Carcinoma of the breast is the most common non-skin malignancy in women and is second to the lung cancer as a cause of cancer death [1]. TCB is an integral part of triple assessment of breast cancer which includes clinical assessment, mammography and TCB or CNB [2].
TCB is considered superior to Fine Needle Aspiration Cytology (FNAC) of breast lesions as it provides sufficient tissue for pathologists to make an accurate diagnosis which can guide both surgeons and oncologists in designing appropriate therapeutic strategy for management of patients with breast masses [3].
Histopathological evaluation of TCB can help to differentiate benign and malignant lesions, to categorize each group into different subtypes. We analysed 892 numbers of TCBs in our centre and there were no false positive biopsy identified in this series giving a specificity of 100% which include diagnosis of carcinoma, phyllodes tumour, lymphoma and sarcoma. The benign lesions were categorized into neoplastic (fibroadenoma, phyllodes tumour) and non-neoplastic, i.e., granuloma, inflammatory, normal etc.
Materials and Methods
This retrospective study of breast lesions was performed from January 2013 to June 2016 for a period of three years and six months. All the patients attending the outpatient department of AH Regional Cancer Center, Cuttack, Odisha, India, with complaints of breast symptoms were examined by the surgical oncologists of our institute. Wherever, a biopsy was indicated following clinical and radiological examinations, TCB was performed under local anaesthesia by the concerned surgeons. The needle used was TRU-CUTTM 2N2704X, 149X15CM (carefusion Waukwgan, IL).
Usually two to three passes were made in each patient. Seeing the adequacy of material, the specimens were fixed in 10% formalin and embedded in paraffin wax and stained with Haematoxylin and Eosin stain. The histology was compared where subsequent excision biopsy were available like wide local excision and mastectomy.
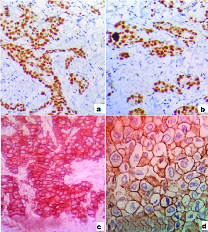
The paraffin blocks were used for IHC where the oncologists planned for Neo-Adjuvant Chemotherapy (NACT). IHC was done on 4 μm thickness sections from paraffin blocks of TCB/CNB for ER, PR and Her 2/neu. Routine IHC staining procedures like baking were followed, such as, antigen retrieval, endogenous enzyme block, staining with primary antibody, incubated Horse Radish Peroxidase (HRP) polymers conjugated with secondary antibodies (Biogenex). Finally sections were washed and chromogen was added. Then sections were counterstained by haematoxylin, dehydrated and mounted for analysis. For each row of staining, a positive and negative control slide was also prepared. Semi-quantitative Allred scoring system [4] were used to interpret ER, PR staining which takes into consideration of both the proportion (PS) and intensity (IS) of nuclear staining [Table/Fig-1a,b]. The scoring for PS ranged from 0 to 3 and for intensity it ranged from 0 to 5. Tumour cells with a Total Score (TS) of 3 to 8 were considered positive and TS less than 3 were considered negative. Her-2/neu staining was scored from 0 to 3. Intense complete circumferential staining in more than 10% cells was considered positive and given a score of 3 [Table/Fig-1c,d].
a) Nuclear staining of ER in cancer cells (IHC, 10X); b) Nuclear staining of PR in cancer cells (IHC, 10X); c & d) Intense, complete circumferential membrane staining of Her-2/neu in almost all the cancer cells (IHC, 10X, 40X).
Biopsy was repeated in 23 cases where there was clinical suspicion of malignancy, FNAC was positive but initial TCB was negative, where mammography showed BIRADS III or IV lesions, where there was predominant necrotic pattern and in cases where the patients were unfit for surgery to do the receptor assay for treatment planning. Sensitivity (SN) and Specificity (SP) were analysed.
Results
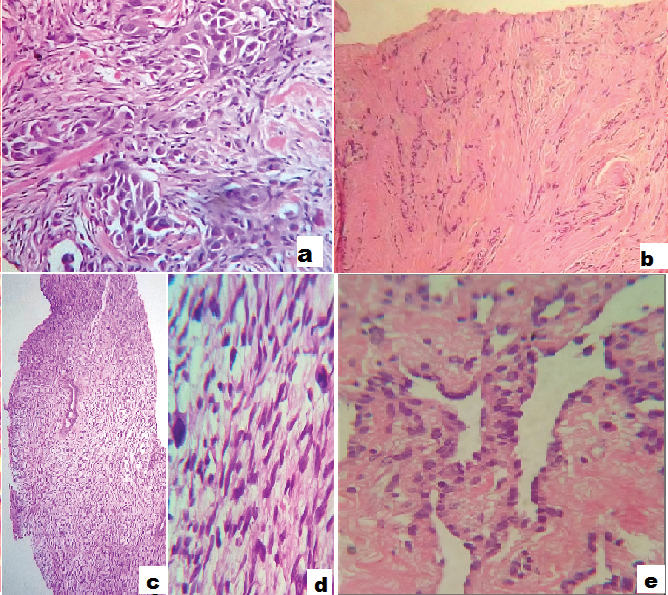
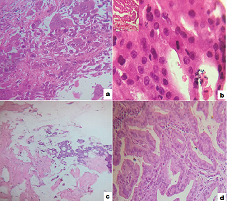
A total number of 892 TCBs were performed in AH Regional Cancer Centre, Cuttack, Odisha, India, from January 2013 to June 2016. The age range was from 16 to 88 years. A total of 13 (1.4%) TCBs were performed in male patients, among which, two were reported as invasive duct carcinoma, eight as gynaecomastia, one as fibroadenoma, one each as inflammation/mastitis and Fibrofatty Collagenous Stroma (FFCS). One of the carcinomas in male was Invasive Duct Carcinomas Not Other Specified (IDC-NOS) type and other one was mucinous type. All cases of gynaecomastia, fibroadenoma were confirmed on excisional specimens and two of the carcinoma cases were also confirmed in mastectomy specimens. Overall there were 747 (83.7%) cases diagnosed as malignant neoplasm out of which 735 (98.39%) were carcinomas (with 21 cases diagnosed on repeat TCBs). Among all carcinoma cases 702 (95.51%) were reported as IDC-NOS type, 24 (3.26%) were Invasive Lobular Carcinomas ILC, 2 (0.27%) metaplastic carcinoma, 1(0.13%) apocrine carcinoma, 5 (0.68%) mucinous carcinomas and 1(0.13%) papillary carcinoma which were confirmed on mastectomy specimens [Table/Fig-2a-e,3a-d].
a) Invasive duct carcinoma (IDC, GR III) (x100, H&E stain); b) Invasive lobular carcinoma (x40, H&E stain); c) Malignant Phyllodes tumour (x40, H&E stain); d) Malignant Phyllodes tumour (x400, H&E stain); e) Angiosarcoma (x400, H&E stain).
a) Metaplastic carcinoma showing pleomorphic neoplastic cells and multinucleated giant cells (x100, H&E stain); b) Apocrine carcinoma (x400, H&E stain); c) mucinous carcinoma showing pools of mucin and clusters of neoplastic cells (x40, H&E stain); d) Papillary carcinoma (x100, H&E stain).
Other malignant neoplasms were 9 (1.20%) malignant phyllodes tumour, 2 (0.26%) cases of angiosarcoma and 1 (0.13%) case of NHL [Table/Fig-2a-e].
Nonmalignant cases were 145 (16.25%) out of which 8 (0.89%) cases were gynaecomastia, 2 (0.22%) were granulommatous lesion, 4 (0.44%) were inflammatory lesion, 1 (0.11%) case of lactational change, 73 (8.18%) cases reported as fibrofatty collagenous stroma with few benign acini, 5 (0.55%) cases as atypical hyperplasia, 7 (0.77%) cases as suspicious and 3 (0.33%) cases as inadequate/ scanty tissue. So TCBs were repeated in 23 (2.57%) cases which included all the suspicious, inadequate/scanty tissue, atypical hyperplasia and eight cases reported as FFCS where there was strong suspicion of malignancy on clinical and mammographic assessment. Out of these 23 cases, 21 cases came out to be positive for duct carcinoma and two cases still showed the same fibrofatty collagenous stroma, which on lumpectomy were diagnosed as benign breast disease. So, 21 cases were false negative. There were no false positive biopsies in this series giving a specificity of 100% and sensitivity of 97%.
Out of 735 cases reported as carcinomas, 315 (42.85%) cases occurred in right breast, 412 (56.05%) cases in left breast, and 8 (1.08%) cases were bilateral breast carcinoma, hence, actual number of patients diagnosed with carcinoma on TCB was 727. Of these 727 cases, 219 (30.12%) cases were in young, i.e., below 40 years of age {164 (22.55%) cases between 31-40 years, 51 (7.01%) cases between 21-30 years and 4 (0.55%) cases below 21 years} [Table/Fig-4]. In 9 (9/727) cases, TCBs were done in patients with recurrent chest wall nodules who had undergone mastectomy surgery outside the institution and reports were not available. It was not possible to get the paraffin blocks for receptor assay. Out of the 735 carcinoma, TCB paraffin blocks were used for IHC evaluation in 260 (30%) carcinoma cases and one NHL. The ER, PR and Her-2/neu expression status of the tumour is summarized in [Table/Fig-5]. In these cases either NACT was planned due to high stage of the patients, showing bone, liver and lungs metastasis or there were contraindications for surgery of the patients due to other medical diseases, or recurrent chest wall nodules (nine cases) where receptor assay was not done in initial mastectomy specimens and it was not possible to get the paraffin blocks.
Age and sex incidence of malignant tumors.
| Age group | M | F | IDC | ILC | OtherCarcinoma | MalignantPhyllodes | Others | Total |
|---|
| <20 | | 4 | 3 | 1 | | | | 4 |
| 21-30 | | 51 | 49 | 2 | | | | 51 |
| 31-40 | | 164 | 161 | 2 | | 1 | | 164 |
| 41-50 | 2 | 247 | 235 | 10 | 3 | 1 | | 249 |
| 51-60 | | 184 | 171 | 5 | 2 | 4 | 2 | 184 |
| 61-70 | | 76 | 66 | 3 | 3 | 3 | 1 | 76 |
| >71 | | 19 | 17 | 1 | 1 | | | 19 |
| Total | 2 | 745 | 702 | 24 | 9 | 9 | 3 | 747 |
M-male, F-female, IDC-invasive duct carcinoma, ILC-invasive lobular carcinoma
Immunohistochemical staining results in 261 cases.
| Histological markers | Number of cases | Percentage |
|---|
| ER +, PR +, Her-2/neu - | 130 | 49.8 |
| ER -, PR -, Her-2 + | 48 | 18.3 |
| ER +, PR +, Her-2 + | 05 | 1.91 |
| ER -, PR -, Her-2 - | 67 | 25.6 |
| ER +, PR +, Her-2 Equivocal | 02 | 0.76 |
| ER -, PR -, Her-2 Equivocal | 08 | 3.06 |
| CD45 +, CD20 + (NHL) | 01 | 0.38 |
Discussion
Breast cancer is the second most common cancer in the world and the first of the female reproductive system. TCB is performed in an outpatient setting and can replace incisional biopsy done in operating room, being more practical and less costly [5].
Another advantage of TCBs is that a definitive diagnosis of invasive carcinoma can be given and the difficulty of differentiating atypical hyperplasia and carcinomas or low grade well differentiated carcinoma seen in FNAC can be overcome [6].
In our study the sensitivity was 97% in diagnosing malignant lesions which was found to be 95.1% by Rikabi A and 88.7% by Woodcock NP et al., [3,6]. The specificity in our study was 100% which was close to and similar to the observations by other authors [3,6] [Table/Fig-6] [3,6–13].
Comparison with studies by other authors.
| Authors | Year | No. of cases/ Core needle biopsies | Period of study | Sensitivity | Specificity | PPV | NPV | Diagnostic Accuracy |
|---|
| Minkowitz S et al., [7] | 1986 | 158 | Jan 1980 – Nov 1984 | 94 | 100 | - | - | - |
| Woodcock NP et al., [6] | 1998 | 187 | Apr 1994– Jun 1996 | 88.7 | 100 | - | - | - |
| Gukas ID et al., [8] | 2000 | 112 | - | 88.9 | 96.8 | - | - | 93.5 |
| Homesh NA et al., [9] | 2005 | 296 | May 1998- May 2002 | 92.3 | 94.8 | 100 | 100 | 93.4 |
| AA Barra et al., [10] | 2007 | 264 | Aug 1997 – Aug 2002 | 88.3 | 95.2 | 100 | 74.1 | - |
| Kulkarni D et al., [11] | 2009 | 819 | 5 years | 97.7 | 94.2 | 93.1 | 98.1 | 95.5 |
| Lacambra MD et al., [12] | 2012 | 285 | - | 96 | 99 | 99 | 94 | - |
| Rikabi A and Husain S [3] | 2013 | 275 | Jan 2008 – Dec 2010 | 95.1 | 100 | 100 | 97.2 | 98.2 |
| Moschetta M et al., [13] | 2014 | 190 | Sep 2011 – May 2013 | 97 | 96 | 97 | 96 | 96 |
| Present study | 2016 | 892 | Jan 2013 – Jun 2016 | 97.27 | 100 | 100 | 85.52 | 97.64 |
The age range in our series was from 16 to 88 years. We observed four cases in very young patients, i.e., below 20 years. The peak age incidence was between 41 to 50 years, which was identical to other studies [3,7].
Benign changes or normal breast tissue (fibrofatty collagenous stroma) need to be interpreted in the context of clinical findings [7].
As per our observation we were able to diagnose benign lesions like fibroadenomas, gynaecomastia, benign phyllodes tumour, lactational change and papilloma on TCBs which were subsequently confirmed by excisional biopsy specimens. It was also possible to accurately diagnose malignant lesions such as NHL, angiosarcoma and malignant phyllodes tumour where the biopsy materials were adequate and from representative site. The single case of NHL in our series was a case of B cell lymphoma and IHC was done on the TCB paraffin block. TCB was also helpful in giving the accuracy regarding different histological types of carcinoma. We have reported 24 cases of lobular carcinomas in this series, the diagnosis of which may be missed by FNAC as also observed by Minkowitz S et al., [7].
Mucinous, apocrine, metaplastic and papillary carcinomas were reported accurately on TCB sections. Thus, precise pathological diagnosis often facilitates patient management [6].
The size of biopsy needle used in this study was 14G for all the cases. Narrower bore 18G needles were used by Woodcock NP et al., for small lesions to minimize massive displacement during biopsy [6]. Other studies have advocated the use of the larger 14G for all cases stating that it consistently produces higher quality, more intact cores, improving diagnostic accuracy, without an increase in morbidity [14]. However, others claim that the larger needles do cause significantly more bleeding [15]. There were no significant complications after CNB procedure in the patients in our study.
Positive nuclear staining for ER, PR with Allred scores showed 130 (49.8%) cases to be ER, PR positive which is the most common form of invasive breast carcinoma in our series [4]. This is comparable to other studies which is 50% to 65% worldwide. In a study conducted by Mostafa M et al., ER positive cases were 69%, Her-2/neu positive cases were 28% and triple negative cases were 0.9% [16]. The ER, PR negative and Her-2/neu positive in our series was 18.3% and triple negative cases were 25%. This is possibly due to large number of cases (1042) analysed in the series done by Mostafa M et al., [16]. Besides, the present series has taken into consideration of IHC results done on TCBs only, excluding the post surgical specimens.
The result of this study suggests that TCB is an accurate, safe and reliable method in establishing the diagnosis of palpable breast lesions.
Limitation
It needs experienced surgeons so that the biopsy will be from proper site. Besides in tumours having large areas of haemorrhage and necrosis, a TCB may not be helpful. In small tumours or tumours associated with fibrosis, tissue obtained by TCB may not be representative or may require a repeat TCB.
The most important advantage of TCB is that IHC can successfully be done on TCB paraffin blocks. Where there was a strong suspicion of malignancy, clinically and radiologically, and where in tissue sections the material was haemorrhagic or predominantly necrotic, a repeat TCB often increases the sensitivity. Some authors have reported the sensitivity to increase with repeat biopsy from 88 to 97.7% [7] which was also observed in our series.
Conclusion
We agree with other studies that TCB is an essential part of management of palpable breast lesions which can guide the surgeons and oncologists. This is useful for both histological diagnosis and IHC evaluation where necessary. Different histological types of carcinomas, lymphoma, malignant phyllodes tumour and sarcomas can also be diagnosed from TCBs.
M-male, F-female, IDC-invasive duct carcinoma, ILC-invasive lobular carcinoma