Introduction
Obesity is rapidly becoming a pandemic and poses a serious health risk to the individuals. Abdominal obesity is quite common in India and is a prime risk factor for diseases like diabetes, coronary artery disease, Gastroesophageal Reflux Disease (GERD), osteoarthritis etc. A complex and multifactorial aetiopathogenesis of GERD exists in presence of obesity. The current study focuses on high Body Mass Index (BMI), a marker of obesity, as a risk factor for GERD and aims for a better understanding of their complex association.
Aim
To study the association between the BMI and symptoms as well as gross endoscopic appearance of GERD.
Materials and Methods
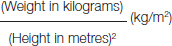
A prospective cross-sectional study was carried out at a tertiary care hospital in Maharashtra, India, between January 2016 and June 2016. A total of 176 patients referred for upper Gastrointestinal (GI) endoscopy due to dyspeptic symptoms of more than two months duration were selected. BMI (weight in kilograms/square of height in metres) was calculated for all patients and they were classified as normal weight (BMI 18.5 -24.9), overweight (BMI 25-29.9) and obese (BMI≥30). The frequency and severity of GERD symptoms was assessed by a self-administered questionnaire. Data on typical and atypical symptoms of GERD was collected. Upper GI endoscopy was done on all patients. Based on gross endoscopic appearance, the disease was divided as Endoscopy Negative Reflux Disease (ENRD) and true GERD (as per Los Angeles staging system). Association between BMI and frequency, severity and type of symptoms of GERD and also between BMI and gross endoscopic oesophagitis was studied using various statistical tests. All tests were two-tailed with a confidence level of 95%. A p-value < 0.05 was considered to be statistically significant.
Results
Typical symptoms of heartburn and acidic regurgitation were present in 71.6% subjects. The frequency and the severity of the dyspeptic symptoms increased significantly with increasing BMI (p<0.05). Based on the endoscopic gross appearance of the oesophageal mucosa, 48.3% participants had ENRD and 51.7% had erosive disease (GERD). High BMI had a statistically significant relationship with occurrence of both ENRD and GERD (p<0.05) but a statistically insignificant relationship with LA classification system for endoscopic oesophagitis.
Conclusion
The prevalence, frequency and severity of symptoms of GERD increases with increase in the BMI. Erosive oesophagitis has significant correlation with increasing BMI, but the staging and classification of endoscopic erosive oesophagitis is independent of the BMI of the patients.
Dyspepsia, Obesity, Oesophagitis, Overweight
Introduction
GERD is defined as a condition arising due to reflux of gastric contents into the oesophagus resulting in either troublesome symptoms such as heartburn, regurgitation, dysphagia, chest pain etc., or an array of extra-oesophageal manifestations such as chronic cough, asthma, arrhythmias, recurrent aspiration pneumonia, etc. Some degree of gastroesophageal reflux is normal {e.g., belching and transient relaxation of Lower Oesophageal Sphincter (LES)} but when it is excessive or when it is associated with impaired clearance of the refluxed gastric juice, it causes the disease complex called GERD.
In India, due to rapid urbanisation and industrialisation epidemiological trends are changing rapidly. In the post-Independence era, under-nutrition was the major health problem in India but now it is gradually being replaced by over-nutrition and obesity. Thus, obesity is rapidly becoming a disease entity in itself. Currently, the prevalence of GERD in India is estimated to be around 8-20% and is on the rise due to several factors such as changing dietary habits, lifestyle and improving socioeconomic status of Indians [1-3]. Excessive body weight or obesity is an independent risk factor for GERD and hiatus hernia [4]. Therefore, it is important to establish a relation between BMI and GERD, not only for its impact on the treatment options but also because both of these have been implicated as important risk factors for development of oesophageal adenocarcinoma [5].
The integrity of the normal gastroesophageal junction is vital to prevent GERD and it depends on both the LES tone and the crural diaphragm. Transient LES relaxation is known to cause GERD symptoms in 90% of patients without hiatus hernia. Several factors such as pregnancy, delayed gastric emptying, gastric acid hypersecretion are known to cause GERD. This study was undertaken with an aim to assess the association, if any, between high BMI, a marker of obesity, and symptomatic GERD diagnosed on upper GI endoscopy and to assess the severity of damage to the oesophagus and GE junction in these patients.
Materials and Methods
This was a cross-sectional observational study of six months duration done between January to June 2016 at a tertiary care hospital in Maharashtra, India. A total of 176 patients above 18 years of age, having symptoms of dyspepsia for more than two months and referred for gastroscopy, were enrolled for the study. The following were exclusion criteria for selection of study subjects: Patients with age less than 18 years; habitual smokers; alcoholics; known cases of peptic ulcer disease, gastroesophageal malignancy and those treated with analgesics; daily and regular users of proton-pump inhibitors and H2 blockers on advice of a physician in the past four weeks. Those using alternative therapy (ayurvedic/homoeopathic medicines) and PPI or H2 blockers occasionally were included in the study. BMI was calculated for all study participants using the following formula [6,7]:
According to the WHO’s (World Health Organisation) classification for BMI cut-off points, the study subjects were classified as normal weight (BMI between 18.5 to 24.9 kg/m2), overweight (BMI between 25 to 29.9 kg/m2) and obese (BMI ≥ 30 kg/m2 and above) [7]. For the purpose of this study, GERD or dyspepsia was defined as re-flux of stomach contents caused troublesome symptoms of either heartburn or acidic regurgitation (Montreal definition for GERD) [8] of more than two months duration. A duration of two months was chosen for this study as it suggested that the symptoms were chronic, recurrent and not acute since acute transient dyspepsia does not require detailed investigations. A burning sensation in the chest behind the breast-bone or in the neck was defined as heartburn. Acidic regurgitation was described as a sour taste in the mouth or a sense of fluid moving up and down in the chest [9]. The frequency and severity of GERD symptoms was assessed by a self-validated, self-administered questionnaire. The internal consistency of the questionnaire was assessed by using Cronbach Alpha. Construct validity of our questionnaire was assessed by comparing it to previously validated questionnaires like GERD symptom frequency questionnaire (GSFQ) [10]. Symptom frequency was reported as: about once a month; about once a week; several times a week; and daily. Symptoms occurring once a week or more were defined as “frequent”. Severity of symptoms was reported as mild (“can be ignored”); moderate (“cannot be ignored, but can carry out routine activity”); severe (“affects routine activity”); and very severe (“marked effect on routine activity”) [5]. Gastroscopy was performed on all study subjects and the endoscopic gross appearance of the oesophagus was used to diagnose GERD. Based on the endoscopic appearance, the dyspepsia was divided into Endoscopy-Negative Reflux Disease (ENRD) and Erosive Disease (true GERD). The term “endoscopy-negative reflux disease” was defined according to the Genval Workshop as applying to individuals who satisfy the definition of GERD but who have neither Barrett’s oesophagus nor definite endoscopic oesophageal mucosal breaks [11]. Erosive Disease was further classified according to the Los Angeles system of classification for oesophagitis on endoscopy [12], which is as follows:
GRADE A: More than one mucosal breaks no longer than 5 mm, none of which extends between the tops of the mucosal folds.
GRADE B: More than one mucosal breaks more than 5 mm long, none of which extends between the tops of two mucosal folds.
GRADE C: Mucosal breaks that extend between the tops of two or more mucosal folds, but involving less than 75% of the oesophageal circumference.
GRADE D: Mucosal breaks involving at least 75% of the oesophageal circumference [12].
Statistical Analysis
All data were reported as mean ± standard deviation (except frequencies). The chi-square test of independence was used for comparison between sets of distinct sub-groups. This was the case when comparing gender and BMI; gender and GERD incidence; BMI and ENRD/GERD incidence. Similarly, Fisher’s-exact test was used for comparison between BMI (only overweight/obese categories) and GERD staging level.
Odds ratio was used to determine if there was a statistically significant association between the independent variable and the dependent variable in each of the following cases: BMI and atypical/typical symptoms; BMI and frequency of symptoms of dyspepsia; BMI and level of severity of dyspeptic symptoms.
All tests were two-tailed with a confidence level of 95% (i.e., with significance defined as p<0.05). Analysis was performed using standard commercially available software (Microsoft Excel 2013).
Results
A total of 176 patients (n=176) participated in the study, of which 98 were males and 78 were females. The mean age of the study participants was 46 years and the mean BMI was 25.2 kg/m2. Of all study participants, 37.5% had above-normal BMI (BMI > 24.9). [Table/Fig-1] shows the participant profile and distribution of symptoms according to the three BMI categories (normal, overweight and obese). Overall, 71.6% patients presented with typical symptoms of heartburn (46%) and acidic regurgitation (54%). Atypical symptoms such as dysphagia, belching, bloating, etc., were present in 28.4% of patients and were more often recorded in the higher BMI subgroup than the normal BMI subgroup (i.e., 51.5% vs 14.5%) patients.
Patient profile, GERD symptoms – Frequency and severity.
| Variable | Allpatientswithdyspepsia(n=176) | Normalweight(Patients withBMI ≤ 24.9)n = 110(62.5%) | Overweight(Patients withBMI ≥25 – 29.9)n = 40(22.72%) | Obese(Patientswith BMI≥30)n = 26(14.78%) |
|---|
| Patient profile |
| Age (years) | 46±10.6 | 43±10.24 | 49±9.74 | 56±5.9 |
| SexMale (%)Female (%) | 98 (56)78 (44) | 60 (55)50 (45) | 22 (55)18 (45) | 16 (62)10 (38) |
| Weight (kg) | 70.1±12.4 | 62.6±5.5 | 75.3±4.4 | 93.7±7.1 |
| Height (m2) | 1.68±0.01 | 1.68±0.01 | 1.68±0.01 | 1.68±0.01 |
| BMI (Kg/m2) | 25.2±4.4 | 21.63±1.9 | 27.2±1.5 | 33.2±2.4 |
| Symptoms |
| TypicalRegurgitation 68 (54%) and/orHeart Burn 58 (46%) | 126 (71.6) | 94 (85.45) | 24 (60) | 8 (30.77) |
| AtypicalDysphagia, Belching VomitingChest painBreathlessness | 50 (28.4) | 16 (14.55) | 16 (40) | 18 (69.23) |
| Frequency of symptomsOnce a monthOnce a weekSeveral times a weekDaily | 12 (6.8)83 (47.2)36 (20.4)45 (25.6) | 9 (8.2)68 (61.8)7 (6.4)26 (23.6) | 2 (5)10 (25)16 (40)12 (30) | 1 (3.8)5 (19.2)13 (50)7 (26.9) |
| Severity of symptomsMildModerateSevereVery severe | 33 (18.8)47 (26.7)72 (40.9)24 (13.6) | 16 (14.5)25 (22.7)53 (48.2)16 (14.5) | 11 (27.5)12 (30)12 (30)5 (12.5) | 6 (23.1)10 (38.5)5 (19.2)5 (19.2) |
The percentage of participants with symptoms of GERD atleast once a week (47.2%) and with severe symptoms (40.9%) was the highest.
Taking normal BMI as the baseline, the odds ratio for frequency of symptoms (once a week to several times a week) was highly statistically significant for the overweight and obese categories, i.e., higher the BMI, greater the chances of having frequent symptoms of GERD (p-value < 0.0001).
The high BMI sub-group had more severe symptoms as compared to the normal BMI sub-group and it commonly affected their daily routine activities (p-value 0.0037).
[Table/Fig-2] shows endoscopic findings in all the patients according to their BMI.
Endoscopic appearance according to the BMI.
| Variable | All patientswithdyspepsia(n=176) | Normal weight(Patients withBMI ≤ 24.9)n = 110 | Overweight(Patientswith BMI ≥25 – 29.9)n = 40 | Obese(Patientswith BMI≥30)n = 26 |
|---|
| Endoscopic Picture |
| Normal oesophagus (ENRD) | 85 (48.3) | 61 (55.5) | 13 (32.5) | 11 (42.3) |
| Abnormal oesophagus (with erosions/ulcers)According to LA aGrade AGrade BGrade CGrade D | 91 (51.7)n=9168 (74.7)20 (22)3 (3.3)0 (0) | 49 (44.5)n=4932 (65.3)15 (30.6)2 (4.1)0 (0) | 27 (67.5)n=2723 (85.2)4 (14.8)0 (0)0 (0) | 15 (57.7)n=1513 (86.7)1 (6.7)1 (6.7)0 (0) |
Based on the upper GI endoscopic gross appearance of the oesophageal mucosa, 85 (48.3%) participants had ENRD and 91 (51.7%) had erosive disease (GERD).
Of the ENRD patients, 55.5% had normal BMI while the rest had high BMI. Of the GERD patients, 44.5% had normal BMI while the rest had high BMI. Increasing BMI had a statistically significant relationship with increased occurrence of both ENRD and GERD (p-value < 0.05).
Participants with GERD were further classified as per the Los Angeles staging system for oesophagitis into Grade A through D. Across all categories of BMI, a majority of the participants were classified as Grade A or B. A total of only 3 participants were classified under Grade C and none under Grade D. The relation between high BMI and oesophagitis according to LA staging system was statistically insignificant.
Discussion
GERD is an increasingly recognised disease in today’s world and its pathophysiology and causative factors are not much understood. Similarly, obesity is fast becoming a separate disease entity and many studies have been carried out about its ill effects on various systems. Structural and functional defects in LES and its tonicity predisposes to GERD. Obesity is one of the factors along with others such as smoking, diabetes mellitus, hiatus hernia, connective tissue disorders like scleroderma which are associated with GERD. It has been studied that increasing BMI increases the risk of developing GERD [13]. However, only three of the nine studies [5,9,14-20] showed a statistically significant relationship between obesity and GERD symptoms. The current study was undertaken with an aim to determine the correlation of GERD with increasing BMI and to ascertain whether the frequency and severity of the GERD symptoms increase significantly with increasing BMI.
The total prevalence of overweight and obesity in the current study was 37.5% (BMI ≥25 kg/m2) which corresponded with a similar study done in 2013 to evaluate the effect of weight loss on reduction of GERD symptoms where the baseline prevalence of GERD was 37% [21]. Among the patients with high BMI, 38.8% were males and 35.9% were females. According to the WHO fact sheet on obesity (WHO fact sheet updated in June 2016), 39% of adults aged 18 years and above were overweight in 2014 (38% of men and 40% of women) [22].
Regurgitation (54%) was a more often recorded symptom than heartburn (46%) in our study. This finding corresponded with that of a study done by Singh M et al., where regurgitation was more frequently recorded than the other symptoms [21]. Also, we found that there was a statistically significant association between increasing BMI and occurrence of atypical dyspeptic symptoms like belching, bloating and respiratory symptoms like breathlessness, chest pain etc. The potential effects of reflux on respiratory functions in the obese can vary from Obstructive Sleep Apnoea Syndrome (OSAS), asthma to GERD-related laryngeal or airway disease which can be problematic to tackle. Of note here is a complex relationship between obesity, obstructive sleep apnoea syndrome and GERD. It has been studied that obesity may contribute to the increased nocturnal reflux episodes and worsen the symptoms of OSAS by certain obesity-related functional changes in the gastrointestinal tract, including slower oesophageal transit, increased intra abdominal pressure, presence of hiatal hernia, which increases oesophageal acid clearance times [23]. With reduction in body weight either medically or surgically, symptoms of both apnea and GERD have been reported to improve [24-26].
In our study, the frequency of symptoms (once a week and several times a week) increased significantly with increasing BMI (p-value < 0.0001). However, there was a statistically insignificant association between BMI and GERD in patients having dyspepsia symptoms either infrequently or daily suggesting that there may be other contributory factors like age, gender and other co-morbidities for such participants. A large cohort study done on 10,545 women showed that as participant BMI increased, the odds ratios for frequency of symptoms increased significantly (p < 0.001). It has also reported a possible dose-response increase in the risk of GERD even in the normal range of BMI [27].
We concluded that the higher the BMI, the greater is the severity of symptoms. This was also noted in few other studies [5,27].
The pathophysiology of GERD differs between obese and non-obese subjects. In the obese, the primary mechanism of GERD is largely structural. The weight of abdominal fat presses the stomach, causing an increased tendency to gastroesophageal reflux and dyspepsia symptoms. Obese patients having long standing GERD are more sensitive to the reflux of acidic contents of the stomach into the oesophagus. There is a higher prevalence of hiatus hernia in overweight patients, which in itself is a risk factor for development and progression of GERD [28]. Symptoms of GERD are more severe in obese subjects because of several factors. There is an increased gastoesophageal gradient because of displaced lower oesophageal sphincter, which is due to increased intra-abdominal pressure. Obesity-associated vagal abnormalities cause increase in biliary and pancreatic enzyme output. This in turn makes the gastric refluxate highly toxic, increasing the damage to the oesophageal mucosa and severity of the dyspepsia [29].
In our study, higher BMI was an important and independent risk factor for GERD as well as ENRD (p < 0.05). Obesity and erosive oesophagitis had a statistically significant cause and effect relationship in our study. This finding was similar to several studies done in the past to ascertain the causal relationship of obesity with erosive oesophagitis [4,30-33]. But it is to be noted that most of these studies were hospital-based with a small sample size and thus prone to bias. Endoscopic staging of GERD according to the LA staging system did not have a statistically significant association with obesity. Therefore, although obesity was an independent risk factor for occurrence of symptoms of erosive oesophagitis, it did not affect its severity and extent on-gross endoscopic evaluation. This finding did not match with a study done by Abdelkadar NA et al., where a statistically significant relationship was found between obesity and endoscopic severity of GERD [34].
Limitation
The limitations of our study were its small sample size and selection bias for patient selection.
Conclusion
It has been put forward through many studies that overweight and obese individuals are at higher risk of developing GERD and they tend to have a higher frequency and severity of symptoms as compared to normal weight individuals. Our study corroborates and supports this hypothesis and shows that the prevalence, frequency and severity of GERD increases with increase in BMI. Thus, obesity is an independent risk factor for GERD and endoscopic erosive oesophagitis. High prevalence of ENRD in individuals with high BMI may be due to obesity related functional changes in their gastrointestinal tract. Atypical symptoms of GERD also significantly correlate with overweight and obesity. Although erosive oesophagitis is more often detected during upper GI endoscopy in overweight and obese patients, staging and classification of endoscopic erosive oesophagitis is independent of the BMI of the patients. Thus, our study highlights the need for implementing weight reduction strategies as a treatment tool for GERD in obese patients.
[1]. Bhatia SJ, Reddy DN, Ghoshal UC, Jayanthi V, Abraham P, Choudhuri G, Epidemiology and symptom profile of gastroesophageal reflux in the Indian population: Report of the Indian society of gastroenterology task forceIndian Journal of Gastroenterology 2011 30(3):118-27. [Google Scholar]
[2]. Sharma PK, Ahuja V, Madan K, Gupta S, Raizada A, Sharma MP, Prevalence, severity, and risk factors of symptomatic gastroesophageal reflux disease among employees of a large hospital in northern IndiaIndian Journal of Gastroenterology 2011 30(3):128-34. [Google Scholar]
[3]. Kumar S, Sharma S, Norboo T, Dolma D, Norboo A, Stobdan T, Population based study to assess prevalence and risk factors of gastroesophageal reflux disease in a high altitude areaIndian Journal of Gastroenterology 2011 30(3):135-43. [Google Scholar]
[4]. Wilson LJ, Ma W, Hirschowitz BI, Association of obesity with hiatal hernia and oesophagitisThe American Journal of Gastroenterology 1999 94(10):2840-44. [Google Scholar]
[5]. Murray L, Johnston B, Lane A, Harvey I, Donovan J, Nair P, Relationship between body mass and gastro-ooesophageal reflux symptoms: The Bristol Helicobacter ProjectInt J Epidemiol 2003 32:645-50. [Google Scholar]
[6]. Index BM. Considerations for Practitioners. [Cited 10 Sep 2016] from Center for Disease Control and Prevention. Available from: https://www.cdc. gov/obesity/downloads/BMIforPactitioners.pdf.:1-4 [Google Scholar]
[7]. WHO: Global Database on Body Mass Index [Internet]. World Health Organization. 2016 [cited 3 September 2016]. Available from: http://who.int/bmi/index.jsp?introPage=intro_3.html [Google Scholar]
[8]. Vakil N, Van Zanten SV, Kahrilas P, Dent J, Jones R, The Montreal definition and classification of gastroesophageal reflux disease: A global evidence-based consensusThe American Journal of Gastroenterology 2006 101(8):1900-20. [Google Scholar]
[9]. Locke G, Talley N, Fett S, Zinsmeister A, Melton L, Risk factors associated with symptoms of gastroesophageal refluxThe American Journal of Medicine 1999 106(6):642-49. [Google Scholar]
[10]. Paré P, Meyer F, Armstrong D, Pyzyk M, Pericak D, Ron G, Validation of the GSFQ, a self-administered symptom frequency questionnaire for patients with gastroesophageal reflux diseaseCanadian Journal of Gastroenterology and Hepatology 2003 17(5):307-12. [Google Scholar]
[11]. Dent J, Brun J, Fendrick AM, Fennerty MB, Janssens J, Kahrilas PJ, An evidence-based appraisal of reflux disease management—the Genval Workshop ReportGut 1998 44(suppl 2):S1-6. [Google Scholar]
[12]. Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, Endoscopic assessment of oesophagitis: Clinical and functional correlates and further validation of the Los Angeles classificationGut 1999 45(2):172-80. [Google Scholar]
[13]. Hampel H, Abraham NS, El-Serag HB, Meta-analysis: Obesity and the risk for gastroesophageal reflux disease and its complicationsAnn Intern Med 2005 143:199-211. [Google Scholar]
[14]. Andersen LI, Jensen G, Risk factors for benign oesophageal disease in a random population sampleJ Intern Med 1991 230:5-10. [Google Scholar]
[15]. Oliveria SA, Christos PJ, Talley NJ, Dannenberg AJ, Heartburn risk factors, knowledge, and prevention strategies: A population-based survey of individuals with heartburnArch Intern Med 1999 159:1592-98. [Google Scholar]
[16]. Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J, Obesity and estrogen as risk factors for gastroesophageal reflux symptomsJAMA 2003 290:66-72. [Google Scholar]
[17]. Diaz-Rubio M, Moreno-Elola-Olaso C, Rey E, Locke GR, Rodriguez-Artalejo F, Symptoms of gastroesophageal reflux: Prevalence, severity, duration and associated factors in a Spanish populationAliment Pharmacol Ther 2004 19:95-105. [Google Scholar]
[18]. Lagergren J, Bergström R, Nyrén O, No relation between body mass and gastroesophageal reflux symptoms in a Swedish population based studyGut 2000 47:26-29. [Google Scholar]
[19]. Wu AH, Tseng CC, Bernstein L, Hiatal hernia, reflux symptoms, body size, and risk of oesophageal and gastric adenocarcinomaCancer 2003 98:940-48. [Google Scholar]
[20]. Stanghellini V, Three-month prevalence rates of gastrointestinal symptoms and the influence of demographic factors: Results from the Domestic/International Gastroenterology Surveillance Study (DIGEST)Scand J Gastroenterol Suppl 1999 231:20-28. [Google Scholar]
[21]. Singh M, Lee J, Gupta N, Gaddam S, Smith BK, Wani SB, Weight loss can lead to resolution of gastroesophageal reflux disease symptoms: a prospective intervention trialObesity 2013 21(2):284-90. [Google Scholar]
[22]. Obesity and overweight [Internet]. World Health Organization. 2016 [cited 12 July 2016]. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/ [Google Scholar]
[23]. Orr WC, Heading R, Johnson LF, Kryger M, Review article: sleep and its relationship to gastroesophageal refluxAlimentary Pharmacology and Therapeutics 2004 20(s9):39-46. [Google Scholar]
[24]. Clements RH, Gonzalez QH, Foster A, Richards WO, McDowell J, Bondora A, Gastrointestinal symptoms are more intense in morbidly obese patients and are improved with laparoscopic Roux-en-Y gastric bypassObesity Surgery 2003 13(4):610-14. [Google Scholar]
[25]. Melissas J, Christodoulakis M, Spyridakis M, Schoretsanitis G, Michaloudis D, Papavasiliou E, Disorders associated with clinically severe obesity: Significant improvement after surgical weight reductionSouthern Medical Journal 1998 91(12):1143-48. [Google Scholar]
[26]. Mathus-Vliegen EM, Tytgat GN, Gastroesophageal reflux in obese subjects: Influence of overweight, weight loss and chronic gastric balloon distensionScandinavian Journal of Gastroenterology 2002 37(11):1246-52. [Google Scholar]
[27]. Jacobson BC, Somers SC, Fuchs CS, Kelly CP, Camargo Jr CA, Body-mass index and symptoms of gastroesophageal reflux in womenNew England Journal of Medicine 2006 354(22):2340-48. [Google Scholar]
[28]. Che F, Nguyen B, Cohen A, Nguyen NT, Prevalence of hiatal hernia in the morbidly obeseSurgery for Obesity and Related Diseases 2013 9(6):920-24. [Google Scholar]
[29]. Barak N, Ehrenpreis ED, Harrison JR, Sitrin MD, Gastroesophageal reflux disease in obesity: Pathophysiological and therapeutic considerationsObesity Reviews 2002 3(1):9-15. [Google Scholar]
[30]. Labenz J, Jaspersen D, Kulig M, Malfartheiner P, Risk factors for erosive oesophagitis: A multivariate analysis based on the ProGERD study initiativeAm J Gastroenterol 2004 99(9):1652-56. [Google Scholar]
[31]. Chang CS, Poon SK, Lien HC, Chen GH, The incidence of reflux oesophagitis among the ChineseAm J Gastroenterol 1997 92(4):668-71. [Google Scholar]
[32]. Stene-Larsen G, Weberg R, Froyshov Larsen I, Bjortuft O, Hoel B, Berstad A, Relationship of overweight to hiatus hernia and reflux oesophagitisScand J Gastroenterol 1988 23(4):427-32. [Google Scholar]
[33]. Ruhl CE, Everhart JE, Overweight, but not high dietary fat intake, increases risk of gastroesophageal reflux disease hospitalization: The NHANES I epidemiologic follow up study. First National Health and Nutrition Examination SurveyAnn Epidemiol 1999 9(7):424-35. [Google Scholar]
[34]. Abdelkader NA, Montasser IF, Bioumy EE, Saad WE, Impact of anthropometric measures and serum leptin on severity of gastroesophageal reflux diseaseDiseases of the Oesophagus 2015 28(7):691-98. [Google Scholar]