Palpable breast lump is a common diagnostic problem encountered by both general practitioners and surgeons. Moreover, breast cancer is now one of the leading causes of cancer in Indian women, being second only to cervical cancer [1-3]. It is one of the leading causes of mortality with nearly 80,000 new cases being diagnosed annually [4].
In the past 20 years, the importance of FNAC has been well documented in the diagnosis of breast lesions [5-7]. Many authors have used various means to come to a conclusive method of diagnosis by FNAC of breast lesions [8-21].
A precise and objective cytological scoring system to diagnose and distinguish proliferative breast disease was first proposed by Masood et al., [22]. They developed a cytological grading system evaluating the palpable breast lump aspirates for the cellular arrangement, the degrees of cellular pleomorphism and anisonucleosis, presence of myoepithelial cells and nucleoli, and the status of the chromatin pattern [18,19]. High degree of concordance observed by Masood et al., between cytological and histological diagnoses led to the proposal of a cytological grading system which is now recognized as MSI [18,22].
Even though there have been reports advocating inclusion of additional cytological criteria into MSI for better diagnostic accuracy, the original criteria is widely accepted and used for cytological diagnosis of breast aspirates. Nandini et al., found that, modifying the original MSI by advocating a change in the scoring range for non proliferative breast disease from 6–10 to 6–8 with shift of scores 9 and 10 to proliferative breast disease without atypia could significantly improve the diagnostic accuracy in group I and II of original MSI. The modified scoring system was named as MMSI [20].
Considering the paucity of studies comparing the diagnostic accuracy of MSI with MMSI, the present study was planned to assess and compare the diagnostic accuracy of MSI & MMSI by comparing it with subsequent histopathological evaluation.
Materials and Methods
The cross-sectional study was approved by the institutional ethical committee and was conducted at Department of Pathology, in a tertiary care centre in southern India over a period of 2 years; from November 1, 2012 to September 30, 2014. All procedures followed in the study were in accordance with the ethical standards of the institutional ethics committee on human experimentation and with the Helsinki Declaration of 1975 that was revised in 2000.
Consecutive cases of palpable breast lumps referred to the Department of Pathology, Amala Institute of Medical Sciences for FNAC were included in the study. The exclusion criteria was inadequate cytology aspirate and cases in which histopathology specimens are unavailable. Criteria for adequacy of FNAC smears were defined by the presence of atleast four clusters of ductal epithelial cells, each made up of five to six cells.
The procedure for obtaining the specimen was first explained to the patient and informed consent was obtained. The lesion was then located, fixed and FNAC was carried out under strict aseptic precautions, with 22 gauge needles and 2ml syringes. A minimum of 3-4 slides were prepared from each subject. Atleast two of these smeared slides were wet fixed for Papanicolaou staining and the remaining was air dried for May-Grunwald-Giemsa (MGG) staining. The stained smears were then studied and grouped into 4 categories, using MSI [Table/Fig-1] and MMSI [Table/Fig-2].
Grading system for interpretation of FNAC (masood’s scoring index)
| Cellular arrangement | Cellular pleomorphism | Myoepithelial cells | Anisonucleosis | Nucleoli | Chromatin clumping | Score |
|---|
| Monolayer | Absent | Many | Absent | Absent | Absent | 1 |
| Nuclear overlapping | Mild | Moderate | Mild | Micronucleoli | Rare | 2 |
| Clustering | Moderate | Few | Moderate | Micronucleoli and/or rare macro nucleoli | Occasional | 3 |
| Loss of cohesion | Conspicuous | Absent | Conspicuous | Predominantly macro nucleoli | Frequent | 4 |
| Total score |
| Nonproliferative breast disease 6 – 10 |
| Proliferative breast disease without atypia 11 – 14 |
| Proliferative breast disease with atypia 15 – 18 |
| Carcinoma in situ / Carcinoma 19 – 24 |
Grading system for interpretation of FNAC (modified masood’s scoring index).
| Cellular arrangement | Cellular pleomorphism | Myoepithelial cells | Anisonucleosis | Nucleoli | Chromatin clumping | Score |
|---|
| Monolayer | Absent | Many | Absent | Absent | Absent | 1 |
| Nuclear overlapping | Mild | Moderate | Mild | Micronucleoli | Rare | 2 |
| Clustering | Moderate | Few | Moderate | Micronucleoli and/or rare macro nucleoli | Occasional | 3 |
| Loss of cohesion | Conspicuous | Absent | Conspicuous | Predominantly macro nucleoli | Frequent | 4 |
| Total score |
| Nonproliferative breast disease 6 –8 |
| Proliferative breast disease without atypia 9– 14 |
| Proliferative breast disease with atypia 15 – 18 |
| Carcinoma in situ / Carcinoma 19 – 24 |
The tissue sections of the respective cases from subsequent excision were prepared from formalin fixed, paraffin embedded blocks and stained with Haematoxylin and Eosin stains. These sections were analysed by an independent observer who was blinded to the FNAC results. Histological diagnosis of each case was categorized mainly into 4 categories [Table/Fig-3]. Correlation and concordance analysis between cytological and histopathological categories were conducted at the completion of the study.
Histopathological lesions included under each category.
| S No. | Category | Lesions Included |
|---|
| 1 | Non-proliferative lesions | FibrosisCystsAdenosis (non-sclerosing)Duct ectasiaBenign lumps or tumours (lipoma, hamartoma, haemangioma, haematoma, neurofibroma) |
| 2 | Proliferative lesions without atypia | Usual ductal hyperplasia (without atypia)Fibroepithelial proliferative lesions (Fibroadenoma, Benign Phyllodes tumour)Sclerosing adenosisMultiple papilloma or papillomatosisRadial scar |
| 3 | Proliferative lesions with atypia | Atypical ductal hyperplasiaAtypical lobular hyperplasia |
| 4 | Carcinoma in situ / Carcinoma | Ca in situ (all types)Carcinoma (all types) |
Statistical Analysis
The entire data collected in this study were of categorical type and thus the descriptive statistics of the data are shown as proportions and/or percentages. Diagnostic accuracy of the cytological scoring method was assessed by standard parameters of sensitivity, specificity, positive and negative predictive values. Overall diagnostic accuracy of cytological diagnoses was estimated using prevalence-weighted average of sensitivity and specificity. Fisher’s-exact test was employed to test the statistical significance of difference between the observed concordance rates of MSI versus MMSI for the various categories of cytological diagnosis. Inter-test agreement analysis for comparing the diagnostic accuracy of MSI and MMSI with reference to Histopathology was performed by calculating Cohen’s Kappa statistic. The level of acceptable alpha error was kept as 5%. All of the statistical analyses were done using GraphPad Prism Ver 6.0 for Windows.
Results
A total of 278 eligible patients were recruited for the study. FNAC in 12 (4.32%) patients did not yield sufficient cellular material and were excluded. Another 59 (21.22%) cases whose histopathologic specimens were unavailable were also excluded. The remaining 207 patients who were included underwent classification into 4 groups based on cytological diagnosis as per MSI and MMSI.
The patients included only females in the age range of 13 to 87 years. A 65.11% of cases were in the age range of 26-55 years (mean age - 46.1 years). A significant increasing trend in the proportion of older patients (above 55 years) was observed as we proceed from category 1 to category 4 of MSI (1 out of 48 in category 1, 3 out of 55 in category 2, 4 out of 15 in category 3 and 42 out of 87 in category 4; Chi-Square test, p < 0.0001).
A total of 5 (2.42%) patients out of 207 had bilateral breast lesions. In remaining 202 unilateral cases, 137(65.84%) had disease in the left breast. A total of 100 (48.31%) cases had involvement of upper outer quadrant. The size of breast lump ranged from 1cm to 7 cm (Mean - 2.71cm). The overall results of the 207 included cases with palpable breast lesions are shown in [Table/Fig-4,5].
Comparison of cytological (masood’s scoring index) and histopathological diagnosis.
| Cytology | Histology |
|---|
| Category | No. of cases | NPBD | PBD without atypia | PBD with atypia | Ca insitu | Carcinoma |
|---|
| NPBD | 50 | 38 | 12 | - | - | - |
| PBD without atypia | 55 | - | 51 | 1 | - | 3 |
| PBD with atypia | 15 | - | 4 | 9 | - | 2 |
| Ca insitu / Carcinoma | 87 | - | - | - | 2 | 85 |
| Total | 207 | 38 | 67 | 10 | 2 | 90 |
NPBD – Non proliferative breast disease, PBD – Proliferative breast disease.
Comparison of cytological (modified masood’s scoring index) and histopathological diagnosis.
| Cytology | Histology |
|---|
| Category | No. of cases | NPBD | PBD without atypia | PBD with atypia | Ca insitu | Carcinoma |
|---|
| NPBD | 41 | 38 | 3 | - | - | - |
| PBD without atypia | 64 | - | 60 | 1 | - | 3 |
| PBD with atypia | 15 | - | 4 | 9 | - | 2 |
| Ca insitu / Carcinoma | 87 | - | - | - | 2 | 85 |
| Total | 207 | 38 | 67 | 10 | 2 | 90 |
NPBD – Non proliferative breast disease, PBD – Proliferative breast disease
Non-Proliferative Breast Disease (NPBD)
Cytomorphological features of this group are shown in the representative figure [Table/Fig-6].
a) Monolayered cluster of ductal epithelial cells with no cytological atypia and abundant myoepithelial cells (Pap stain; 40X); b) Corresponding histopathologic lesion diagnosed as Fibrocystic disease (H&E stain; 4X); c) Ductal epithelial cells along with many myoepithelial cells (MGG stain; 40X); d) Corresponding histopathologic lesion diagnosed as Fibroadenoma (H&E stain; 4X).
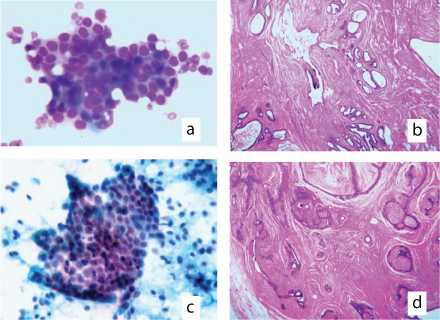
In 50/207 cases, the cytologic findings indicated NPBD and the histologic diagnosis agreed in 38 cases. The rest 12 cases with discrepancy were included in proliferative breast disease without atypia, histologically. Of these 12 cases, 9 had a score of 9 or 10 by MSI, thereby shifting those 9 cases to proliferative disease without atypia by MMSI. The remaining three discrepant cases included one case of phyllodes tumour and two cases of fibroadenoma. In 41/50 cases both the systems gave same score.
Proliferative Breast Disease (PBD) without Atypia
Cytomorphological features of this group are presented in [Table/Fig-6]. A 55 (26.57%) of cases were cytologically diagnosed as PBD without atypia, out of which histologic diagnosis agreed in 51 cases. The four cases with discrepancy included PBD with atypia in one case, microscopic foci of IDC in two cases and one case of Mucinous carcinoma by histologic examination. To these, 9 cases were added from group I by MMSI, all of which were concordant with histopathology.
PBD with Atypia
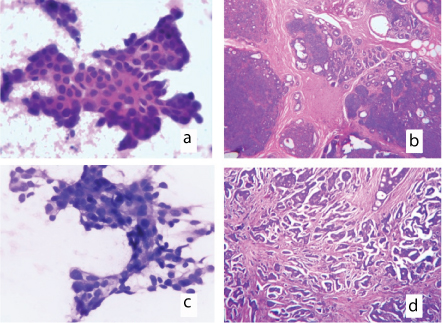
Cytomorphological features of this group are presented in [Table/Fig-7]. Fifteen (7.25%) cases showed proliferative breast disease with atypia by both scoring methods out of which 9 cases were concordant with histologic diagnosis (60%). Two cases reported as carcinoma by histology were missed by cytology. The remaining four cases with discrepancy included three cases of Epithelial Proliferative Breast Lesion (EPL) with apocrine metaplasia and one case of EPL with lactational change by histologic examination.
a) Ductal epithelial cells showing nuclear crowding, cytonuclear atypia with conspicuous micronucleoli and occasional myoepithelial cells (Pap stain;40X); b) Corresponding histopathologic lesion diagnosed as Atypical ductal hyperplasia (H&E stain; 4X); c) Ductal epithelial cells showing marked anisonucleosis, irregular coarse chromatin with frequent micronucleoli, macronucleoli and absent myoepithelial cells (MGG stain; 40X); d) Corresponding histopathologic lesion diagnosed as Invasive ductal carcinoma (H&E stain; 4X).
Carcinoma in situ/Invasive Carcinoma
Cytomorphological features of this group are presented in [Table/Fig-7]. Of 87 cases (42.03%) diagnosed as carcinoma in situ/Carcinoma by cytology, 2 were histologically diagnosed as Ductal Carcinoma in situ (DCIS) and 85 were carcinoma. There was 100% agreement between cytology and histopathology in category 4.
Concordance between Cytological and Histopathological Diagnosis
Concordance analysis was done between cytological and histological diagnosis and the results were expressed in percentages. The Fisher’s-exact test was done to assess the statistical significance of the differences in the concordance obtained by MSI versus MMSI. We found a statistically significant (p=0.046) higher concordance rate (92.68%) for category 1 of MMSI as compared to MSI (76%). Additionally, Cohen’s Kappa coefficients were estimated to assess the agreement between cytological scoring methods and histopathology across all the diagnostic categories. MMSI showed better agreement with histopathology (κ = 0.91 CI {0.85 – 0.95}) than MSI (κ = 0.84 CI {0.78 – 0.90}).
Diagnostic Accuracy of Cytological Scoring
The parameters of diagnostic accuracy were computed by categorizing the cases based on presence or absence of carcinoma. The overall diagnostic accuracy was 97.5% with sensitivity of 94.5% and specificity of 100%. The positive and negative predictive values were 100% and 95.83% respectively [Table/Fig-8].
A 2X2 contingency table of carcinoma cases categorized by FNAC and biopsy.
| Excision Biopsy |
|---|
| Fnac | Positive | Negative |
|---|
| Positive | 87 | 0 |
| Negative | 5 | 115 |
Sensitivity 94.5%, Specificity 100%, Overall diagnostic accuracy 97.5%, Positive predictive value 100%, Negative predictive value 95.83%.
Discussion
The present study was conducted in 207 patients with palpable breast lumps. This study was undertaken to determine whether the defined cytological criteria used in MSI and MMSI can be as effective as open biopsy in stratifying the risk for developing carcinoma in palpable breast lesions on the basis of established histopathologic determinants and also to assess the concordance between cytological scoring with reference to histopathology.
We found that the six parameters proposed by Masood et al., were useful features for cytological scoring of breast lesions. These were consistent with findings in Masood’s study [18]. This demonstrates that the MSI allows an accurate and reproducible diagnosis of the standard histopathologic categories of benign and neoplastic breast diseases. It can also serve as a guide for separating nonproliferative from proliferative breast disease with and without atypia.
Nandini et al., in their study concluded that a slight modification in the MSI by shifting score 9 and 10 of NPBD to PBD without atypia, will increase the diagnostic accuracy of first two categories of MSI [20]. Our study also showed a statistically significant higher concordance rate (92.68%) for category 1, cytologically diagnosed by MMSI as compared to MSI (76%). The category 2 based on MMSI also showed a higher concordance rate than MSI even though it was not statistically significant. Thus, MMSI was found to be more useful index compared to MSI, and improves the diagnostic accuracy of NPBD and PBD without atypia cases. This is important as the prognosis and treatment of these cases varies.
In category 1, out of 50 cases, we got discrepant results by MSI in 12 cases, thus reducing its accuracy to 76%, while Masood, in her study got an accuracy of 90%. This disparity may be accounted to the differences in the sample size; 80 (Masood’s study) when compared to 207 in the present study. Out of these 12 cases of discrepancy, 9 were shifted to category 2 by MMSI, which increased the diagnostic accuracy of category 1. This diagnostic accuracy was comparable with the observation by Nandini et al. Rest of the three discrepant cases in this category included two cases of fibroadenoma and one case of Phyllodes Tumour (PT). PT has been wrongly categorised into category 1 by both MSI and MMSI due to absence of criterion for stromal component evaluation. The rest two cases of typical FA were missed by MSI as well as MMSI in this study and were placed in category 1. Inclusion of cellularity as one of the criteria might be useful in such cases for accurate categorization as proliferative lesions.
In category 2, four discrepant cases were there, one case each of PBD with atypia and mucinous carcinoma and two cases of Invasive ductal carcinoma. Since Masood’s criteria doesn’t include cellularity and background material as parameters, there is a great chance of mucinous carcinoma being mistakenly categorized as a benign lesion by MSI, as occurred in the present study. The other two cases of invasive carcinoma were microscopic foci and the needle might not have hit the malignant focus.
Maximum number of discrepant cases was found in category 3 which included, two cases of carcinoma, three cases of EPL with apocrine metaplasia and one case of EPL with lactational change by histologic examination. Apocrine metaplastic cells often cause concern due to moderate atypia and can be the cause of false-positive diagnosis in cytology [23]. Masood scoring index gave a score of 15 and 16 for those three cases of apocrine metaplasia, finally placing it in PBD with atypia category, whereas it actually belongs to the category 1 or 2. Similar observation was also made by Makunura et al., in his study [23]. Another area of concern was accurate cytological diagnosis of EPL cases with lactation change. The pattern seen in FNAC smears of ‘lumps’ in a pregnant or lactating breast can be problematic most of the time and causes concern for malignancy. A milky background in smears would have aided in diagnosing lactational change, but unfortunately background is not a parameter in MSI. However, a clinical correlation and ultrasonography may help us in identifying such false positive cases. The two discrepant cases of invasive carcinoma encountered in this group were of low grade in histopathology, which still remains a ‘grey zone’ area in cytology. We also found that both the cases had a score of 18 by MSI, which is the highest score in the respective category and rest all had a score below 18. Therefore, a change in the scoring indices by shifting score 18 to category 4, thereby modifying score for PBD with atypia as 15 to 17 and Carcinoma as 18 to 24, may probably resolve this issue. However, this needs to be evaluated with a higher sample size to prove conclusively.
In category 4, no histologically diagnosed Carcinoma in situ and Carcinoma cases were missed cytologically using MSI; thus there were no false-positive results in this study, which is generally considered to be the most important error to be avoided, especially if definitive treatment to be undertaken is solely on the basis of cytology. The concordance rate of this category was 100%, which is similar to that discussed by Masood et al., and Nandini et al., in their studies. Also, the study confirmed that MSI/MMSI is a specific test (specificity 100%) to predict malignant lesion correctly (PPV 100%). The sensitivity and negative predictive value in finding malignancy in cytology by MSI were 94.5% and 95.83% respectively, with an overall diagnostic accuracy of 97.5%. These results were found to be comparable with the pioneer studies.
Limitation
The limitations of the present study primarily include reporting of cytology and histopathology by single observer and relatively smaller number of samples in PBD with atypia category in comparison to other categories.
Conclusion
The present study concludes that Modified Masood scoring index has better diagnostic accuracy than conventional Masood scoring index in the cytological diagnosis of palpable breast lump aspirates.
NPBD – Non proliferative breast disease, PBD – Proliferative breast disease.
NPBD – Non proliferative breast disease, PBD – Proliferative breast disease