Giant Leiomyoma of the Oesophagus
Dhamodaran Kandasamy1, Niyas Ahamed2, Sujatha Kannan3, Vasundaran Samuel4
1 Professor, Department of Cardiothoracic Surgery, Government Stanley Medical College, Chennai, India.
2 Postgraduate, Department of General Surgery, Government Stanley Medical College, Chennai, India.
3 Associate Professor, Department of Anatomy, Government Stanley Medical College, Chennai, India.
4 Assistant Professor, Department of Cardiothoracic Surgery, Government Stanley Medical College, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Niyas Ahamed, 93, EB Colony, Khajamalai, Trichy-620023, Tamil Nadu, India.
E-mail: niyasdr@yahoo.co.in
Leiomyomas are rare benign tumours of the oesophagus that remain silent in more than 50% of the cases. Giant leiomyomas measuring more than 5 cm are very rare. A 47-year-old female presented with chest pain, cough and dysphagia for two months. Imaging studies were indicative of a 12.1x11.9 cm mass lesion in the distal oesophagus, CT guided biopsy confirmed leiomyoma. The patient being taken up for surgery was found to have a 20x19x17 cm irregular lobulated and encapsulated mass lesion arising from distal oesophagus encapsulating submucosally. En bloc resection of the tumour along with distal oesophagus with a clearance of 4 cm above and below the oesophagogastric junction was done followed by gastro-oesophageal anastomosis. Histopathologically, leiomyoma was confirmed. The patient had a smooth postoperative recovery.
Benign tumour, Oesophageal leiomyoma, Resection
Case Report
A 47-year-old female post-hysterectomy patient presented with complaints of cough with expectoration, chest pain and dysphagia to solid foods with regurgitation for two months. The patient underwent hysterectomy 15 years back for dysfunctional uterine bleeding, details of which could not be traced. She underwent thoracotomy 10 years back for excision of a left bronchial carcinoid. Her son died of similar illness at the age of 17 that went undiagnosed.
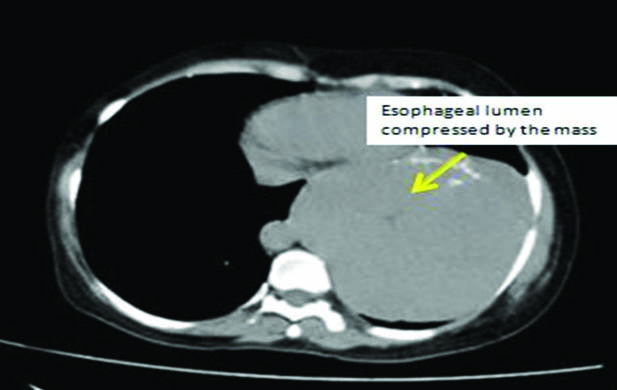
The clinical examination being inconclusive, we proceeded with the investigations. Barium meal study showed an irregular circumferential mass of distal oesophagus with involvement of oesophagogastric junction and no filling defect. USG abdomen showed a heteroechoic mass lesion measuring 12.1x11.9 cm, superior to the spleen. CECT chest revealed large exophytic, hypodense, extrinsic mass lesion arising from oesophagus measuring 11.5x11.5 cm [Table/Fig-1]. Endoscopy showed a submucosal lesion 28-32 cm from the central incisors. CT guided biopsy was taken which revealed a possibility of leiomyoma of vascular origin. After the initial workup, we proceeded for surgery.
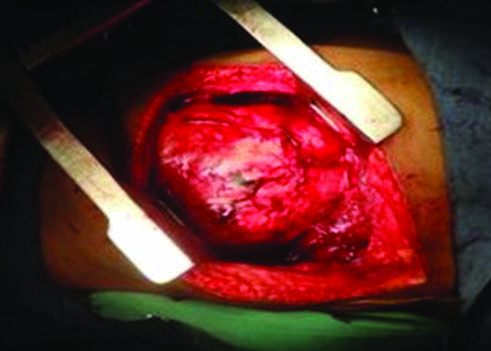
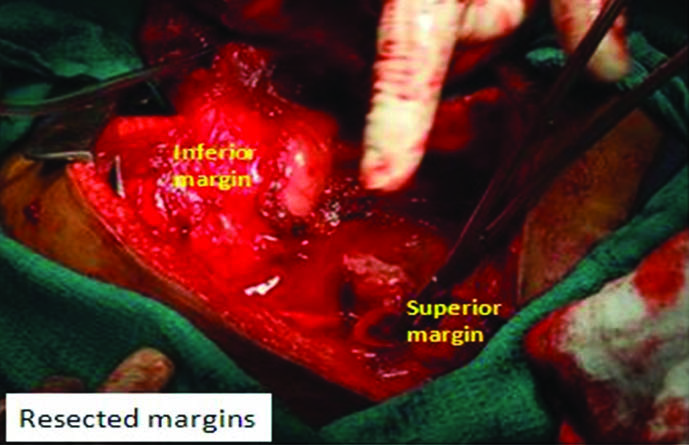
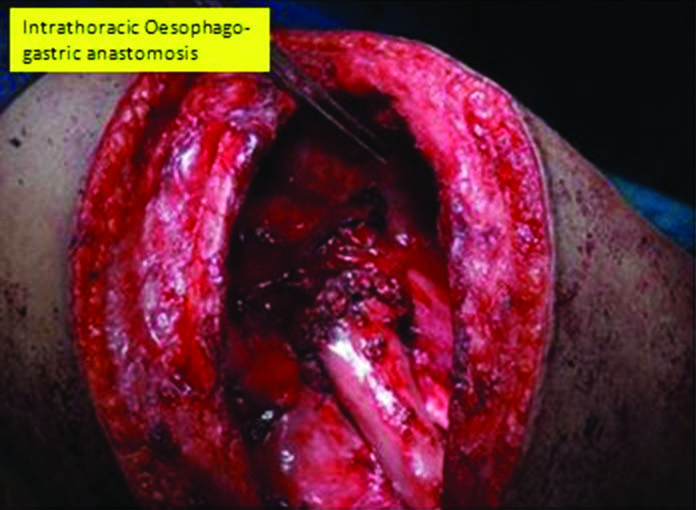
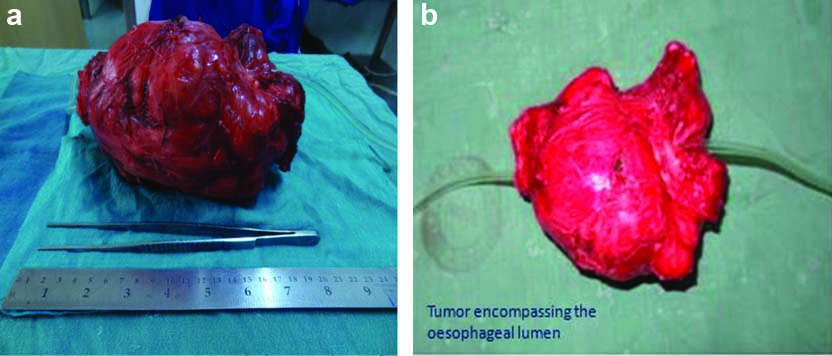
Diagnostic laparoscopy was performed to rule out intra-abdominal pathologies, following which a left posterolateral thoracotomy was done at 7th intercostal space. A 20x19x17 cm irregular lobulated and encapsulated mass lesion, occupying left hemithorax, arising from distal oesophagus, was found involving the oesophagogastric junction encircling submucosally [Table/Fig-2]. Stomach was normal. The lesion was dissected free from the left lung, descending aorta and pericardium. The tumour being large and encompassing oesophageal lumen, en bloc resection was done along with distal oesophagus with a clearance of 4 cm proximally and distally [Table/Fig-3]. Primary intrathoracic oesophago-gatric anastomosis was performed end to end with 2’0 vicryl [Table/Fig-4]. The tumour weighed 1.2 kg [Table/Fig-5]. Decortication of the left lung was done; diaphragm was repaired with 1’0 prolene. Feeding jejunostomy was done for postoperative nutrition.
Tumour in the thoracic cavity.
Perioperative image showing the resected margins.
Primary intrathoracic oesophago-gatric anastomosis.
(a,b) The excised specimen.
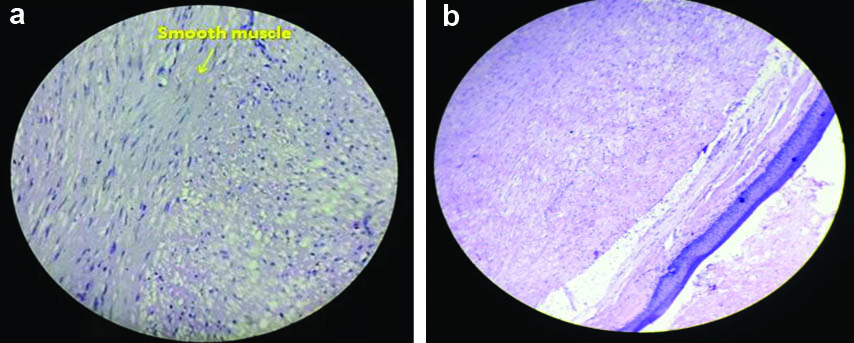
The patient was in ICU care for two days. Intercostal drain was removed and oral feeds were initiated on postoperative day 6 and 8 respectively. Postoperative period was uneventful for the patient, with no leak in the barium meal study done on 8th postoperative day [Table/Fig-6]. Histopathology report confirmed the presence of benign leiyomyoma [Table/Fig-7] with Immunohistochemical (IHC) markers positive for Desmin and smooth muscle actin. The patient is on regular follow up for the past two years and is asymptomatic till now.
Postoperative barium meal study.

(a,b) Histopathology - Leiomyoma.
Discussion
Benign tumours of the oesophagus are rare and constitute <1% of oesophageal neoplasms [1]. About two-thirds of the oesophageal benign tumours are Leiomyoma’s making it the most common benign tumour.
Leiomyomas of the oesophagus arise from smooth muscle of which 60% arise in the distal third [2]. Usually, leiomyomas grow from 2 to 5 cm in diameter, although tumours of several millimeters to 22 cm in length have also been reported [3]. Tumours larger than 5 cm are rare. It is the clinical presentation and management that differentiates them from other smaller leiomyoma. Those tumours weighing more than 1000 g are termed as giant tumours [3]. They are asymptomatic in more than half of the patients. Dysphagia and retrosternal pain develops when the tumour diameter is >5cm [4]. Since leiomyomas grow extramurally, dysphagia is not often proportional to the size of the tumour. The larger the tumour i.e., >5 cm, it is associated with muscle atrophy and more muscular defects. It may present as a mediastinal mass on chest X-ray [2].
Differential diagnosis includes malignancies such as squamous/adenomatous carcinoma and leiomyosarcoma. Barium study is the investigation of choice wherein it demonstrates a smooth filling defect in the lumen without mucosal abnormality [5]. CECT chest reveals the exact location, size, extent, and vascularity of the tumour. On Endoscopic Ultrasound (EUS), leiomyoma appears as a homogenous, hypoechoic lesion surrounded by a hyperechoic region [6]. Preoperative biopsy remains a controversy.
Although malignant transformation is very rare, surgery remains the mainstay of treatment. Endoscopic Mucosal Resection (EMR) is preferred for tumours that are 2-4 cm in length [7]. In leiomyoma, tumour size and location determines the nature of surgery. Right lateral thoracotomy is carried out for tumours occupying middle third of oesophagus whereas left lateral approach is considered for lower third tumours. Enucleation is the procedure done routinely.
Minimally invasive surgery is possible in tumours less than 5 cm, although some authors suggest that tumours sized even up to 8 cm can be resectable during thoracoscopy [8]. Regular follow up with barium swallow is essential in tumours less than 5 cm as malignant transformation is rare [1,9]. For giant oesophageal leiomyoma, oesophageal resection and reconstruction is preferred rather than conventional enucleation of tumour because: (i) of the technical difficulty; (ii) poor wound healing in the defect of oesophageal muscle that has become thin and membranous following pressure; (iii) lower oesophageal sphincter dysfunction or loss following enucleation [10,11].
Conclusion
Leiomyoma, a benign neoplasm of the oesophagus, poses a serious diagnostic and therapeutic challenge. Precise preparation for the surgery is essential for lesions sized over 8-10 cm, as resection of the oesophagus may be necessary. Once the diagnosis of oesophageal leiomyoma is established, a tailor-made surgical approach should be applied based on the size and location of the tumour.
[1]. Punpale A, Rangole A, Bhambhani N, Karimundackal G, Desai N, de Souza A, Leiomyoma of oesophagusAnn Thorac Cardiovasc Surg 2007 13:78-81. [Google Scholar]
[2]. Peters JH, DeMeester TR, Oesophagus and diaphragmatic hernia. In: Brunicardi FC, Andersen KD, Billiar RT, Dunn LD, Hunter GC, Pollock RE, edsSchwartz’s Principles of Surgery 2005 8th edNew YorkMcGraw-Hill:906 [Google Scholar]
[3]. Heitmiller FR, Brock VM, Benign Tumours and Cysts of the Oesophagus. In: Yeo JC, Peters HJ, edsShackelford’s Surgery of the Alimentary Tract 2013 7th edPhiladelphiaElsevier:465 [Google Scholar]
[4]. Chak A, EUS in submucosal tumoursGastrointest Endosc 2002 56:S43-48. [Google Scholar]
[5]. Sun X, Wang J, Yang G, Surgical treatment of oesophageal leiomyoma larger than 5 cm in diameter: A case report and review of the literatureJ Thorac Dis 2012 4(3):323-26. [Google Scholar]
[6]. Xu GQ, Zhang BL, Li YM, Chen LH, Ji F, Chen WX, Diagnostic value of endoscopic ultrasonography for gastrointestinal leiomyomaWorld J Gastroenterol 2003 9:2088-91. [Google Scholar]
[7]. Kajiyama T, Sakai M, Torii A, Kishimoto H, Kin G, Uose S, Endoscopic aspiration lumpectomy of oesophageal leiomyomas derived from the muscularis mucosaeAm J Gastroenterol 1995 90:417-22. [Google Scholar]
[8]. Kent M, d’Amato T, Nordman C, Schuchert M, Landreneau R, Alvelo-Rivera M, Minimally invasive resection of benign oesophageal tumoursJ Thorac Cardiovasc Surg 2007 134:176-81. [Google Scholar]
[9]. Priego P, Lobo E, Alonso N, Gil Olarte MA, Pérez de Oteyza J, Fresneda V, Surgical treatment of oesophageal leiomyoma: An analysis of our experienceRev Esp Enferm Dig 2006 98:350-58. [Google Scholar]
[10]. Sabbah F, Oudanane M, Ehirchiou A, Raiss M, Hrora A, Benamer A, Leiomyoma of the oesophagusPresse Med 2001 30:1148-50. [Google Scholar]
[11]. O’Hanlon DM, Clarke E, Lennon J, Gorey TF, Leiomyoma of the oesophagusAm J Surg 2002 184:168-69. [Google Scholar]