Introduction
Periodontal disease is characterised by chronic infection and inflammation in periodontal tissues leading to destruction of alveolar bone with subsequent tooth loss. Periodontal infections are the result of an interaction between tooth associated microbial biofilms and the host defences. Periodontal pathogens can affect local and systemic immune and inflammatory responses.
Aim
The aim of the present study was to evaluate serum C-Reactive Protein (CRP), plasma fibrinogen and peripheral blood levels in healthy subjects, chronic and aggressive periodontitis patients.
Materials and Methods
A total of 55 subjects, 27 males and 28 females were selected for the study. Blood samples were taken from healthy controls (n=20) and patients with chronic periodontitis (n=20) and aggressive periodontitis (n=15). The periodontal status of each patient was assessed by recording Oral Hygiene Index-Simplified (OHI-S), Bleeding Index (BI), Probing Pocket Depth (PPD) and Clinical Attachment Level (CAL). The levels of serum CRP were measured using high sensitivity Enzyme Linked Immunosorbent Assay (ELISA) and levels of plasma fibrinogen were measured using Quantitative Immunoturbidimetric assay. Data description was done in the form of mean and standard deviation and analysis of data was done using one way ANOVA (Analysis of Variance) and Students t-test to test the statistical significance between groups.
Results
The levels of serum CRP and plasma fibrinogen was increased in patients with chronic and aggressive periodontitis when compared to healthy controls (p<0.001). A positive correlation was found to exist between levels of clinical parameters like OHI-S, BI, PPD and CAL when compared with CRP and fibrinogen as well as with the study groups.
Conclusion
The finding of the present study suggests the role of serum as a diagnostic marker in inflammatory conditions and indicates that levels of CRP and fibrinogen may serve as important biomarkers for evaluating the association between periodontitis and cardiovascular diseases.
Introduction
Periodontal disease is characterised by chronic infection and inflammation in periodontal tissues leading to destruction of alveolar bone with subsequent tooth loss [1]. Periodontal infections are the result of an interaction between tooth associated microbial biofilms and the host defences. There is growing evidence that these chronic infections can go beyond the periodontium and predispose to various systemic diseases [2].
Periodontitis has been linked to atherosclerosis and cardiovascular diseases based on various cross-sectional and prospective epidemiological studies [3,4]. Subgingival dental plaque contains numerous Gram-negative anaerobic pathogenic bacteria in deep periodontal pockets. These pathogenic microrganisms produce various endotoxins such as lipopolysaccharides, leucotoxins and chemotactic inhibiting factors which can result in an increase in circulating levels of cytokines, adhesive proteins and proinflammatory molecules. These endotoxins can interact with toll-like receptors present on the surface of neutrophils and monocytes resulting in activation of signal transduction pathways in both innate and adaptive immune systems. These mechanisms leads to the production of pro-inflammatory cytokines like Interleukin-6 (IL-6), Interleukin-1 (IL-1) and Tumour Necrosis Factor-α (TNF-α) that can activate hepatocytes in the liver to produce acute phase proteins including CRP [5,6]. Elevated levels of pro-inflammatory cytokines as well as pathogenic bacteria can be translocated through systemic circulation resulting in direct exacerbation of cardiovascular disease or influencing other systemic risk factors associated with cardiovascular disease [5,7].
Acute Phase Response (APR) is a non specific process that may occur as initial host response to injuries, infections, ischemic necrosis or malignancy. Acute phase proteins are those proteins whose plasma concentration is altered (increases or decreases) by atleast 25% in response to inflammation [8]. Acute phase proteins have both pro and anti-inflammatory properties. This systemic response helps to destroy infections or noxious agents, remove damaged tissue and repair the affected tissue or organ. These acute phase proteins have been found to have an essential role in the inhibition of extracellular proteases, blood clotting, fibrinolysis, and modulation of immune cell function [9].
CRP production is a part of non specific APR to most forms of inflammatory stimuli such as heat, infection, hypoxia and tissue damage. Even though CRP is primarly synthesized by hepatocytes, extra hepatic sources include alveolar macrophages, coronary artery, peripheral blood lymphocytes, adipose tissue and lung epithelial cells. Factors such as smoking, cardiovascular diseases, triglycerides, diabetes and periodontal disease have been found to be associated with raised CRP levels [10]. In healthy individuals, CRP levels were found to be ≤ 0.3 mg/l. Serum levels of CRP could exceed 100 mg/l following acute tissue damage in serum or plasma within 24 to 48 hours which could be useful for diagnosis, monitoring and therapy of inflammatory process and associated disease [11].
Fibrinogen an important determinant of blood viscosity is a soluble plasma glycoprotein that is synthesized by liver and is converted into fibrin by thrombin during coagulation of blood. Fibrinogen can promote early plaque formation through damaging the endothelial cells of artery linings, stimulating the proliferation of vascular muscle cells and activating inflammatory cells. Fibrinogen also plays an important role in thrombosis by influencing platelet adhesion and aggregation [12]. The normal fibrinogen levels have been found to be about 1.5-3 g/l while increased levels have been found to be associated with cardiovascular disease (≥3.43 g/l). An elevated fibrinogen level can therefore predispose to platelet aggregation and thrombosis thereby increasing predisposition for coronary heart disease [13,14].
One of the major causes of mortality and morbidity worldwide has been found to be Coronary Artery Disease (CAD). Even though various risk factors such as diabetes mellitus, hypertension and smoking has been identified, periodontal disease has been found to provide vital information regarding elevated risk of CAD. CRP has been found to be a valuable predictor for Myocardial Infarction (MI), atherosclerotic lesions, stroke, peripheral vascular disease and sudden cardiac death as shown in multiple prospective epidemiological studies [3,15]. Elevated inflammatory and homeostatic responses as well as lipid metabolism due to periodontal infection might be possible pathways underlying the observed association between periodontal disease and increased risk for CVD [16].
Therefore, this study was carried out to assess the levels of serum CRP, plasma fibrinogen and periodontal parameters in systemically and periodontally healthy individuals and patients with chronic and aggressive periodontitis and to determine whether raised levels of periodontal parameters can predispose to increased levels of systemic inflammatory markers such as serum CRP and plasma fibrinogen of the three study groups.
Materials and Methods
The present study was conducted in the Department of Periodontology, Rajah Muthiah Dental College and Hospital with the help of Department of Biochemistry, Rajah Muthiah Dental College and Hospital, Annamalai University, Tamil Nadu, India. This was a cross- sectional descriptive study which was carried out for a period of six months. Participants were interviewed to obtain medical and demographic information and were screened for periodontal examination. All periodontal clinical parameters were evaluated by a single calibrated investigator. A total of 55 subjects were selected for the study with 27 males and 28 females which included 20 controls, 20 patients with chronic periodontitis and 15 patients with aggressive periodontitis (five localized and 10 generalized aggressive periodontitis).
Since there were constraints in obtaining aggressive periodontitis patients (localized and generalized) within time period of the study (six months), their sample size had to be restricted to 15. Therefore, the control and the chronic periodontitis group had to be limited to 20 each.
The nature and purpose of study was explained to the patient and an informed consent was obtained. This study was put forward before the Ethical Committee and clearance was obtained.
Subjects for this study comprised of:
Group A: Systemically healthy controls- Age group; 25-45 years. Individuals with PPD ≤3 mm, CAL <2 mm with no clinical signs of inflammation.
Group B: Chronic periodontitis patients- Age group; 30-45 years. Individuals having more than 30% of their teeth with PPD ≥4 mm, CAL ≥2 mm.
Group C: Generalized and localized aggressive periodontitis patients- Age group; 20-35 years. Individuals having a minimum of 20 remaining teeth with a pattern of generalized interproximal attachment loss affecting at least three permanent teeth other than first molars and incisors (generalized aggressive periodontitis)/localized first molar or incisor presentation with interproximal attachment loss on at least two permanent teeth, one of which is a first molar and involving not more than two teeth other than first molars and incisors and microbial deposits which are inconsistent with respect to the degree of periodontal destruction [17].
Systemically healthy individuals of both genders, dentition with at least 20 functioning teeth, those who were not under any antibiotics, systemic steroids or anti-inflammatory drugs and had not undergone any periodontal therapy six months prior to and during the period of study were included in the study. Subjects who were alcoholics, smokers and pregnant females were excluded.
Clinical parameters recorded were;
OHI-S (Green and Vermillion 1964) [18];
Gingival Bleeding Index (Ainamo and Bay 1975) [19];
PPD;
CAL.
Estimation of Peripheral Blood, Serum CRP and Plasma Fibrinogen
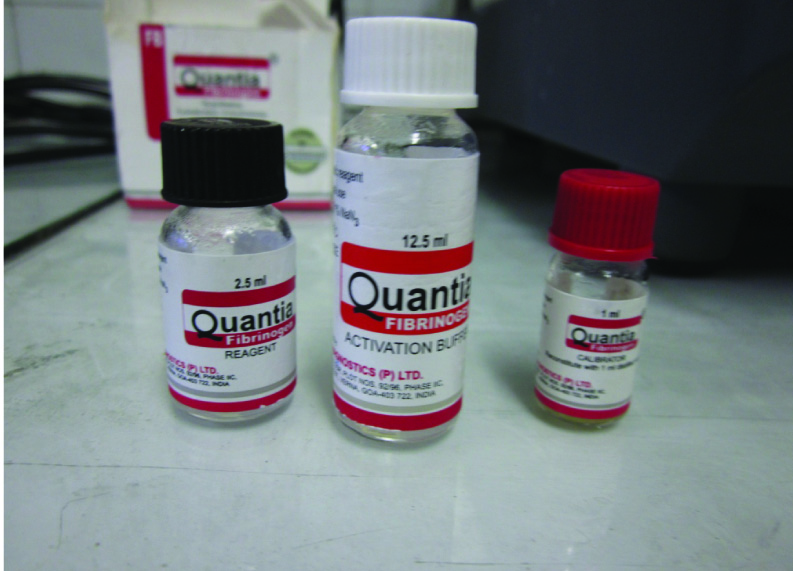
Subject consent was taken prior to the collection of samples. Almost 5 ml of blood was collected in the morning hours from anticubital fossa by venipuncture using 20 gauge needles with a 5 ml syringe. The blood was transferred to non-ethylene diamino tetra-acetic acid containing test tubes and was allowed to clot at room temperature and after one hour, serum and plasma were extracted from the blood by centrifuging at 3000 rpm for five minutes. Extracted serum and plasma were immediately transferred to Eppendorf vials and stored at -20OC till the time of assay [Table/Fig-1,2].


Samples were then assayed for CRP (high sensitivity–CRP) using ELISA Kit (The EiAsy Way, Diagnostics Biochem Canada Inc [Table/Fig-3]). The serum levels of high sensitivity-CRP was measured using ELISA technique which is an enzymatically amplified “two step” sandwich type immunoassay where the standard samples, control samples and unknown samples were incubated in microtitration wells coated with high sensitivity-CRP antibody.
High sensitivity-CRP reagents.

Quantitative Immunoturbidimetric assay (Quantia fibrinogen) was used for estimation of fibrinogen in collected plasma and is based on agglutination reaction [Table/Fig-4]. The test specimen was mixed with QUANTIA–fibrinogen antibody reagent (R2) and activation buffer (R1) and allowed to react. Presence of fibrinogen in the test specimen resulted in formation of an insoluble complex with an increase in turbidity, which was measured at a wavelength of 340 nm. The increase in turbidity corresponds to the concentration of fibrinogen in the test specimen.
Statistical Analysis
All the data were analysed using SPSS package version 14.0 software programs. Data description was done in the form of mean and standard deviation; and analysis of data was done to test the statistical significance between groups. One way ANOVA (Analysis of Variance) was applied to compare the mean values of OHI-S, BI, PPD, CAL, CRP, fibrinogen among three groups. Students t-test was applied to compare the mean values of OHI-S, BI, PPD, CAL, CRP, fibrinogen between two groups. A p-values < 0.05 was considered to be statistically significant.
Results
In the present study, mean OHI-S, BI score, mean PPD level and CAL was found to be higher in patients with chronic periodontitis when compared to patients with aggressive periodontitis and systemically and periodontally healthy subjects [Table/Fig-5].
One-way ANOVA test showing mean and standard deviation of OHI-S, BI, PPD level, CAL, CRP, and fibrinogen level between three groups.
| Parameters | Groups | N | Mean | SD | F-value | p-value |
|---|
| OHI-S | A | 20 | 0.62 | 0.22 | 9.83 | <0.001 (Highly significant) |
| B | 20 | 4.00 | 0.61 |
| C | 15 | 2.27 | 0.49 |
| BI | A | 20 | 0.440 | 0.660 | 42.31 | <0.001(Highly significant) |
| B | 20 | 85.120 | 6.067 |
| C | 15 | 69.013 | 8.123 |
| PPD | A | 20 | 2.375 | 0.297 | 11.32 | <0.001(Highly significant) |
| B | 20 | 5.735 | 0.854 |
| C | 15 | 5.527 | 0.446 |
| CAL | A | 20 | 0.00 | 0.00 | 24.86 | <0.001(Highly significant) |
| B | 20 | 5.93 | 0.39 |
| C | 15 | 5.41 | 0.81 |
| CRP | A | 20 | 1112.35 | 390.38 | 8.69 | <0.004(Highly significant) |
| B | 20 | 3397.00 | 2511.77 |
| C | 15 | 2692.27 | 2585.64 |
| Fibrinogen | A | 20 | 337.50 | 158.33 | 6.40 | <0.001(Highly significant) |
| B | 20 | 763.90 | 247.39 |
| C | 15 | 616.53 | 189.49 |
In the present study, mean CRP levels were found to be higher in patients with chronic periodontitis (3397.00±2511.77 ng/ml) when compared with aggressive periodontitis patients (2692.27±2585.64 ng/ml) and periodontally healthy subjects (1112.35±390.38 ng/ml; p<0.004) [Table/Fig-5]. Similarly, mean fibrinogen level was found to be higher in patients with chronic periodontitis (763.90±247.39 μg/ml) when compared to patients with aggressive periodontitis (616.53±189.49 μg/ml) and periodontally healthy subjects (337.50±158.33 μg/ml; p<0.001) [Table/Fig-5].
Intergroup comparison using students t-test, for CRP levels, fibrinogen levels and periodontal parameters between the three groups has been shown in [Table/Fig-6,7,8,9 and 10].
Students t-test comparing CRP and fibrinogen level between Group B and Group C.
| Parameters | Groups | N | Mean | SD | p-value |
|---|
| CRP | B | 20 | 3397.00 | 2511.77 | Not Significant |
| C | 15 | 2692.27 | 2585.64 |
| Fibrinogen | B | 20 | 763.90 | 247.39 | Not Significant |
| C | 15 | 616.53 | 189.49 |
Students t-test comparing CRP and fibrinogen level between Group A and Group B.
| Parameters | Groups | N | Mean | SD | p-value |
|---|
| CRP | A | 20 | 1112.35 | 390.38 | <0.001 (Highly significant) |
| B | 20 | 3397.00 | 2511.77 |
| Fibrinogen | A | 20 | 337.50 | 158.33 | <0.001(Highly significant) |
| B | 20 | 763.90 | 247.39 |
Students t-test comparing CRP and Fibrinogen Level Between Group A and Group C.
| Parameters | Groups | N | Mean | SD | p-value |
|---|
| CRP | A | 20 | 1112.35 | 390.38 | <0.001 (Highly significant) |
| C | 15 | 2692.27 | 2585.64 |
| Fibrinogen | A | 20 | 337.50 | 158.33 | <0.001(Highly significant) |
| C | 15 | 616.53 | 189.49 |
Students t-test comparing different periodontal parameters between Group A and Group B.
| Periodontal Parameters | Groups | N | Mean | SD | p-value |
|---|
| OHI-S | A | 20 | 0.62 | 0.22 | <0.001 (Highly significant) |
| B | 20 | 4.00 | 0.61 |
| BI | A | 20 | 0.440 | 0.611 | <0.001(Highly significant) |
| B | 20 | 85.120 | 6.067 |
| PPD | A | 20 | 2.375 | 0.297 | <0.001(Highly significant) |
| B | 20 | 5.735 | 0.854 |
| CAL | A | 20 | 0.00 | 0.00 | <0.001(Highly significant) |
| B | 20 | 5.93 | 0.39 |
Students t-test comparing different periodontal parameters between Group A and Group C.
| PeriodontalParameters | Groups | N | Mean | SD | p-value |
|---|
| OHI-S | A | 20 | 0.62 | 0.22 | <0.001 (Highly significant) |
| C | 15 | 2.27 | 0.49 |
| BI | A | 20 | 0.440 | 0.611 | <0.001(Highly significant) |
| C | 15 | 69.013 | 8.132 |
| PPD | A | 20 | 2.375 | 0.297 | <0.001(Highly significant) |
| C | 15 | 5.527 | 0.446 |
| CAL | A | 20 | 0.00 | 0.00 | <0.001(Highly significant) |
| C | 15 | 5.41 | 0.18 |
Discussion
Periodontitis is an infectious disease of the supporting tissues of the teeth, characterized by gradual loss of tooth supporting alveolar bone. Once initiated, periodontal disease maintains a slowly progressive and destructive character with periods of exacerbation and remission. Factors contributing to periodontal disease include oral hygiene, individual host response and resident microflora. The inflammatory process in periodontitis can involve vasculature directly by interaction of organisms or bacterial byproducts within vessel wall or indirectly through modulation of haemostasis or hepatic activation of acute phase response that leads to increased circulation of acute phase reactants such as CRP [20]. Elevated CRP has been found to be a significant risk factor for atherosclerosis, cardiovascular disease and type 2 diabetes [21]. Fibrinogen in excessive levels can also increase proinflammatory cytokines such as IL-6 and TNF-α, promote colonization and attachment of bacteria as well as migration of leukocytes at the site of inflammation [22].
Two hypothesis have been proposed regarding the aetiological pathways of the association between periodontitis, systemic inflammation and cardiovascular disease. In direct pathways, oral microbes and their byproducts gain systemic access through the circulating system. The indirect pathways, considers the diseased periodontium as a source of systemic inflammatory mediators. Chronically elevated CRP levels in periodontitis patients exacerbate ongoing inflammatory processes in atherosclerotic lesions, thereby increasing the risk of cardiovascular and cerebrovascular events [23]. Therefore, measurement of serum acute phase proteins may help to identify a subset of patients who are at higher risk for destructive disease or reveal those patients who are undergoing a process of periodontal breakdown [24].
In the present study, mean CRP levels were found to be higher in patients with chronic periodontitis when compared with aggressive periodontitis patients and periodontally healthy subjects. This is in accordance with studies done by Rai B et al., and Gani DK et al., who found elevated levels of mean CRP in patients with periodontitis [25,26]. A possible reason for the elevation of serum CRP may be its role in initial host response to injuries, infections, ischemic necrosis or malignancy where it helps to destroy infections or noxious agents, to remove damaged tissue and to repair affected tissue or organ. In the present study, mean fibrinogen level was found to be higher in patients with chronic periodontitis when compared to patients with aggressive periodontitis and periodontally healthy subjects. This is in accordance with studies done by Sahingur SE et al., who found elevated levels of mean fibrinogen in periodontitis patients when compared with the control group [22]. A possible reason for the increase may be that, a higher percentage of patients with chronic periodontitis exhibit H1H2 or H2H2 genotypes which were found to be associated with higher fibrinogen levels when compared with healthy individuals [22]. There is a strong association of fibrinogen with blood viscosity and thrombus formation and circulating levels of fibrinogen have been known to have a strong relationship with coronary artery disease [27,28]. In the present study, no statistically significant results were obtained when CRP and fibrinogen were compared in patients with chronic and aggressive periodontitis. High CRP levels (42.1 mg/l) were found to be associated with higher incidence of stroke and myocardial infarction. It may be speculated, that periodontitis may predispose affected patients to cardiovascular diseases by increasing the levels of acute phase proteins which may lead to increased inflammatory activity in atherosclerotic lesions [26].
The effect of periodontal treatment on systemic levels of inflammatory markers CRP and fibrinogen has been investigated through various studies. The effects of non surgical periodontal treatment on plasma levels of fibrinogen in patients with periodontitis and arterial hypertension was done by Vidal F et al., and results obtained showed significant reduction in the blood levels of fibrinogen [29]. Recent trials have shown that treatment of periodontal infections either by mechanical therapy, drug therapy or extraction can lower the serum levels of CRP. Mattila K et al., conducted a study on 35 patients with adult periodontitis and after treatment results showed significant decrease in CRP levels after treatment [30]. A median decrease of 0.5 mg/l in serum CRP was noted six months after completion of periodontal therapy by D’Aiuto F et al., [31]. Therefore, periodontal therapy has been found to be effective in reducing bacterial load in deep pockets thereby decreasing infection and local inflammation and improving periodontal clinical parameters.
In the present study, mean CRP and fbrinogen levels were slightly higher in chronic periodontitis individuals when compared with aggressive periodontitis individuals and this mean difference was statistically not significant. A reason for the slight increase in CRP levels in chronic periodontitis group may be due to its long standing nature when compared with aggressive periodontitis group although the exact cause have not been fully understood [32].
The findings of the present study supports the fact that levels of serum CRP and plasma fibrinogen were increased in individuals with periodontitis when compared with normal individuals and elevated levels of these inflammatory markers can increase the severity of periodontal destruction as observed with raised periodontal parameters.
Limitation
The small sample size due to strict guidelines for recruiting patients, along with the absence of post treatment results pose limitations in evaluating the relationship of these biomarkers with periodontal and cardiovascular diseases. Systemic conditions such as diabetes and infectious conditions were excluded purely on the basis of self reported histories and there is a possibility that this might have led to undiagnosed medical conditions. Estimation of other sensitive markers like serum amyloid A and α-2 macroglobulin from serum and plasma as well as estimation of CRP in saliva and gingival crevicular fluid would provide greater clarity and understanding between these biomarkers, periodontal and cardiovascular diseases.
Conclusion
An increase in levels of serum CRP and plasma fibrinogen were observed in both study groups when compared to healthy controls. An increase in level of mean serum CRP and plasma fibrinogen were observed in chronic and aggressive periodontitis group when compared to control group and this was found to be statistically significant (p<0.001). A positive correlation exists between levels of clinical parameters like OHI-S, BI, PPB, CAL and the study groups. A positive correlation exists between levels of CRP and fibrinogen and all periodontal parameters under study.
From the results of the above study, it could be assumed that levels of serum CRP and plasma fibrinogen can provide information about the presence and intensity of inflammatory process and can be useful in predicting biological mechanism underlying the association between periodontitis and cardiovascular diseases. Elevated CRP and fibrinogen levels can be used as a predictive risk factor for future cardiovascular and coronary events. Further studies with large sample size, allowing incorporation of periodontal treatment phase and correlating periodontal microbes with the levels of expression of serum CRP and plasma fibrinogen are necessary to validate the results of the present study.
[1]. Kinane DF, Causation and pathogenesis of periodontal diseasePeriodontol 2000 2001 25:8-20. [Google Scholar]
[2]. Offenbacher S, Madianos PN, Champagne CM, Southerland JH, Paquette DW, Williams RC, Periodontitis-atherosclerosis syndrome: An expanded model of pathogenesisJ Periodontal Res 1999 34:346-52. [Google Scholar]
[3]. Emingil G, Buduneli E, Aliyev A, Akilli A, Atilla G, Association between periodontal disease and acute myocardial infarctionJ Periodontol 2000 71:1882-86. [Google Scholar]
[4]. Haraszthy VI, Zambon JJ, Trevisan M, Zeid M, Genco RJ, Identification of periodontal pathogens in atheromatous plaquesJ Periodontol 2000 71:1554-60. [Google Scholar]
[5]. Williams RC, Offenbacher S, Periodontal MedicinePeriodontol 2000 2000 23:9-156. [Google Scholar]
[6]. Al-Zahrani MS, Bissada NF, Borawski EA, Obesity and periodontal disease in young, middle-aged and older adultsJ Periodontol 2003 74:610-15. [Google Scholar]
[7]. Deshpande RG, Khan MB, Genco RJ, Invasion of aortic and heart endothelial cell by P.gingivalisInfect Immun 1998 66:5337-43. [Google Scholar]
[8]. Gruys E, Toussaint MJ, Niewold TA, Koopmans SJ, Acute phase reaction and acute phase proteinsJ Zhejiang Univ Sci B 2005 6(11):1045-56. [Google Scholar]
[9]. Ebersole JL, Cappelli D, Acute–phase reactants in infections and inflammatory diseasesPeriodontol 2000 2000 23:19-49. [Google Scholar]
[10]. Gomes-Filho IS, Coelho JMF, da Cruz SS, Passos JS, Teixeira de Freitas CO, AraqaoFarias NS, Chronic periodontitis and C-reactive protein levelsJ Periodontol 2011 87(7):969-78. [Google Scholar]
[11]. Iwamoto Y, Nishimura F, Soga Y, Takeuchi K, Kurihara M, Takashiba S, Antimicrobial periodontal treatment decreases serum C-reactive protein, tumor necrosis factor-alpha, but not adiponectin levels in patients with chronic periodontitisJ Periodontol 2003 74(8):1231-36. [Google Scholar]
[12]. Wu T, Trevisan M, Genco RJ, Dorn JP, Falkner kl, Sempos CT, Examination of the reaction between Periodontal health status and Cardiovascular risk factors: serum total and high density lipoprotein cholesterol, C-reactive protein and plasma fibrinogenAm J Epidemol 2000 151(3):273-82. [Google Scholar]
[13]. Hantgan RR, Francis CW, Fibrinogen structure and physiology. In:Marder VJ, Aird WC, Bennett JS, Schulman’s, White GC edsHemostasis and thrombosis: Basic principles and clinical practice 1994 Lippincott Williams & Wilkins:277-300. [Google Scholar]
[14]. van der Bom JG, De Maat MP, Bots ML, Kluft C, Grobbee DE, Seasonal variation in fibrinogen in the Rotterdam studyThromb Heamost 1997 78:1059-62. [Google Scholar]
[15]. Tousoulis D, Davies G, Stefanadis C, Toutouzas P, Ambrose JA, Inflammatory and thrombotic mechanisms in coronary atherosclerosisHeart 2003 89:993-97. [Google Scholar]
[16]. Al-Rasheed A, Elevation of white blood cells and platelet counts in patients having chronic periodontitisSaudi Dent J 2012 24:17-21. [Google Scholar]
[17]. Newman GM, Takei HH, Klokkevold PR, Carranza FA, Carranza’s Clinical PeriodontologyVol 10:507-09. [Google Scholar]
[18]. Shabani LF, Begzati A, Dragidella F, Hoxha VH, Cakolli VH, Bruci B, The correlation between DMFT and OHI-S Index among 10-15-year-old children in KosovaJournal of Dental and Oral Health 2015 1(1):1-5. [Google Scholar]
[19]. Rebelo MAB, de Queiroz AC, Gingival Indices: State of Artwww.intechopen.com 41-54 [Google Scholar]
[20]. Radafshar G, Shad B, Mirfeizi M, Association between periodontal disease and elevated C-Reactive Protein in acute myocardial infarction patientsJournal of Dentistry 2006 3(3):129-34. [Google Scholar]
[21]. Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM, C-reactive protein, Interleukin 6 and risk of developing type 2 diabetes mellitusJAMA 2001 286:327-34. [Google Scholar]
[22]. Sahingur SE, Sharma A, Genco RJ, De Nardin E, Association of increased levels of fibrinogen and -455G/A fibrinogen gene polymorphism with chronic periodontitisJ Periodontol 2003 74:329-37. [Google Scholar]
[23]. Haynes WG, Stanford C, Periodontal disease and atherosclerosis from dental to arterial plaqueArterioscler Thromb Vase Biol 2003 23:1309-11. [Google Scholar]
[24]. Ebersole JL, Cappelli D, Mathys EC, Steffen MJ, Singer RE, Montgomery M, Periodontitis in humans and non-human primates: Oral-systemic linkage including acute phase proteinsAnn Periodontol 2002 7(1):102-11. [Google Scholar]
[25]. Rai B, Kharb S, Jain R, Anand SC, Periodontitis, C-Reactive Protein and Peripheral Blood;Links with Cardiovascular DiseaseAdvances in Medical and Dental Sciences 2010 3(3):76-79. [Google Scholar]
[26]. Gani DK, Lakshmi D, Krishnan R, Emmadi P, Evaluation of C-reactive protein and Interleukin-6 in peripheral blood of patients with chronic periodontitisJ Indian Soc Periodontol 2009 13(2):69-74. [Google Scholar]
[27]. Iyer UM, Desai P, Assessment of C-Reactive Protein and fibrinogen levels in type 2 diabetes mellitusBiomedical Research 2010 21(2):208-13. [Google Scholar]
[28]. Schwahn C, Volzke H, Robinson DM, Luedemann J, Berhardt O, Gesch Periodontal disease, but not edentulism, is independently associated with increased plasma fibrinogen levels. Results from a population based studyThromb Haemost 2004 92:244-52. [Google Scholar]
[29]. Vidal F, Figueredo CM, Cordovil I, Fischer RG, Periodontal therapy reduces plasma levels of interleukin -6, C-reactive protein and fibrinogen in patients with severe periodontitis and refractory arterial hypertensionJ Periodontol 2009 80:786-91. [Google Scholar]
[30]. Mattila K, Vesanen M, Valtonen V, Nieminen M, Palosuo T, Rasi V, Effect of treating periodontitis on C-reactive protein levels: A pilot studyBMC Infect Dis 2002 2:30 [Google Scholar]
[31]. D’Aiuto F, Parkar M, Andreaou G, Brett PM, Ready D, Tonetti MS, Periodontitis and atherogenesis: Casual association or simple coincidenceJ Clin Periodontol 2004 31:402-11. [Google Scholar]
[32]. Kanaparthy A, Kanaparthy R, Niranjan N, Evaluation of serum C-reactive protein levels in subjects with aggressive and chronic periodontitis and comparison with healthy controlsDent Res J 2012 9(3):261-65. [Google Scholar]