Introduction
Acute and chronic urticaria can result in severely impaired quality of life from pruritus and associated sleep lessness, as well as anxiety and depression. Various treatment modalities are available out of which second generation non sedating H1 antihistamines e.g., fexofenadine, loratidine, desloratadine, cetirizine, levocetirizine, ebastine etc., are used as the first line treatment.
Aim
To compare the safety and efficacy of ebastine 20 mg, ebastine 10 mg and levocetirizine 5 mg in the patients of urticaria
Materials and Methods
A longitudinal study was conducted in dermatology Outpatient Department (OPD) of Adesh Institute of Medical Sciences and Research, Bathinda, India. A total of 150 patients between the age group 10-70 years, both men and women having urticaria were enrolled and divided into three groups of 50 each. Group A was given ebastine 20 mg OD, Group B was given ebastine 10 mg OD and Group C was given levocetirizine 5 mg OD. The patients were asked to scale their severity of disease over a period of follow up based on Urticarial Activity Score 7 (UAS7).
Results
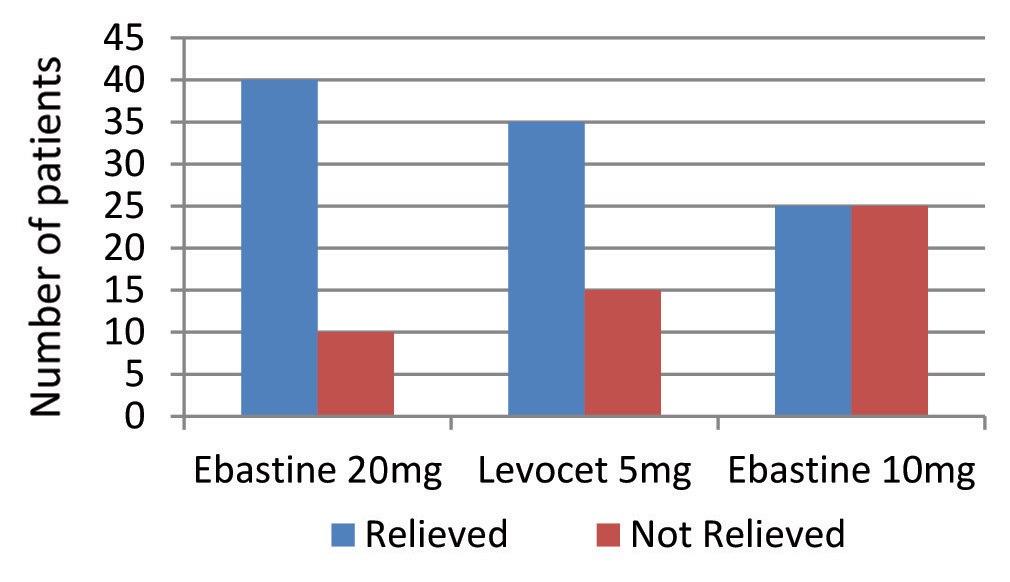
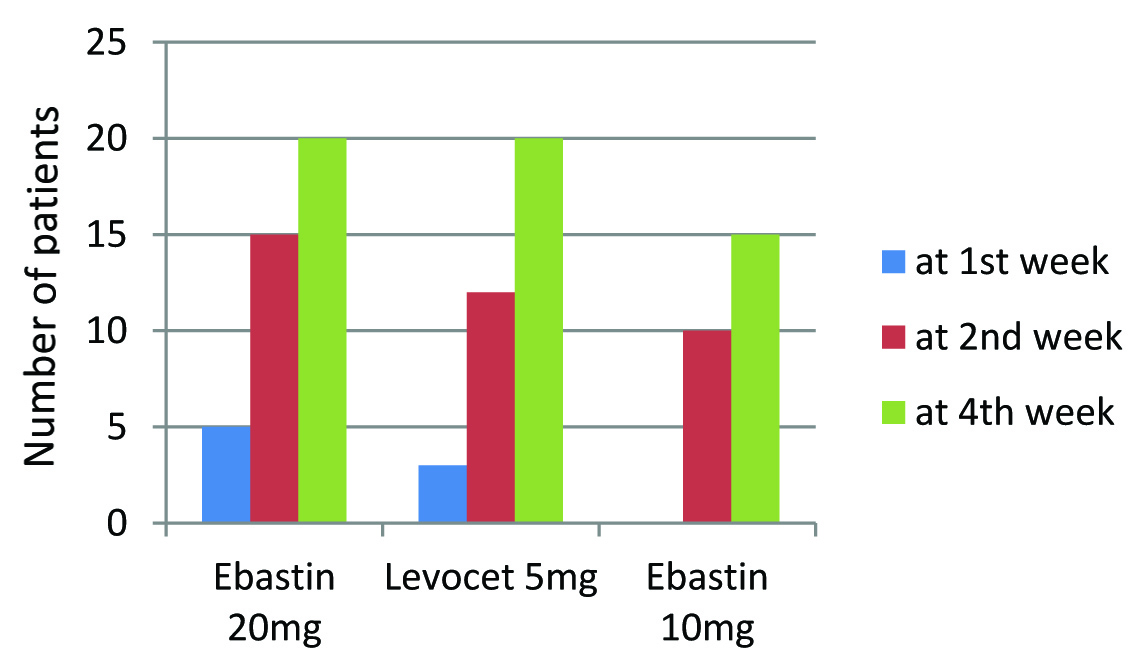
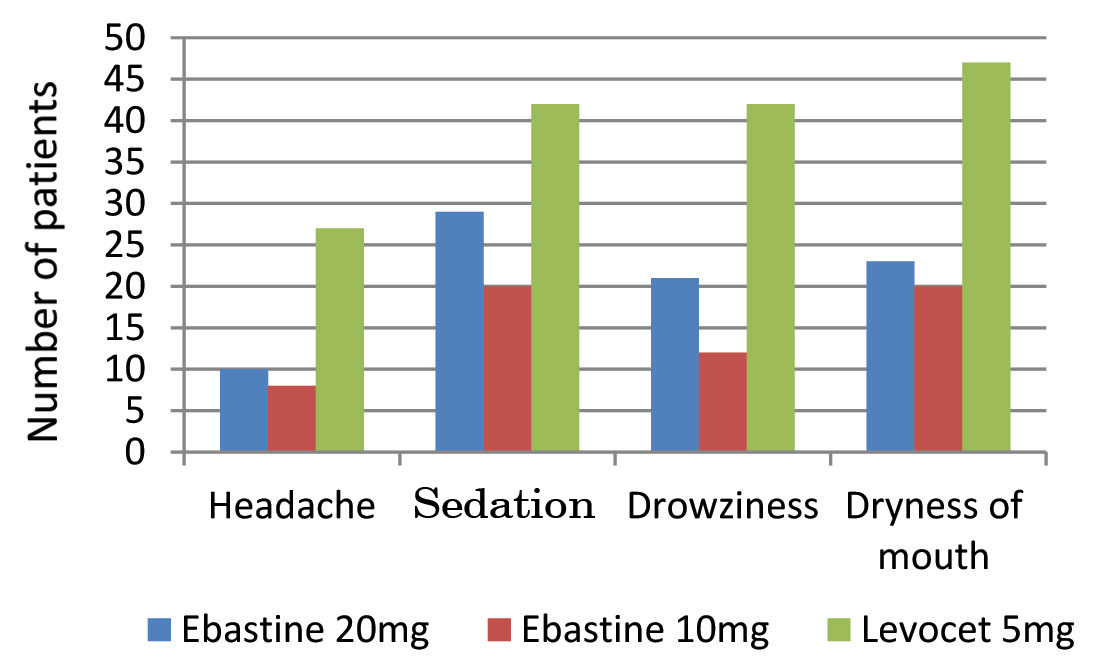
The mean age of patients was 32.82 years. The mean UAS 7 score at the end of 4th week was 1.08 with ebastine 20 mg, 1.98 with levocetirizine 5 mg and 3.98 with ebastine 10 mg. In group A, 40 out of 50 patients (i.e., 80%), in Group B 25 out of 50 (i.e., 50%) get UAS7=0 and in Group C, 35 (i.e., 70%) patients who got relieved of symptoms at the end of treatment. When the scores were redefined and categorized under relieved and not relieved, and comparison done between all three groups, then there was a significant difference in the number of patients getting relieved, with p<0.001 (highly significant). Levocetirizine 5 mg had shown more side effects like dryness of mouth and sedation as compare to ebastine irrespective of dosage. The comparison made between the number of patients developing side effects among the groups was highly significant (p<0.001) for all the side effects.
Conclusion
Ebastine 20 mg is found to have superior efficacy for treatment of Urticaria as compared to ebastine 10 mg but with levocetirizine 5 mg the results were almost similar. Tolerability of ebastine 20 mg is similar to ebastine 10 mg but with levocetirizine 5 mg there were more side effects and less tolerability.
Introduction
Urticaria also known as hives, wheals, welts or nettle rash – appears as raised, well circumscribed areas of erythema and edema involving the dermis and epidermis that are very pruritic. In acute urticaria – wheals are cleared completely within six weeks and in Chronic urticaria, the wheals persists for more than six weeks or often reappears over many years [1]. Wheals may appear on any part of the body, they may change shape, may change site of appearance, disappear and reappear over short periods of time or may spread across large areas. The rash is usually very itchy and ranges in size from a few millimeters to the size of a hand. Although the affected area may change in appearance within 24 hours, the rash usually settles within a few days Itching may be mild to severe. Scratching, alcoholic beverages [2], exercise and emotional stress may worsen the itching. Symptoms can last anywhere from minutes to months - or even years. Acute generalized urticaria is often idiopathic (in about 1/3rd of cases). Known causes include the following: <1% associated with food (particularly shellfish, fish, eggs, cheese, chocolate, nuts, berries, tomatoes [3], drugs, environmental factors (e.g., pollens, chemicals, plants, dander’s, dust, mold), exposure to latex, exposure to undue skin pressure, cold, or heat, emotional stress exercise, pregnancy {i.e., Pruritic Urticarial Papules and Plaques of Pregnancy (PUPPP)}, infections, malaria, ameobiasis, hepatitis, mononucleosis, cox-sackievirus, mycoplasma infections, infestations (e.g., scabies), HIV, parasitic infections, moths [4]. Chronic urticaria can be related to all of the above as well as to the following: Autoimmune disorders; probably up to 50% of chronic urticaria is autoimmune [5–8], Cholinergic urticaria induced by emotional stress, heat, or exercise [9]. Chronic medical illness, such as hypothyroidism, hyperthyroidism, amyloidosis and many others [10], cold urticaria, cryoglobulinemia, cryofibrinogenemia, or syphilis [11], mastocytosis [12] and inherited auto inflammatory syndromes [13]. The aetiology of chronic urticaria is undetermined in atleast 80-90% of patients [14]. In urticaria pigmentosa, Lesions are hyper pigmented (yellow, tan, or brown) and when lesions are stroked, a linear wheal is formed; this characteristic and diagnostic sign is known as the Darrier sign [15] but now urticaria pigmentosa is no longer considered a subtype of urticaria [16]. Recurrent urticaria can be related to the following: Solar urticaria occurs only on parts of skin exposed to the sun, exercise (cholinergic urticaria), emotional or physical stress, Water (aquagenic urticaria). For chronic or recurrent urticaria, basic laboratory studies should be prompted by signs and symptoms but may include a CBC count, erythrocyte sedimentation rate, thyroid-stimulating hormone value, and an antinuclear antibody level looking for possible causes of the urticaria [17]. Urticaria results from the release of histamine, bradykinin, leukotriene C4, prostaglandin D2, and other vasoactive substances from mast cells and basophils in the dermis [18]. The activation of the H1 histamine receptors on endothelial and smooth muscle cells leads to increased capillary permeability. The activation of the H2 histamine receptors leads to arteriolar and venular vasodilation [19,20]. Antihistamines block the action of the histamine. The main treatment of all forms of urticaria in adults and in children is with an oral second-generation antihistamine e.g., cetirizine, loratidine, fexofenadine, desloratadine, levocetirizine, ebastine, rupatadine and bilastine oral prednisone is used in severe urticaria or intramuscular injection of adrenaline is reserved for life-threatening anaphylaxis, supportive treatment with omalizumab or cyclosporine, other treatments that are sometimes used off-label in chronic urticaria include: Leukotriene, Anti-TNF alpha agents, e.g., infliximab, adalimumab, methotrexate, dapsone, phototherapy, intravenous immunoglobulins and if the cause of urticaria is known (drugs, pollens etc.,) then these should be eliminated [21]. The prognosis in acute urticaria is excellent as it is usually self limited but the prognosis in chronic urticaria is more guarded and depends on the co morbid disease causing the urticaria as well as the response to therapy [22]. Acute and chronic urticaria can result in severely impaired quality of life from pruritus and associated sleeplessness, as well as anxiety and depression. Additionally, many of the diseases associated with chronic urticaria may cause significant morbidity and mortality [22].
Ebastine is a piperidine derivative, is non sedating anti histamine and is long-acting, second generation, selective H1-receptor inverse agonist, extensively metabolized, probably in the liver, to carebastine which exert most (if not all) of the pharmacological actions associated with the administration of the parent drug. Peak plasma level of the metabolites occurs within two to four hours. Food increases the plasma level of carebastine 1.5-2.0 fold. Half-life is in between 15-19 hours. Ebastine and carebastine are highly protein bound (>95%). Headache, dry mouth and drowsiness, rarely abdominal pain, dyspepsia, asthenia, pharyngitis, epistaxis, sinusitis, nausea and insomnia may occur as adverse effects [21]. Caution should be exercised in patients with history of liver and kidney impairment, QT interval prolongation, during pregnancy and breastfeeding [23].
Levocetirizine (R-cetirizine) is a third generation non sedative antihistamine and is an inverse agonist developed from the second generation antihistamine cetirizine and has been shown to have both important affinity and selectivity for H1-receptors. It is rapidly and extensively absorbed. Tmax is 0.9 hour. Food delayed Tmax by approximately 1.25 hour and decreased Cmax by approximately 36%. The half life is about 8 to 9 hour. Elimination is 85.4% and 12.9% via urine and feces, respectively. Levocetirizine may cause side effects like: sleepiness, tiredness, weakness, sore throat, dry mouth, fever, cough and nosebleed [24].
The aim was to compare the safety and efficacy of ebastine 20 mg, ebastine 10 mg and levocetirizine 5 mg in the patients of acute urticaria.
Materials and Methods
A randomized longitudinal study was conducted in Dermatology Outpatient Department (OPD) of Adesh Institute of Medical Sciences and Research, Bathinda, India for a period of six months from January 2016 to July 2016. A total of 150 patients between the age group 10-70 years, both men and women having urticaria were enrolled and divided into three groups of 50 each. Group A was given ebastine 20 mg OD, Group B was given ebastine 10 mg OD and Group C was given levocetirizine 5 mg OD. Eligible patients were required to go for clinical examination and routine investigations including hemoglobin, total leucocyte count, absolute eosinophil count, urine analysis and stool examination. Informed consent was taken. These patients were then followed over the period of time at 1st week, 2nd week and 4th week. The patients were asked to scale there severity of disease over a period of follow up based on urticarial activity score 7 and patients over the period of follow up were also asked about the occurrence of side effects. UAS7 score-based health states were defined as follows: urticaria-free=0; well controlled urticaria=1–6; mild urticaria=7–15; moderate urticaria=16–27; and severe urticaria=28–42. The patients who had UAS score =0 that is patients had no itching and no wheals at the end of 4th week of treatment were considered to be relieved and then the total percentage of patients relieved in each group was calculated.
Statistical Analysis
Data was statistically compared by Chi-Square test SSPS data analysis software. The total no. of patients who develop side effects were also compared statistically by Chi-Square under each category for each side effect and p-value was calculated.
Results
A total of 150 patients were enrolled in study out of which 80(53.33%) were males and 70 (46.66%) were females as shown in [Table/Fig-1] and maximum patients i.e., 102 were in the age group of 20-40 years (68%) as shown in [Table/Fig-2]. The mean age of patients was 32.82 years as shown in [Table/Fig-3]. Out of 50 patients of Group A, 40 patients (i.e., 80%) were relieved (that is UAS=0) as shown in [Table/Fig-4]. Out of these, five patients (10%) get UAS=0 at 1st week of treatment and 15(30%) at 2nd week and 20 (40%) at 4th week of treatment as shown in [Table/Fig-5]. In Group B, 25 out of 50 (i.e., 50%) get UAS 7=0 at the end of treatment. Out of these 25 none of the patient got relieved of itching and wheals at 1st week as shown in [Table/Fig-5]. In Group C, there were 35 (i.e., 70%) patients who got relieved of symptoms as shown in [Table/Fig-4] and out of these three patients (6%) were relieved at 1st week and 12 patients (24%) at 2nd week and 20 (40%) were relieved of symptoms by 4th week as shown in [Table/Fig-5]. The mean UAS 7 score at the end of 4th week was 1.08 with ebastine 20 mg, 1.98 with levocetirizine 5 mg and 3.98 with ebastine 10 mg as shown in [Table/Fig-7]. When the scores were redefined and categorized under relieved and not relieved and compared, we found a significant difference in the number of patients getting relieved, as shown in [Table/Fig-8]. Out of 150 patients, 90 patients (60%) developed dryness of mouth (47 patients due to levocetirizine and less dryness with ebastine). There were 91 patients (60.6%) who developed sedation out of which 42 patients (28%) developed sedation with levocetirizine whereas 29 (i.e., 19.3%) with ebastine 20 mg and 20 patients (13.3%) developed sedation with ebastine 10 mg. With levocetirizine, 42 (i.e., 28%) developed drowsiness and with ebastine 20 mg, 21 patients (14%) and with ebastine 10 mg, 12 patients (8%) developed drowsiness as a side effect. With levocetirizine 5 mg, 27 patients (18%) and with ebastine 20 mg, 10 patients (6.6%) and with ebastine 10 mg, eight patients (5.3%) developed headache. [Table/Fig-6]. The comparison between side effects of ebastine 20 mg, 10 mg and levocetirizine 5 mg. was highly significant (p<0.001) for all the side effects, for all three forms of medications as shown in [Table/Fig-9].
Number of males and females in each group.
| Groups | Male | Female |
|---|
| Ebastine 20 mg- Group A | 30(20%) | 20(13.3%) |
| Ebastine 10 mg -Group B | 29(19.3%) | 21(14%) |
| Levocetirizine 5 mg -Group C | 21(14%) | 29(19.3%) |
| Total | 80(53.3%) | 70(46.6%) |
Age wise distribution of patients in each group.
| Age | Group A | Group B | Group C |
|---|
| 10-20 yrs | 12(8%) | 5(3.3%) | 3(2%) |
| 21-30 yrs | 13(8.6%) | 14(9.3%) | 13(8.6%) |
| 31-40 yrs | 17(11.3%) | 23(15.3%) | 22(14.6%) |
| 41-50 yrs | 6(4%) | 8(5.3%) | 10(6.6%) |
| 51-60 yrs | 1(0.66%) | - | 1(0.66%) |
| >=61 yrs | 1(0.66%) | - | 1(0.66%) |
| Groups | Mean age |
|---|
| Ebastine 20 mg | 30.24 |
| Ebastine 10 mg | 33.02 |
| Levocetirizine 5 mg | 35.2 |
| Overall mean age | 32.82 |
Number of patients relieved with each medication.
UAS 7 = 0 of patients on follow up.
Side effects of medication given.
Mean UAS 7 score at follow up
| 1st week | 2nd week | 4th week |
|---|
| Ebastine 20mg | 19.5 | 7.1 | 1.08 |
| Ebastine 10mg | 24.8 | 12.82 | 3.98 |
| Levocet 5mg | 25.38 | 10.32 | 1.98 |
Statically analyses of patients relieved in each group.
| Relived | Not Relieved | p-value |
|---|
| Ebastine 20mg | 40(26.6%) | 10(6.6%) | P< 0.01(p= 0.005248) |
| Ebastine 10mg | 25(16.6%) | 25(16.6%) |
| Levocetrizine 5mg | 35(23.3%) | 15(10%) |
Comparison between no. of patients developing side effects in each group.
| Side effect | | Levocetirizine 5 mg | Ebastine20 mg | Ebastine10 mg | p-value |
|---|
| Dryness | Yes | 47(31.3%) | 23(15.3%) | 20(13.3%) | p<0.001 |
| No | 3(2%) | 27(18%) | 30(20%) |
| Sedation | Yes | 42(28%) | 29(19.3%) | 20(13.3%) | p<0.001 |
| No | 8(5.3%) | 21(14%) | 30(20%) |
| Drowsiness | Yes | 42(35%) | 21(14%) | 12(8%) | p<0.001 |
| No | 8(5.3%) | 29(19.3%) | 38(25.3%) |
| Headache | Yes | 27(18%) | 10(6.6%) | 8(5.3%) | p<0.001 |
| No | 23(15.3%) | 40(26.6%) | 42(28%) |
The difference in the number of patients experiencing side effects is varying for Ebastine 20mg, 10mg and Levocetirizine 5mg. This difference is highly significant (p<0.001) for all the side effects, for all three forms of medication.
Discussion
Urticaria has a profound impact on the quality of life and causes immense distress to patients, necessitating effective treatment. Various treatment modalities are available out of which second generation non-sedating H1 antihistamines e.g., fexofenadine, loratidine, desloratadine, cetirizine, levocetirizine, ebastine, mizolastine, olapatadine, rupatadine etc., are used as the first-line treatment [25]. Approximately 15 to 20% of the general population will have urticaria at least once during their lifetime. Urticaria mostly occurs after adolescence with highest incidence in young adults but can occur at any age. Approximately 3% of population is affected by urticaria [26]. In our study, we found that ebastine 20 mg was more efficacious for treating urticaria associated wheals and pruritus and also with ebastine 20 mg there were five patients who get relieved at 1st week of treatment as compared to levocetirizine 5 mg, three patients were relieved at 1st week and with ebastine 10 mg none of the patients get relieved at 1st week of treatment. This was comparable to the studies which showed superior efficacy of 20 mg of ebastine as compared with 10 mg of ebastine and 10 mg of cetirizine on the skin wheal response 24 hour after the last dose of a 6-day-long treatment [27–30].
In our study we found that the efficacy of ebastine 20 mg and levocetirizine 5 mg have only some difference in relieving itching and wheals. We found that side effects were more with levocetirizine as compared to that of ebastine. These can be comparable with the study also showed that with levocetirizine, patients experienced headache (23.8%), pharyngitis (19.4%), influenza (14.6%), fatigue (8.3%), and somnolence (8.3%) when used to treat Urticaria [31].
Limitation
Limitations of the study were that we were not able to do crossover study in our patients, evaluate the blood drug levels & evaluate all side effects of drugs.
Conclusion
The study concluded that ebastine 20 mg is found to have superior efficacy and similar tolerability for treatment of Urticaria as compared to ebastine 10 mg but with levocetirizine 5 mg, there was similar efficacy and had more side effects with lesser tolerability. There is the still need for additional studies designed to investigate the response of higher doses of Non Sedative Antihistamines in patients who doesn’t respond to the recommended doses according to current guidelines.
The difference in the number of patients experiencing side effects is varying for Ebastine 20mg, 10mg and Levocetirizine 5mg. This difference is highly significant (p<0.001) for all the side effects, for all three forms of medication.
[1]. Frigas E, Park MA, Acute urticaria and angioedema: Diagnostic and treatment considerationsAm J Clin Dermatol 2009 10(4):239-50. [Google Scholar]
[2]. Ribeiro F, Sousa N, Carrapatoso I, SegorbeLuÍs A, Urticaria after ingestion of alcoholic beveragesJ Investig Allergol ClinImmunol 2014 24(2):122-23. [Google Scholar]
[3]. Darlenski R, Kazandjieva J, Zuberbier T, Tsankov N, Chronic urticaria as a systemic diseaseClin Dermatol 2014 32(3):420-23. [Google Scholar]
[4]. Powell RJ, Leech SC, Till S, Huber PA, Nasser SM, Clark AT, BSACI guideline for the management of chronic urticaria and angioedemaClin Exp Allergy 2015 45(3):547-65. [Google Scholar]
[5]. Kasperska-Zajac A, Jasinska T, Grzanka A, Kowalik-Sztylc A, Markers of systemic inflammation in delayed pressure urticariaInt J Dermatol 2013 52(3):309-10. [Google Scholar]
[6]. Konstantinou GN, Asero R, Maurer M, Sabroe RA, Schmid-Grendelmeier P, Grattan CE, EAACI/GA (2) LEN task force consensus report: The autologous serum skin test in urticariaAllergy 2009 64(9):1256-68. [Google Scholar]
[7]. Hossler EW, Caterpillars and moths: Part I. Dermatologic manifestations of encounters with LepidopteraJ Am Acad Dermatol 2010 62(1):1-10. [Google Scholar]
[8]. Kaplan AP, Greaves M, Pathogenesis of chronic urticariaClin Exp Allergy 2009 39(6):777-87. [Google Scholar]
[9]. Viola M, Quaratino D, Gaeta F, Rumi G, Caruso C, Romano A, Cross reactive reactions to non steroidal anti inflammatory drugsCurr Pharm Des 2008 14(27):2826-32. [Google Scholar]
[10]. Vonakis BM, Saini SS, New concepts in chronic urticariaCurr OpinImmunol 2008 20(6):709-16. [Google Scholar]
[11]. Guldbakke KK, Khachemoune A, Aetiology, classification, and treatment of urticariaCutis 2007 79(1):41-49. [Google Scholar]
[12]. Bains SN, Hsieh FH, Current approaches to the diagnosis and treatment of systemic mastocytosisAnn Allergy Asthma Immunol 2010 104(1):1-10.quiz 10-2, 41 [Google Scholar]
[13]. Goldfinger S, The inherited autoinflammatory syndrome: A decade of discoveryTrans Am Clin Climatol Assoc 2009 120:413-18. [Google Scholar]
[14]. Nichols KM, Cook-Bolden FE, Allergic skin disease: Major highlights and recent advancesMed Clin North Am 2009 93(6):1211-24. [Google Scholar]
[15]. Brodell LA, Beck LA, Differential diagnosis of chronic urticariaAnn Allergy Asthma Immunol 2008 100(3):181-88.quiz 188-90, 215 [Google Scholar]
[16]. Sánchez-Borges M, Asero R, Ansotegui IJ, Baiardini I, Bernstein JA, Canonica GW, Diagnosis and treatment of urticaria and angioedema: A worldwide perspectiveWorld Allergy Organ J 2012 5(11):125-47. [Google Scholar]
[17]. Irinyi B, Szeles G, Gyimesi E, Tumpek J, Heredi E, Dimitrios G, Clinical and laboratory examinations in the subgroups of chronic urticariaInt Arch Allergy Immunol 2007 144(3):217-25. [Google Scholar]
[18]. Acton QA, Vasculitis: New Insights for the Healthcare Professional: 2013 Edition-Scholarly Brief™, 22-Jul-2013, Chapter 4Immunology:24 [Google Scholar]
[19]. Zuberbier T, Maurer M, Urticaria: Current opinions about aetiology, diagnosis and therapyActa Derm Venereol 2007 87(3):196-205. [Google Scholar]
[20]. Kaplan AP, Joseph K, Maykut RJ, Geba GP, Zeldin RK, Treatment of chronic autoimmune urticaria with omalizumabJ Allergy ClinImmunol 2008 122(3):569-73. [Google Scholar]
[21]. Grattan CEH, Humphreys F. Guidelines for evaluation and management of urticaria in adults and children, British Association of Dermatologists Therapy Guidelines and Audit Subcommittee, July 2007, library-media/documents/Urticaria_2007.pdf [Google Scholar]
[22]. Grob JJ, Gaudy-Marqueste C, Urticaria and quality of lifeClin Rev Allergy Immunol 2006 30(1):47-51. [Google Scholar]
[23]. Vincent J, Liminana R, Meredith PA, Reid JL, The pharmacokinetics, antihistamine and concentration-effect relationship of Ebastine in healthy subjectsBritish Journal of Clinical Pharmacology 1988 26(5):497-502. [Google Scholar]
[24]. Gandon JM, Allain H, Lack of effect of single and repeated doses of levocetirizine, new antihistaminic drug, on cognitive and psychomotor functions in healthy volunteersBr J Clin Pharmacol 2002 54(1):51-58. [Google Scholar]
[25]. Godse KV, Zawar V, Consensus statement on the management of urticariaIndian J Dermatol 2011 56(5):485-89. [Google Scholar]
[26]. Greaves MW, Chronic urticariaN Engl J Med 1995 332:1762-72. [Google Scholar]
[27]. Frossard N, Benabdesselam O, Purohit A, Mounedji N, Pauli G, Activity of ebastine (10 and 20 mg) and cetirizine at 24 hours of a steady state treatment in the skin of healthy volunteersFundam Clin Pharmacol 2000 14(4):409-13. [Google Scholar]
[28]. Godse KV, Ebastine in chronic spontaneous urticaria in higher doseIndian J Dermatol 2011 56(5):597-98. [Google Scholar]
[29]. Hurst M, Spencer CM, Ebastine: An update of its use in allergic disordersDrugs 2000 59(4):981-1006. [Google Scholar]
[30]. Magerl M, Schmolke J, Metz M, Zuberbier T, Siebenhaar F, Maurer M, Prevention of signs and symptoms of dermographic urticaria by single-dose Ebastine 20 mgClin Exp Dermatol 2009 34(5):e137-40. [Google Scholar]
[31]. Singh-Franco D, Ghin HL, Robles GI, Borja-Hart N, Perez A, Levocetirizine for the treatment of allergic rhinitis and chronic idiopathic urticaria in adults and childrenClin Ther 2009 31(8):1664-87. [Google Scholar]