Dexmedetomidine is the active d-isomer of medetomidine, which is a selective and specific α2-adrenoceptor agonist [1]. It acts by the central sympatholytic action, thereby providing haemodynamic stability. It has both analgesic as well as anaesthetic sparing property [2]. Dexmedetomidine is also a potent sedative [3,4].
At the time of laparoscopy, endotracheal intubation and time of extubation are most critical events which provoke transient, but marked sympatho-adrenal response such as tachycardia and hypertension. Also, Carbon dioxide (CO2) used for creating pneumoperitoneum at the time of surgery, causes spikes in plasma levels of catecholamine and vasopressin. This leads to rise in intra-abdominal pressure due to raised diaphragm which leads to side effects on the CVS such as low cardiac output, rise in arterial pressure and increase systemic and pulmonary vascular resistance, leading to hypertension and tachycardia [4].
This study aimed at assessing the effect of intravenous dexmedetomidine and fentanyl on perioperative haemodynamics and recovery during postoperative period following elective laparoscopic surgical procedures.
Materials and Methods
A double blinded randomized controlled study was done for the patients operated between June 2014- May 2016 at Sterling Hospital, Ahmedabad, Gujarat, India.
Sixty patients, aged 18-60 years, with American Society Anesthesiologists (ASA) status I and II who were undergoing elective laproscopic surgery were selected for this study. Approval for the study was taken from the Institutional Ethics Committee and written informed consent was obtained in local language.
These patients were randomly allotted into two groups: Group F (fentanyl) and Group D (dexmedetomidine). Patients with age more than 60 years and those with any significant history of psychiatric/neurological illness, hypertensive patients, those who have known allergic reaction, and those patients with gross abnormalities in laboratory investigations were excluded from the study.
Vital data like Pulse, Blood Pressure (BP), Electrocardiogram (ECG) and Peripheral Capillary Oxygen Saturation (SPO2) were recorded after shifting patient to the operating room. All patients were given premedication in the form of Inj. glycopyrollate-0.004 mg/kg and Inj. ondensetron-0.08 mg/kg.
The prepared drug dexmedetomidine or fentanyl (conc. 4μg/ml) was administered IV over 10 minutes prior to induction of anaesthesia, in Group D (n = 30), intravenous dexmedetomidine 0.5 μg/kg as loading dose over 10 minutes prior to induction followed by 0.2-0.7 μg/kg/hr till surgery was over and in Group F (n = 30), intravenous fentanyl 0.5 μg/kg as loading dose over 10 minutes prior to induction followed by 0.2 μg/kg/hr-0.7 μg/kg/hr till surgery was over.
Ten minutes after infusion of drug dexmedetomidine or fentanyl, the parameters ECG, HR, Resperatiory Rate (RR), SBP, DBP, Mean Arterial Pressure (MAP), SpO2 were recorded. The sedation was evaluated after the infusion of study drug dexmedetomidine or fentanyl according to modified Ramsay sedation score.
All the patients of Group D and Group F were induced with Inj. sodium thiopental 5mg/kg-7mg/kg IV and Inj. succinylcholine 1.5mg/kg-2mg/kg IV. All the patients were intubated with cuffed endotracheal tube of appropriate size. Patients of both the groups were maintained with O2+N2O+ sevoflurane (1.5-2%) + Inj. atracurium 0.4 mg/kg to 0.5 mg/kg and maintenance dose of 0.08 mg/kg to 0.10 mg/kg intermittently.
Intraoperatively the following parameters were monitored: Continuous ECG, HR, SBP, DBP, Mean Arterial Presssure (MAP), SpO2 and ETCO2. Infusion of drug (dexmedetomidine or fentanyl) was stopped and sevoflurane was discontinued 10 minute before reversal. Residual paralysis was reversed with Inj. neostigmine 0.05 mg/kg IV, + Inj. glycopyrrolate 8μg/kg IV. The patients were extubated after adequate reversal of muscle relaxant adjudged by adequate spontaneous breathing and limb movement, return of consciousness and obeying of verbal command. The patients were then shifted to postoperative recovery room for observation and further management.
The above parameters were recorded at predetermined time intervals: prior to infusion of drugs (dexmedetomidine/fentanyl), immediately after the drugs, after injection of induction drugs, five mins after intubation just after pneumoperitoneum, during pneumoperitoneum (5,10,15,30,45,60 minutes), five minutes after release of pneumoperitoneum, five and 10 minutes after extubation.
Adverse effect like bradycardia, tachycardia, hypotension, hypertension, nausea, vomiting, respiratory depression, if any noted during operative procedure were treated as follows-Bradycardia- (HR<55/min): Inj. glycopyrolate 0.2 mg IV.; tachycardia- (HR> 30% above baseline value): Inj. propofol 20 mg IV in titrated dose; hypotension- (SBP<60 mmHg): Inj. ephedrine 6 mg IV in titrated dose; hypertension- (SBP>140 mmHg): Inj. propofol 20 mg IV in titrated dose and increasing concentration of isoflurane upto 1.2%. Amount of rescue analgesia during intraoperative period by IV propofol was noted.
Postoperatively, the sedation was determined by modified Ramsay sedation score. The score consists of the following six grades:
1 = Anxious or agitated and restless or both;
2 = Cooperative, oriented and tranquil;
3 = Drowsy but responds to commands;
4 = Asleep, brisk response to light glabellar tap or loud auditory stimulus;
5 = Asleep, sluggish response to light glabellar tap or loud auditory stimulus;
6 = Asleep and unarousable.
Sedation score greater than 3 was considered as undesirable. Patient was shifted out of recovery room after score of less than or equal to 3 was observed.
The results were expressed as number of occurrences, percentage (%) and mean±SD. Demographic characteristics, preoperative vitals were compared using student’s t-test and nominal data were compared with chi-square test. Repeated measures of analysis of variance (RMANOVA) was used to compare continuous variables. Statistical analysis was performed using GRAPH. PAD INSTAT Software Package. A p-value of less than 0.05 was considered statistically significant.
Results
The groups, Group D and Group F, were found to be comparable with regarding age, sex, weight and ASA physical status. The surgical intervention included the patients operated for laparoscopic cholecystectomy and laparoscopic appendectomy was included in study. Both groups were found to be comparable to each other. The duration of anaesthesia (p>0.05) was found to be comparable with each other. Pre-induction HR (p=0.240), SBP (p=0.173) and DBP (p=0.774) were all comparable to each groups.
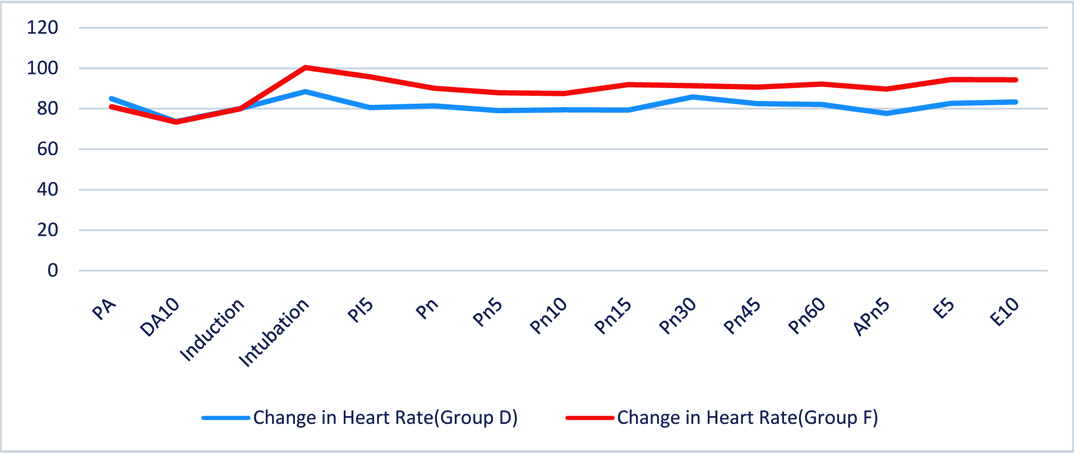
In Group D the heart rate did not rise significantly and remained relatively stable around baseline throughout the study period except at laryngoscopy where it showed marginal rise. In Group F the heart rate fell below baseline after injection of fentanyl and inducing drug, then increased after laryngoscopy and continued to remain on higher side throughout the period of study. Ten minutes after the test drug, the difference of heart rate was not statistically significant as p-value is 0.951. After intubation there was 5% rise in heart rate from baseline in Group D ascompared to 18% rise in Group F (p=0.001) which is significant. After creation of pneumoperitoneum heart rate in Group D decreased by 3.51% compared to 11.11% rise in Group F from baseline which is statistically significant (p=0.012). Intraoperatively, throughout the period of pneumoperitoneum, Group D showed significantly fall in heart rate from baseline at all time points, whereas in Group F the heart rate constantly remained above the baseline throughout the intra operative period and the difference between two group is statistically significant as p-value is less than 0.05 at all time points.
Post extubation at five minutes and 10 minutes in Group D mean heart rate fell by 2% from baseline, as compared to Group F which showed average 15% rise which is statistically significant (p=.002) [Table/Fig-1].
Changes in heart rate (beats/min).
PA-Pre Administration DA-Drug Administration
PI-Post Intubation Pn-Post Pneumothorax
Apn-After Pneumothorax E-Extubation
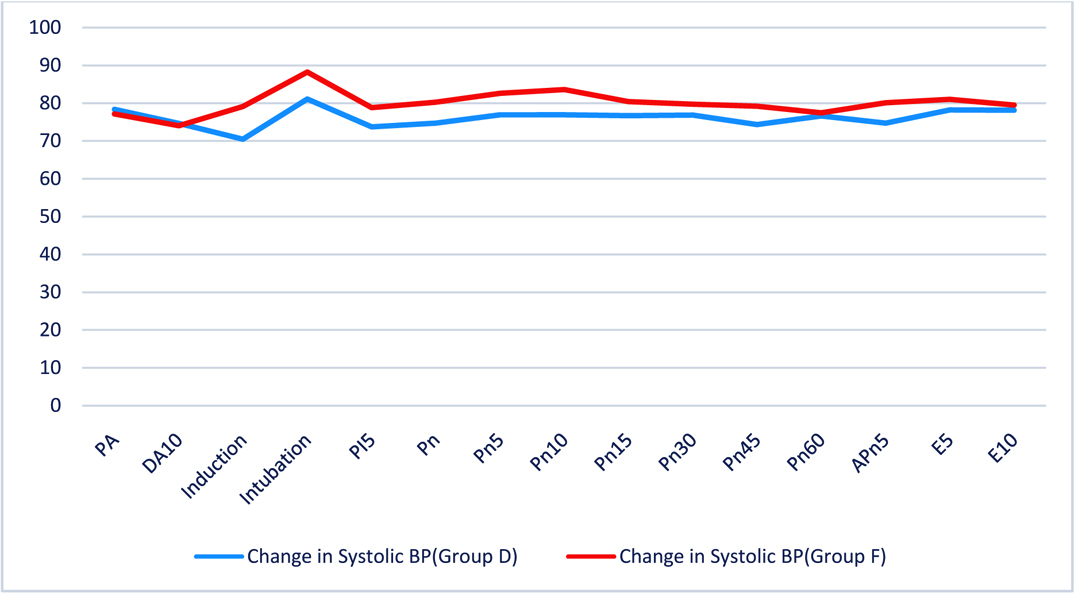
When SBP in Group D is compared with that of Group F it was observed that-Ten minutes after the test drug, there was 9% fall in SBP below baseline value in group D as compared to Group F where there is no fall of SBP (p=0.010) which is statistically significant. After intubation, both the groups showed rise in SBP. Group D showed a rise of 9%, but not above baseline, where as in group F there was 19% increase of SBP than baseline which is significant (p=0.001). After creation of pneumoperitoneum there was 8.8% fall in SBP in Group D as compared to 4.2% rise in Group F (p=0.006, statistically significant). In intraoperative period, throughout the period of pneumoperitoneum till release of pneumoperitoneum Group D showed significant fall in SBP from baseline as compared to Group F. At all time points that is at five minutes, 10 minutes, 45 minute after pneumoperitoneum and at five min after release of pneumoperitoneum, the difference between two groups was statistically significant with p-value less than 0.05. Post extubation at 10 minutes, change in SBP in both groups is not statistically significant (p=0.541) [Table/Fig-2].
Changes in systolic blood pressure (mm Hg).
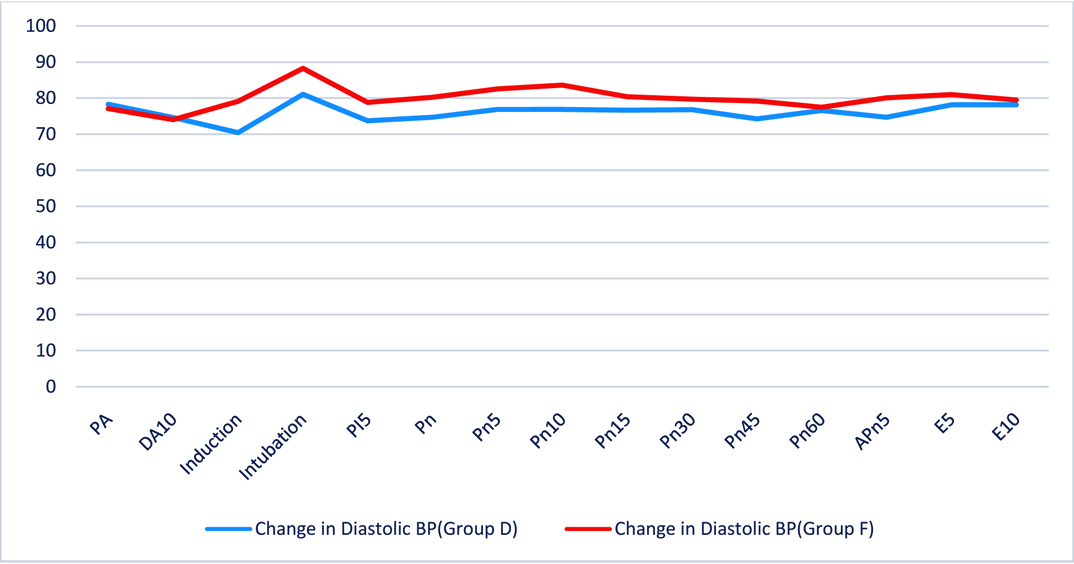
In Group D the DBP remained relatively stable below baseline at all time points. In Group F the DBP was significantly higher than the baseline value till the end of study. Ten minutes after the test drug, fall in DBP was not statistically significant (p=0.774). After intubation, both Group D & F showed rise in DBP by 3% & 15% respectively (p=0.027) which is statistically significant. After creation of pneumopritoneum, fall in DBP in both groups is not significant. In intraoperative period, throughout the period of pneumoperitoneum and after release of pneumo the DBP remained below baseline in Group D as compared to Group F where it remained constantly above baseline. There was significant difference between two groups at 10 minutes, at 45 minutes and after release of pneumoperitoneum as p-value is less than 0.05. Post extubation at five minutes DBP was not statistically significant (p=0.340) [Table/Fig-3].
Changes in diastolic blood pressure (mm Hg).
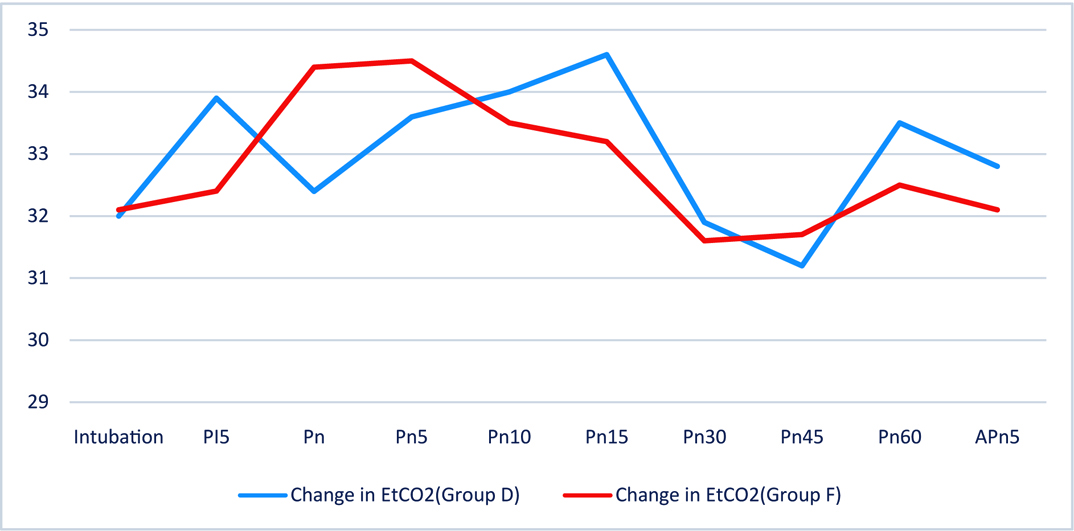
ETCO2 in Group D and Group F were comparable and difference was not significant [Table/Fig-4].
Postoperatively the mean duration of adequate analgesia was 81.3 minutes in Group D where as it was 41.9 minutes in Group F. The duration was much longer in Group D as compared to Group F with p-value=0.001, which is statistically significant.
Bradycardia was observed in two patients in the dexmedetomidine group within 10 min post extubation, which promptly responded to Inj. atropine 0.6 mg intravenous. The duration of recovery was similar in both the groups. After operation, none of the patients in either of the groups complained of any discomfort or of intraoperative awareness. No patients developed hypotension (SBP<60mmHg) in both Group D and Group F. Three (10%) patient developed intraoperative hypertension (SBP>140 mm Hg) in Group D where as 19 patients (63.3%) in Group F developed intraoperative hypertension. None of the patient in Group D had tachycardia (HR>30% above baseline) where as four patients (10%) in Group F developed tachycardia during intubation & perioperative period. Nausea & vomiting was found in two patients (6%) in Group D and three patients (10%) in Group F in postoperative period which were effectively treated. None of the patients in both groups have any respiratory depression. None of the patients in both groups developed any ECG abnormality. There was no significant difference in pre and intraoperative SpO2 and ETCO2 values.
Discussion
This study has demonstrated that use of dexmedetomidine for intraoperative infusion helps attenuates stress responses to different noxious stimuli during surgery and helps maintain haemodynamic stability and early recovery [5].
Dexmedetomidine, being a highly selective α2 agonist is sympatholytic and also has haemodynamic stability property [6]. It leads to dose-dependent decrease in heart rate and blood pressure [7]. Previous studies have shown that dexmedetomidine controls stress response to intubation by decreasing central sympathetic outflow, hence decreasing serum epinephrine and norepinephrine levels [8]. It stimulates receptors in the medullary vasomotor center, reducing norepinephrine turnover and controls central sympathetic outflow, resulting in alterations in sympathetic function, hence suppressing the haemodynamic response to intubation, extubation without any side effects like respiratory depression and Post operating Nausea and Vomiting (PONV). It leads to a dose dependent decrease of arterial BP and HR due to decrease in serum norepinephrine concentrations. Also, this is due to decrease in central stimulation of parasympathetic outflow and inhibition of sympathetic outflow from the brainstem- the locus coeruleus. Dexmedetomidine has shown blunting of cardiovascular response to intubation in many studies of patients undergoing general or gynaecological surgery. These findings are consistent with our study results which showed a significant decrease in change in HR, SBP and DBP [9,10].
Patients receiving high dosage led to postoperative bradycardia in as many as 40% patients in healthy surgical patients. Usually, these were temporary effects which could be treated successfully with atropine or epinephrine. HR and BP decreased in the study by Feld JM et al., who compared dexmedetomidine with fentanyl in bariatric surgery [11]. Tanskanen PE et al., showed that intraoperative infusion of dexmedetomidine maintains HR and BP in control for a longer duration as compared to placebo group [7]. Dexmedetomidine blunts the haemodynamic response during emergence from anaesthesia and extubation [8,10]. Our study showed a significant attenuation of HR at the time of extubation in dexmedetomidine group. Dexmedetomidine if used as the substitute for remifentanil in gynaecologic laparoscopic surgery, leads to better perioperative haemodynamic stability and postoperative analgesia [12].
Dexmedetomidine can lead to cardiovascular depression, causing, bradycardia and hypotension. Bradycardia is due to activation of alpha-2-adrenoceptors, imidazoline-preferring receptors or both in the ventrolateral medulla. Two patients in our study had bradycardia in the postoperative period, which is statistically insignificant. It may be attributed to the slow infusion of bolus in our patients. These results are similar to those of Bekker A et al., who had reported that dexmedetomidine, when given at a similar dose, was useful in blunting the increase in systolic BP perioperatively, even though no increase the incidence of hypotension or bradycardia was seen [13]. Hogue CW et al., reported dexmedetomidine maintains baroreflex sensitivity, maintaining the HR in response to fluctuation of BP. Slowing of the HR is mainly due to sympathetic withdrawal [14].
Hall JE et al., in their study concluded that small doses of dexmedetomidine led to significant sedation which could be reversed by the help of verbal or physical stimuli, and it resolved completely after two hour of termination of infusion [4]. In our study, no clinically significant sedation was seen in any patient though nine patient had sedation score ≤3 in Group D. In the study by Turan G et al., it was seen that cough, difficulty in breathing, laryngeal edema and bronchospasm did not happen with a single dose of dexmedetomidine [15]. Also, Gurbet A et al., in their study did not observe sedation in any patient who had received intraoperative dexmedetomidine infusion [2]. Mechanism of action of dexmedetomidine is a postsynaptic alpha-2-adrenoceptor located in the locus coeruleus [16]. Gurbet A et al., concluded that continuous intravenous dexmedetomidine while operating for abdominal surgery leads to effective postoperative analgesia and reduced postoperative need of morphine without any increase in the incidence of side effects [2]. In their study, Basar H et al., concluded that a single dose of 0.5 μg/kg of dexmedetomidine given during the preoperative period led to significant sedation with no limitation in recovery scores [17].
During the postoperative period, recovery and longer discharge time of patients from post anaesthesia recovery room receiving perioperative dexmedetomidine infusion. In their study, Massad IM et al., found that combining dexmedetomidine to other anaesthetic agents, leads to a balanced anaesthesia and a significant drop in the incidence of PONV postoperatively [18]. In our study there was no difference between both groups after two hours. This may be due to sedative property of dexmedetomidine [6]. However, sedation due to dexmedetomidine is rarely seen with respiratory depression.
Limitation
In our study, dexmedetomidine was stopped 20 minute prior to extubation, potential benefit of dexmedetomidine in controlling haemodynamic response at the time of extubation and during postoperative period could not be established. Another limitation of this study was that there was a lack of Bispectral Index (BIS) monitoring to monitor intraoperative awareness.
Conclusion
Dexmedetomidine, during intraoperative infusion, controls stress response to various noxious stimuli and maintains haemodynamic stability. The sedative property postpones postoperative recovery, which may require monitoring for a longer duration in postoperative period.