyelid skin is the thinnest in the body and lacks subcutaneous fat, but otherwise contains all other skin structures viz., hair follicles and accessory glandular structures of eccrine and apocrine type. Among the accessory glands there are the sweat glands of the eyelid skin, the apocrine gland of moll, the accessory lacrimal gland of Krause and Wolfring, the meibomian glands and the glands of Zeiss. The epithelium of the skin is keratinized stratified squamous epithelium. Melanocytes are spread in the basal layer of the epithelium. The dermis contains fibrous tissue, blood vessels, lymphatic vessels and nerves. The posterior eyelid surface is lined by the palpebral conjunctiva that is composed of epithelium and sub epithelial stroma of fibro vascular connective tissue.
The tumours of the eyelid can be located anywhere through the whole thickness of the upper and lower lids, including the medial and lateral canthus areas; conjunctival tumours are lesions from the bulbar conjunctiva, fornix and limbus [2].
Tumours of the eye and its appendages are rare with different incidence and prevalence rates reported in different parts of the world. In spite of being a small organ, the eyelids contain numerous histological elements that can be the origin of a variety of benign and malignant lesions.
Tumours of the eyelid are classified according to their tissue or cell of origin and as benign or malignant [3,4]. Mostly eyelid tumours are of cutaneous origin, mainly epidermal, which can be divided into epithelial and melanocytic tumours. Tumours of the skin epithelium are divided according to their clinical behaviour and histopathologic findings into three main groups; benign, precancerous and malignant [5]. The eyelid adnexal tumours can be divided into cystic or solid lesions of either benign or malignant nature. These tumours arise from hair follicles, sweat glands, sebaceous glands and accessory lacrimal glands. Cystic lesions may occur due to obstruction in the duct, trauma, surgery or inflammatory process. Eyelid stromal tumours are classified according to their tissue of origin [6]. The tumour biology of eyelid carcinomas encompasses a wide range of behaviours from indolent low-grade nodular tumours to highly aggressive sebaceous gland carcinoma and merkel cell carcinomas.
Benign epithelial lesions, BCC, cystic lesions and melanocytic lesions represent about 85% of all eyelid tumours [7]. Cutaneous SCC and melanoma are relatively rare. Adnexal and stromal tumours are less frequent. Other tumours of the eyelid are lymphoid tumours, hamartomas and choristomas. Inflammatory and infectious lesions that can simulate neoplasms are not uncommon.
It is a consensus among all reports that the four most common malignancies involving the eyelids are BCC, SCC, Sebaceous Gland Carcinoma (SGC) and Malignant Melanoma (MM) [8]. However, their relative frequencies differ [9–11]. BCC is usually the most common and accounts for more than 80% of eyelid malignancies in Singapore and USA [9,11]. There are no published reports describing the epidemiology of eyelid tumours in many countries. The Western and Asian data have considerable variations in case distribution and presentation [8,9]. The main malignant tumours affecting the eyelid are BCC, SGC, SCC and MM in that order of frequency in Asia; SGC and BCC forms, majority of tumours in India [12]. SCC is rare in Indian population and generally occurs in predisposed individuals like in patients with xeroderma pigmentosa [12].
Of the four common types of eyelid cancers [5], BCC of the eyelid usually affects adults, but may also occur in younger people. They are related to sun exposure and are similar to basal cell carcinoma of the skin. BCC most often occurs in the lower eyelid. SCC can occur from a pre cancerous condition, such as actinic keratosis or Bowen’s disease. These tumours are also related to sun exposure and are similar to SCC of the Skin. SCC tends to behave more aggressively and is more likely to spread than BCC. SGC is cancer of the glands in the eyelid [13]. It occurs more often in women than men and occurs most often in the elderly. These tumours develop most often on the upper eyelid, followed by the lower eyelid and the caruncle. SGC can start in the meibomian glands, glands of zeis or the sebaceous glands of the caruncle. SGC is often diagnosed at a later stage because it can mimic benign conditions [13]. It can also grow aggressively. SGC may be multifocal, so they have a tendency to recur after treatment. MM of the eyelid is very uncommon and accounts for less than 1% of all eyelid cancers. MM of the eyelid is similar to melanoma of the skin, staged and treated the same way as a skin melanoma [5]. Delayed or mistaken diagnosis is very common with eyelid malignancies and progression of disease that may lead to infiltration of postseptal orbital structures, including the lacrimal gland and thus locally advanced cases are not uncommon.
Eyelid tumours evaluation includes assessment of primary tumour extent considering the possibility of malignancy masqueraders [14]. Additionally, orbital extension assessment clinically and by CECT scans and/or MRI scans is done along with delineation of the accurate extent of the lesion [15]. Assessment for lymph node spread is an essential part of the clinical examination to assess involvement of preauricular, parotid, submandibular and cervical lymph nodes. Biopsy of the lesion is necessary for confirmation and identification of the cell type and the presence of perineural invasion. Since metastatic potential is highly dependent upon histopathologic type and grade, biopsy helps guiding further workup for metastasis, in treatment decisions and in prognostication.
A Tumour Node Metastasis (TNM) based staging classification system by Union for International Cancer Control (UICC) to describe the extent of cancers is available for eyelid carcinomas as like many other solid cancers. The TNM staging system for eyelid carcinomas applies to basal cell carcinoma, SCC and SGC. However, pathologic staging is the single most important prognosticator [5]: Factors such as larger size, incomplete excision, histopathologic features such as poor differentiation, multicentric origin, pagetoid spread and delayed diagnosis were known or thought to be associated with poor prognosis [16,17]. BCC of the eyelid does not usually spread to lymph nodes or other organs, therefore they have good prognosis. SCC and can spread to the orbit, lymph nodes or other organs and is more aggressive than BCC. But if SCC of the eyelid is detected early and is completely removed, the prognosis is good. SGC of the eyelid has mortality rate of about 5%–10% [18]. But sebaceous gland tumours are not diagnosed early and have a high rate of recurrence and metastasis.
The goal of treatment is cure of the cancer with maximum preservation of function and cosmetics. Surgical approaches often offer the most efficient and effective means for accomplishing cure. There is a general consensus that complete surgical excision is the essential element in the treatment of primary malignant eyelid tumours. If an eyelid lesion is localized and seems to be well circumscribed, it can be managed by excision and eyelid reconstruction with histopathological section control of surgical margins. The recommended surgical margins for Standard Surgical Excision (SSE) with Postoperative Margin Assessment (POMA) for BCC is 4 mm and 4 mm to 6 mm for SCC, low risk subtypes [19,20]. Eyelid reconstructive techniques generally include direct closure for defects measuring less than 25%, direct closure with lateral canthotomy and cantholysis for defects measuring slightly larger than 25% and Tenzel semicircular rotational flap for defects up to 2/3’s of upper or lower lid width. Lid-sharing procedure was used when the defect is too large to be closed by Tenzel semicircular rotational flap such as Hughes flap technique for lower eyelid defect, reverse Hughes flap or Cutler-Beard surgical technique for upper eyelid defect [21].
An evidence-based review reported that for BCC, SCC and SGC, the published evidence support two recommendations, Moh’s micrographic surgery or excision with frozen-section control [22] and were graded as grade I recommendation. For sebaceous gland carcinoma, the recommendations also included conjunctival map biopsies. It concluded that the strongest evidence favours complete surgical removal using histopathologic controls for verifying tumour free margins of excision. Supplemental cryotherapy, topical chemotherapy and irradiation should be applied if the tumour margin is unclear or if there is residual involvement of bulbar conjunctiva [23–25]. Indications for adjuvant radiotherapy were unclear, tumour margins and/or presence of multiple nodal metastases or presence of extra capsular spread.
If malignant orbital invasion is diagnosed, it is appropriate to collaborate with a multidisciplinary team in planning management. An oncologist should be involved and also other disciplines according to the extent and direction of tumour invasion. Radical surgery and adjuvant radiotherapy or chemotherapy may be needed in such cases. Occasionally, surgery is not the best management at least as the initial treatment to contemplate and this can be decided jointly [15]. The surgery is performed in an attempt to achieve cure with tumour free margins. Malignancies of the ocular adnexa viz., SCC, SGC and BCC are the most prevalent causes of orbital exenteration [26,27]. Other less common cancers include conjunctival malignant melanoma, adenoid cystic carcinoma of the lacrimal gland and uveal melanoma with extrascleral extension [28].
Conclusion
Diagnosis and treatment of eyelid tumours is not always simple but quite challenging. The recognition and treatment of malignant eyelid tumours pose a challenge to even experienced oncologists and ophthalmologists and the wide range of clinical presentations along with several benign and malignant conditions affecting the ocular and periocular area, which mimic each other, contribute to a high risk of misdiagnosis and consequent suboptimal treatment. Each tumour is unique in its biologic behaviour and extent and management is necessarily tailored to fit that. Late diagnosis of tumours leads to more invasive surgery and consequently will have adverse functional and aesthetic effects. The cases described here exemplify this scenario.
[1]. Bedrossian EH, Embryology and anatomy of the eyelid. In: Tasman W, Jaeger EA, editorsDuane’s Foundation of Clinical Ophthalmology, Ocular Anatomy, Embryology and Teratology 2004 1:1-24. [Google Scholar]
[2]. Domingo RED, Manganip LE, Castro RM, Tumours of the eye and ocular adnexa at the Philippine Eye Research Institute: a 10-year reviewClin Ophthalmol 2015 9:1239-47. [Google Scholar]
[3]. Campbell RJ, Sobin LH, Tumours of the eyelidIn: World Health Organization International Histological Classification of Tumours 1998 2nd edBerlinSpringer:3-9. [Google Scholar]
[4]. Pe’er J, Eyelid tumours: Classification and differential diagnosis. In: Pe’er J, Singh AD, editorsClinical Ophthalmic Oncology: Eyelid and Conjunctival Tumours. 2nd ed. Ch. 2 2014 BerlinSpringer:9-10. [Google Scholar]
[5]. Pe’er J, Pathology of eyelid tumoursIndian J Ophthalmol 2016 64(3):177-90. [Google Scholar]
[6]. Herwig MC, Loeffler KU, Adnexal tumours. In: Pe’er J, Singh AD, editorsClinical Ophthalmic Oncology: Eyelid and Conjunctival Tumours. 2nd ed., Ch. 37 2014 BerlinSpringer:63-8. [Google Scholar]
[7]. Kersten RC, Ewing-Chow D, Kulwin DR, Gallon M, Accuracy of clinical diagnosis of cutaneous eyelid lesionsOphthalmology 1997 104(3):479-84. [Google Scholar]
[8]. Coroi MC, Roşca E, Muţiu G, Coroi T, Bonta M, Eyelid tumours:Histopathological and clinical study performed in County Hospital of Oradea between 2000-2007Rom J Morphol Embryol 2010 51(1):111-15. [Google Scholar]
[9]. Cook BE Jr, Bartley GB, Epidemiologic characteristics and clinical course of patients with malignant eyelid tumours in an incidence cohort in Olmsted County, MinnesotaOphthalmology 1999 106(4):746-50. [Google Scholar]
[10]. Wang JK, Liao SL, Jou JR, Lai PC, Kao SC, Hou PK, Malignant eyelid tumours in TaiwanEye (Lond) 2003 17(2):216-20. [Google Scholar]
[11]. Lee SB, Saw SM, Au Eong KG, Chan TK, Lee HP, Incidence of eyelid cancers in Singapore from 1968-1995Br J Ophthalmol 1999 83(5):595-97. [Google Scholar]
[12]. Nagaraju G, Chinmayee JT, Natarajan M, Vanitha MD, Squamous Cell Carcinoma of Eyelid Masquerading as Basal Cell CarcinomaJournal of Evidence based Medicine and Healthcare 2015 2(16):2456-59. [Google Scholar]
[13]. Shields JA, Demirci H, Marr BP, Eagle RC Jr, Shields CL, Sebaceous carcinoma of the ocular region: A reviewSurv Ophthalmol 2005 50(2):103-22. [Google Scholar]
[14]. Lober CW, Fenske NA, Basal cell, squamous cell, and sebaceous gland carcinomas of the periorbital regionJ Am Acad Dermatol 1991 25(4):685-90. [Google Scholar]
[15]. Tyers AG, Orbital exenteration for invasive skin tumoursEye (Lond) 2006 20(10):1165-70. [Google Scholar]
[16]. Nelson BR, Hamlet KR, Gillard M, Railan D, Johnson TM, Sebaceous carcinomaJ Am Acad Dermatol 1995 33(1):1-15.J Am Acad Dermatol. 1995;33(1):1-15; quiz 16-8 [Google Scholar]
[17]. Burns SJ, Foss AJ, Butler TK, Outcome of periocular sebaceous gland carcinomaOphthal Plast Reconstr Surg 2005 21(5):353-55. [Google Scholar]
[18]. Wali UK, Al-Mujaini A, Sebaceous gland carcinoma of the eyelidOman J Ophthalmol 2010 3(3):117-21. [Google Scholar]
[19]. Wolf DJ, Zitelli JA, Surgical Margins for Basal Cell CarcinomaArch Dermatol 1987 123(3):340-44. [Google Scholar]
[20]. Kimyai-Asadi A, Alam M, Goldberg LH, Peterson SR, Silapunt S, Jih MH, Efficacy of narrow-margin excision of well-demarcated primary facial basal cell carcinomasJ Am Acad Dermatol 2005 53(3):464-68. [Google Scholar]
[21]. Gündüz K, Demirel S, Günalp I, Polat B, Surgical approaches used in the reconstruction of the eyelids after excision of malignant tumoursAnn Ophthalmol (Skokie) 2006 38(3):207-12. [Google Scholar]
[22]. Cook BE Jr, Bartley GB, Treatment options and future prospects for the management of eyelid malignancies: An evidence-based updateOphthalmology 2001 108(11):2088-98.quiz 2099-100, 2121 [Google Scholar]
[23]. Yoon JS, Kim SH, Lee CS, Lew H, Lee SY, Clinicopathological analysis of periocular sebaceous gland carcinomaOphthalmologica 2007 221(5):331-39. [Google Scholar]
[24]. Lisman RD, Jakobiec FA, Small P, Sebaceous carcinoma of the eyelidsThe role of adjunctive cryotherapy in the management of conjunctival pagetoid spread. Ophthalmology 1989 96(7):1021-26. [Google Scholar]
[25]. Shields CL, Naseripour M, Shields JA, Eagle RC Jr, Topical mitomycin-C for pagetoid invasion of the conjunctiva by eyelid sebaceous gland carcinomaOphthalmology 2002 109(11):2129-33. [Google Scholar]
[26]. Ben Simon GJ, Schwarcz RM, Douglas R, Fiaschetti D, Orbital exenteration: one size does not fit allAm J Ophthalmol 2005 139(1):11-17. [Google Scholar]
[27]. Rathbun JE, Beard C, Quickert MH, Evaluation of 48 cases of orbital exenterationAm J Ophthalmol 1971 72(1):191-99. [Google Scholar]
[28]. Pushker N, Kashyap S, Balasubramanya R, Bajaj MS, Sen S, Betharia SM, Pattern of orbital exenteration in a tertiary eye care centre in IndiaClin Experiment Ophthalmol 2004 32(1):51-4. [Google Scholar]