Portal Venous Thrombosis: Eosinophilic Vasculitis
Vasanthi Natarajan1, David Jose2, Kevin John3, Ashok Kumar Das4
1 Assistant Professor, Department of Internal Medicine/Endocrinology, Pondicherry Institute of Medical Sciences, Puducherry, India.
2 Assistant Professor, Department of Internal Medicine, Pondicherry Institute of Medical Sciences, Puducherry, India.
3 Senior Resident, Department of Internal Medicine, Pondicherry Institute of Medical Sciences, Puducherry, India.
4 Professor, Department of Internal Medicine/Endocrinology, Pondicherry Institute of Medical Sciences, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vasanthi Natarajan, PIMS, Kalapet, Kanagachetikulam, Puducherry, India.
E-mail: vasanthikarthi2004@yahoo.co.in
Portal Vein Thrombosis (PVT) is caused by various thrombophilic states. PVT secondary to underlying vasculitis especially Churg-Strauss disease is among the rarest presentation. Here, we report a case of peripheral eosinophilia, eosinophilic ascitis and venous thrombosis involving portal vein and superior mesenteric vein diagnosed as Churg-Strauss Syndrome (CSS). He was managed with steroids and anticoagulants. Following initiation of steroids, eosinophilia and eosinophilic ascitis improved.
Churg-Strauss disease, Eosinophilic ascitis, Peripheral eosinophilia
Case Report
A 48-year-old male presented to medicine outpatient department with abdominal distension of one month duration, which was progressive and worsened in the last one week. He did not take any treatment at this stage. There was also history of fever with thrombocytopenia (which was documented in the previous blood investigation report) one week back and treated conservatively for the same. There was no history of any bleeding manifestations. The patient also complained of weight loss which was not quantifiable, associated with decreased appetite for last one month. He used to take alcohol for last 10 years occasionally but never smoked. On examination, his vitals were stable. Abdomen examination showed diffuse distension of the abdomen with free fluid and there were dilated veins over the abdominal wall. Rectal examination was normal. Respiratory system examination showed bilateral occasional rhonchi. Other system examination was normal.
His blood investigation revealed eosinophilia and thrombocytopenia. Total count- 18,100 cells/cumm with neutrophils-46%, lymphocytes-18%, eosinophils-35%, platelets-13000 cells/cumm, absolute eosinophil count-6330/μl, ESR-10 mm/hr, IgE (ELISA)-312 (normal-2.0-305.9 IU/ml). Diagnostic ascitic fluid tapping was done, which showed eosinophilic ascitis with a total count of 270 cells, differential count of polymorphs 12%, lymphocytes 60%, eosinophils 28%. Serum Ascitis Albumin Gradient (SAAG) was high, suggestive of portal hypertension. Liver function test showed elevated liver enzymes (SGOT-407 u/l, SGPT-1250 u/l). Hepatitis B and C virus serology was negative. Prothrombin time- Patient/Control-17.9/11.5, INR was 1.5. X-ray chest was normal. A 2D echocardiography showed normal left ventricular function.
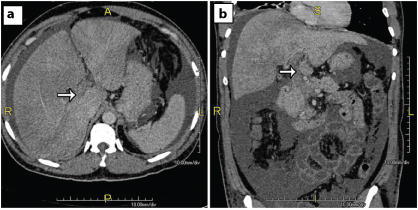
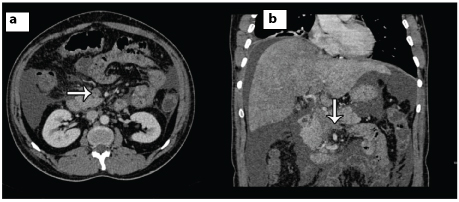
Ultrasound of the abdomen showed moderate ascitis, minimal right-sided pleural effusion with the suspicion of PVT. He then underwent Computed Tomography (CT) of abdomen with contrast, which showed portal vein [Table/Fig-1], superior mesenteric vein thrombosis [Table/Fig-2]. CT thorax showed thrombosis involving right lower territory of pulmonary vein. With this presentation of peripheral eosinophilia, eosinophilic ascitis and venous thrombosis, we considered eosinophilic granulomatosis with polyangitis- Churg-Strauss disease. His vasculitic work up c ANCA, p ANCA, ANA (ELISA, Indirect Immunofluorescence) including anti phospholipid antibody were negative with normal complements. Serum homocysteine level was normal. As we suspected CSS, retrospectively we confirmed the history of allergy to dust and fumes and recurrent breathlessness. He used to get treatment with inhaled bronchodilators and Tab. Deriphyllin for the same at local place. He was treated with Inj. Dexamethasone 6 mg thrice daily followed by oral tapering dose of prednisolone 1 mg/kg/day. Following initiation of steroids his peripheral eosinophilia and eosinophilic ascitis improved. He felt better and abdominal distention decreased. Inj.low molecular weight heparin followed by oral anticoagulants (Tab.Warfarin 3 mg daily) was started once his platelet count improved. The patient came after eight days then lost follow up.
Computed tomography of abdomen with contrast axial a); Coronal view b) Shows portal vein thrombosis (white arrow).
Computed tomography of abdomen with contrast axial view a); and Coronal; b) View shows superior mesenteric vein thrombosis (white arrow).
Discussion
CSS is a vasculitis involving small and medium sized vessels [1]. It presents with history of allergy, asthma, peripheral eosinophilia with pulmonary infiltrates. Extra pulmonary manifestations of CSS include cardio vascular, renal, gastrointestinal, peripheral nervous system and dermatological involvement. Gastrointestinal manifestation of CSS can produce bowel ischemia, perforation and bleeding. Gastric involvement with portal vein thrombosis leading to portal hypertension is rarely reported in literature.
CSS clinically present in three phases-prodromal, eosinophilic and vasculitic phase. In eosinophilic phase, there will be eosinophilic infiltration of major organs. In vasculitic phase, cardiac and gastrointestinal manifestation is more, which has got high mortality [1]. Allenbach Y et al., has reported that among all vasculitis, wegeners granulomatosis, CSS and microscopic polyangitis has increased risk of getting venous thrombosis [2].
The diagnosis of CSS is based on two common criteria, which includes American College of Rheumatology (ACR) criteria and Lanham criteria. The ACR criteria include: 1) asthma; 2) peripheral eosinophilia; 3) mononeuropathy multiplex, polyneuropathy; 4) X-ray features of pulmonary opacities; 5) Paranasal sinus involvement; 6) eosinophilic infiltration of vessels in biopsy. The presence of four or more among these has a sensitivity of 85% in diagnosing CSS [3].
In the Lanham criteria, there should be all the three factors, which includes asthma, peripheral eosinophilia >1500 cells/cumm, systemic vasculitis involving two or more extrapulmonary organs [4]. Our patient had history of asthma, peripheral eosinophilia, venous thrombosis involving portal vein and superior mesenteric vein - fulfilling the Lanham criteria, hence, diagnosed as Churg Strauss disease. In CSS 40% of patients present with ANCA positivity and remaining are ANCA negative [5]. CSS with kidney, peripheral nervous system involvement and vasculitic phase of the disease predominantly present with ANCA positivity at diagnosis. ANCA negativity predominantly indicates cardiac involvement. Suspicion of eosinophilic vasculitis is confirmed either by laboratory methods or histopathological examination. Biopsy of involved organ can present with necrotizing vasculitis, tissue eosinophilia and extra vascular granuloma. Solans R et al., has reported that 23% of normal histopathology in CSS patients [6]. Even without asthma and peripheral eosinophilia cases with Churg Strauss disease has been reported [7].
Eosinophilic gastroenteritis can present with diarrhoea, ascitis, haemorrhage and perforation. It is classified as mucosal, muscular and subserosal type. The clinical features depend on the extent of involvement. Ascitis occurs in subserosal involvement of eosinophilic gastroenteritis. Eosinophilic ascitis with mesenteric thrombosis causing occlusion is very rarely reported. Eosinophilic ascitis with peripheral eosinophilia is usually treated with steroids, which has good prognosis [8]. But in the presence of significant venous thrombosis as in our patient with the suspicion of vasculitis warrants anticoagulants along with steroids.
Prothrombotic causes accounts for almost 50% of non cirrhotic PVT [9]. Various thrombophilic states and post surgical causes have been described to cause PVT. Complete venous occlusion of portal vein and its extension into the superior mesenteric vein may cause bowel ischemia and gangrene, which needs early intervention.
Conclusion
Vascular thrombosis involving portal and superior mesenteric vein thrombosis with eosinophilic ascitis and peripheral eosinophilia secondary to vasculitis is one of the rarest manifestations of CSS. Early recognition and management with steroids and anticoagulants is important to prevent dreaded complication like bowel ischemia.
[1]. Guillevin L, Cohen P, Gayraud M, Lhote F, Jarrousse B, Casassus P, Churg-Strauss syndrome. Clinical study and long-term follow-up of 96 patientsMedicine 1999 78(1):26-37. [Google Scholar]
[2]. Allenbach Y, Seror R, Pagnoux C, Teixeira L, Guilpain P, Guillevin L, High frequency of venous thromboembolic events in Churg-Strauss syndrome, Wegener’s granulomatosis and microscopic polyangiitis but not polyarteritis nodosa: a systematic retrospective study on 1130 patientsAnn Rheum Dis 2009 68(4):564-67. [Google Scholar]
[3]. Masi AT, Hunder GG, Lie JT, Michel BA, Bloch DA, Arend WP, The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndromeArthritis Rheum 1990 33(8):1094 [Google Scholar]
[4]. Lanham JG, Elkon KB, Pusey CD, Hughes GR, Systemic vasculitis with asthma and eosinophilia: a clinical approach to the Churg-Strauss syndromeMedicine 1984 63(2):65 [Google Scholar]
[5]. Sablé-Fourtassou R, Cohen P, Mahr A, Pagnoux C, Mouthon L, Jayne D, Antineutrophil cytoplasmic antibodies and the Churg–Strauss syndromeAnn Intern Med 2005 143:632-38. [Google Scholar]
[6]. Solans R, Bosch JA, Pérez-Bocanegra C, Selva A, Huguet P, Alijotas J, Churg-Strauss syndrome: outcome and long-term follow-up of 32 patientsRheumatology (Oxford) 2001 40(7):763-71. [Google Scholar]
[7]. Sharma BK, Daga MK, Sharma MA, Limited form of Churg-Strauss syndrome presenting without asthma and eosinophiliaMed J Aust 2004 181(9):498-99. [Google Scholar]
[8]. Alsulaiman RM, Eosinophilic ascites:A case report and literature reviewJ Fam Community Med 2015 22:183-85. [Google Scholar]
[9]. Hillaire S, Bonte E, Denninger MH, Casadevall N, Cadranel JF, Lebrec D, Idiopathic non-cirrhotic intrahepatic portal hypertension in the West: a re-evaluation in 28 patientsGut 2002 51(2):275 [Google Scholar]