Evaluation of Periapical Healing of Apicomarginal Defect in Mandibular First Molar Treated with Platelet Rich Fibrin: A Case Report
Jitesh Wadhwa1, Alpa Gupta2, Suruchi Hans3
1 Reader, Department of Orthodontics, K.D Dental College, Mathura, Mathura, Uttar Pradesh, India.
2 Senior Resident, Department of Conservative Dentistry and Endodontics, Postgraduate Institute of Dental Sciences, Rohtak, Haryana, India.
3 Reader, Department of Periodontics, Maharaja Ganga Singh Dental College and Research, Ganganagar, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Alpa Gupta, 640/30, Adarsh Nagar, Rohtak-124001, Haryana, India.
E-mail: alpagupta2008@gmail.com
The presence of an apicomarginal defect is one of the reasons for the failure of endodontic treatment. The best treatment option to treat an apicomarginal defect is to perform endodontic surgery using Guided Tissue Regeneration (GTR) membranes. The present case report evaluated the healing of periapical lesion along with apicomarginal defect using Platelet Rich Fibrin (PRF) as membrane in periapical surgery of mandibular first molar. Recall examination was performed at 3 and 18 months post surgery. A satisfactory periapical healing was evident using PRF in apicomarginal defect of mandibular first molar. PRF may be considered as an alternative treatment for GTR membranes in the treatment of apicomarginal defects.
Endodontic periodontal communications, Guided tissue regeneration, Mineral trioxide aggregate
Case Report
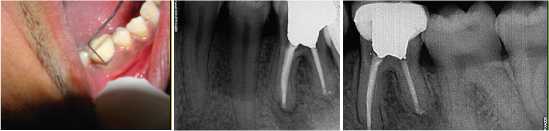
A 25-year-old male patient reported to the Department of Conservative Dentistry and Endodontics with pain and complain of pus discharge in lower right posterior tooth. On clinical examination, extensive occlusal caries and a sinus opening on the buccal aspect of gingiva was found with respect to the right mandibular first molar. An intraoral periapical radiograph revealed deep occlusal caries approximating the pulp with periapical radiolucency with respect to mesial and distal roots [Table/Fig-1a]. The sinus track was traced with the gutta percha point in order to confirm the related tooth. The Pocket Depth (PD) of more than 10 mm on the midbuccal aspect of the tooth was observed with help of periodontal Williams O probe. Baseline Clinical Attachment Level (CAL) and Gingival Marginal Position (GMP) with respect to concerned tooth were also measured and found to be 10 mm and 0 mm respectively. The diagnosis of irreversible pulpitis was determined on the basis of clinical assessment, including history of spontaneous, intense and lingering pain to cold stimulus. Further the diagnosis includes suppurative chronic apical periodontitis and endodontic- periodontal communication to the apex. According to Simon JH et al., classification the lesion is described as primary endodontic lesion with secondary periodontal involvement [1]. The patient was informed about the treatment modality and the root canal treatment was performed [Table/Fig-1b]. The patient reported to the department after a period of 3 months with similar complaint of pus discharge in relation to the same previously treated tooth. Again the sinus opening on the buccal aspect of the gingiva was found. PD of 10 mm was reported without any reduction [Table/Fig-1c,d]. Any clinical or radiographic evidence of vertical root fracture was not evident. Taking into consideration all the above mentioned facts, the periapical surgery was planned. Consent was obtained from the patient after careful explanations of the surgical procedure used along with the risks and benefits.
Surgical Techniques
First of all the patient was anesthetized with 2% lidocaine with 1:80,000 epinephrine (Xylocaine; Astra Zeneca Pharma, Bangalore, India). After the elevation of a full-thickness mucoperiosteal flap, an osteotomy was performed with round burs under copious saline irrigation in order to locate the root end of mesial root. The distal root was already exposed upto the apex [Table/Fig-1e]. The resection of roots was done for approximately 3mm from the root apex. All the pathological tissue was debrided from the surgical site and excessive bleeding was controlled with cotton pellets dipped in 0.1% epinephrine (Jackson Lab (P) Ltd, Punjab, India). Root-end preparations extending 3 mm into the canal space along the long axis of the root were made with S12-7D ultrasonic retrotips (Satelec) driven by a piezoelectric ultrasonic unit (P5 Booster, Suprasson Neutron; Acteon Inc, Mt. Laurel, NJ). Finally mineral trioxide aggregate (Pro Root; Retroplast Trading, Rorvig, Denmark) was placed as root end filling material whose appropriate placement was verified by an operating microscope under high magnification. PRF was prepared by drawing the required amount of blood into a 10 ml test tube without an anticoagulant and centrifuged immediately using a table top centrifuge (REMI Laboratories, Mumbai, Maharashtra, India) for 10 minutes at 3,000 rpm. After centrifugation the final end product comprised of acellular platelet poor plasma at the top of the tube. Middle layer consisted of PRF and red blood corpuscles were present at the bottom of the tube. During preparation of PRF, the blood was collected and centrifuged at a faster rate in order to avoid the coagulation [2].
Finally, a PRF membrane was prepared by pressing out the fluid from fibrin clot, which was then placed over the treated site [Table/Fig-1f] [2]. A 4-0 monofilament sutures were used to close the surgical site. Finally a postoperative radiograph was obtained [Table/Fig-1g]. The patient was instructed regarding the postoperative care, the sutures were removed after seven days of surgical treatment, and the healing progress was checked and found to be satisfactory. The patient reported for follow up at three months. After that patient came for routine follow up at 18 months since he had left the station for some months. To evaluate the healing of periapical lesion the radiographs were taken using Rinn (XCP Instruments, Elgin, IL) parallel technique. Finally the data was digitalized with Kodak RVG 6000 (Kodak Digital Radiography System, Pt. Husada Intra Care, Indonesia). Periodontal PD, CAL and GMP were also recorded. Baseline radiograph was compared with postsurgical follow up radiographs to characterize radiographic periapical healing as complete, incomplete (scar tissue formation), uncertain (some reduction of former radiolucency), or unsatisfactory (no reduction or enlargement of former radiolucency) as explained by Rud J et al., and Molven O et al., [3,4]. In our case after applying the above mentioned criteria the results came under the category of successful outcome.
a) The preoperative radiograph; b) The post obturation radiograph; c) The preoperative probing depth; d) Tracing of sinus tract with the aid of gutta percha. e) Exposed distal root and window preparation with respect to mesial root of first molar; f) PRF membrane placement over the surgical site; g) Immediate post surgical radiograph. (Images from left to right)

Discussion
An apicomarginal defect can be explained as a total loss of buccal alveolus extending from original crestal bone to the apex of the tooth [5]. The healing of apicomarginal defects in anterior region using different treatment modalities which have been already mentioned in various studies [6-9]. The present case report highlights the role of PRF in the healing of apicomarginal defect in mandibular first molar area. The case was performed without using any bone graft in order to evaluate the role of PRF alone in healing of such defects. The presence of deep periodontal pocket, large periapical radiolucency with endodontic periodontal communication to the apex and lastly the presence of buccal bone loss with no evidence of vertical root fracture categorizes the present case into E and F type of periodontal lesions as described by Kim E [10].
PRF is a second-generation platelet concentrate extensively utilize to improve soft and hard-tissue healing. It helps in stimulating the defense mechanism. The various growth factors released by PRF like cytokines, present in the fibrin meshwork plays an important role in healing process [2].
The role of PRF has been well documented in regeneration process for the treatment of periodontal intrabony defects, gingival recessions and furaction defects [11-14]. Since very few studies evaluated healing of apicomarginal defects in posterior region [Table/Fig-2] [6,7], further studies are required in this direction. The results of present case report revealed that at three months, the PD was found to be reduced from 10 mm to 2 mm [Table/Fig-3]. The periodontal parameters, CAL and GMP remained same for both three months and 18 months i.e., 2 mm and 0 mm respectively [Table/Fig-4a]. Complete periapical radiographic healing was found at 3months and 18 months follow up period based on the criteria established by Rud et al., and Molven et al., [Table/Fig-4b,c] [3,4]. The possible reasons of healing in present case may be attributed by the two factors. Firstly by the immune-regulatory action of PRF and secondly removal of infection from the surgical site, promotes the connective tissue and bone formation from adjacent healthy periodontium [15].
Apicomarginal studies in posterior region using different treatment modalities.
| Study | Site & type of defect treated | Treatment modality |
|---|
| Marin-Botero et al., [6] | Treated apicomarginal defect in 8 mandibular, 22 maxillary teeth | Guided tissue regeneration |
| Dietrich et al., [7] | Treated apicomarginal defect in 11 mandibular molars, 2 maxillary molars, 3 maxillary premolars & 1 mandibular premolar | Guided tissue regeneration with bone graft. |
Preoperative & postoperative clinical parameters assessment.
| PD | CAL | GMP |
|---|
| Preoperative clinical assessment | >10 mm | 10 mm | 0 mm |
| Postoperative clinical assessment | 2 mm | 2 mm | 0 mm |
a) Three month post surgical probing depth; b) Three months post surgical follow up; c) 18 months post surgical follow up. (Images left to right)
Conclusion
PRF plays an important role in healing of an apicomarginal defects which was evident in the present case report but more studies are required to confirm its relevance.
[1]. JH Simon, DH Glick, AL Frank, The relationship of endodontic-periodontic lesionsJ Periodontol 1972 43:202-08. [Google Scholar]
[2]. DM Dohan, J Choukroun, A Diss, SL Dohan, AJ Dohan, J Mouhyi, Platelet rich fibrin (PRF):a second generation platelet concentrate. Part I: technological concepts and evolutionOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101:e37-44. [Google Scholar]
[3]. J Rud, JO Andreasen, JE Moller-Jensen, Radiographic criteria for the assessment of healing after endodontic surgeryInt J Oral Surg 1972 1:195-214. [Google Scholar]
[4]. O Molven, A Halse, B Grung, Observer strategy and the radiographic classification of healing after endodontic surgeryInt J Oral Maxillofac Surg 1987 16:432-39. [Google Scholar]
[5]. JL Gutmann, JW Harrison, Success, failure, and prognosis in periradicular surgeryIn: Surgical Endodontics 1991 1st EditionBostonBlackwell Scientific Publications:338-9. [Google Scholar]
[6]. ML Marin-Botero, JS Dominguez-Mejia, JA Arismendi-Echavarria, AL Mesa- Jaramillo, GA Florez-Moreno, SI Tobon-Arroyave, Healing response of apicomarginal defects to two guided tissue regeneration techniques in periradicular surgery: a double-blind, randomized-clinical trialInt Endod J 2006 39:368-77. [Google Scholar]
[7]. Y Dietrich, P Zunker, D Dietrich, JP Bernimoulin, Periapical and periodontal healing after osseous grafting and guided tissue regeneration treatment of apicomarginal defects in periradicular surgery: results after 12 monthsOral Surg Oral Med Oral Patholo Oral Radiol Endod 2003 95:474-82. [Google Scholar]
[8]. B Goyal, S Tewari, J Duhan, PK Sehgal, Comparative evaluation of platelet-rich plasma and guided tissue regeneration membrane in the healing of apicomarginal defects: A Clinical StudyJ Endod 2011 37:773-80. [Google Scholar]
[9]. M Dhiman, S Kumar, J Duhan, P Sangwan, S Tewari, Effect of platelet-rich fibrin on healing of apicomarginal defects: a randomized controlled trialJ Endod 2015 41:985-91. [Google Scholar]
[10]. E Kim, JS Song, IY Jung, SJ Lee, S Kim, Prospective clinical study evaluating endodontic microsurgery outcomes for cases with lesions of endodontic origin compared with cases with lesions of combined periodontal-endodontic originJ Endod 2008 34:546-51. [Google Scholar]
[11]. MK Thorat, AR Pradeep, B Pallavi, Clinical effect of autologous platelet-rich fibrin in the treatment of intra-bony defects: a controlled clinical trialJ Clin Periodontol. 2011 38:925-32. [Google Scholar]
[12]. A Sharma, AR Pradeep, Treatment of 3-wall intrabony defects in patients with chronic periodontitis with autologous platelet-rich fibrin: a randomized controlle clinical trialJ Clin Periodontol 2011 82:1705-12. [Google Scholar]
[13]. A Sharma, AR Pradeep, Autologous platelet-rich fibrin in the treatment of mandibular degree II furcation defects: a randomized clinical trialJ Periodontol 2011 82:1396-403. [Google Scholar]
[14]. M Del Corso, G Sammartino, DM Dohan Ehrenfest, Re. Clinical evaluation of a modified coronally advanced flap alone or in combination with a plateletrich fibrimembrane for the treatment of adjacent multiple gingival recessions: a 6-month study. (letter to the editor)J Periodontol 2009 80:1694-97. [Google Scholar]
[15]. L Lin, MY Chen, D Ricucci, PA Rosenberg, Guided tissue regeneration in periapical surgeryJ Endod 2010 36:618-25. [Google Scholar]