TKA is the surgical replacement of arthritic knee joint There has been a progressive modification in the design of the TKA implant over last few decades. Still, the Patello-Femoral (PF) complications continue to be the most common complications in TKA [1].
The PFJ includes both anterior condyle of distal femur and patella. Resurfacing of PFJ involves both anterior femur and patellar cut. The anterior femur and the patellar cut are usually unmeasured and the implant used does not match the amount of bone resected. This discrepancy in the amount of bone resected and the size of the prosthesis inserted leads to overstuffing of the PFJ and limited knee ROM [2,3].
So, we put forth the dimension- “PATELLO - FEMORAL COMPOSITE” to study the overstuffing of PFJ. This is the distance between anterior cortical line of femur shaft and anterior cortex of patella with the knee in full extension. We hypothesize that accurate reproduction of PFC in the postoperative TKA patients is of paramount importance to avoid PFJ overstuffing. Through our study, we wish to calculate chances of overstuffing of PFJ in postoperative TKA patients and to document the effect of overstuffing of PFJ on passive knee ROM in postoperative TKA patients.
Materials and Methods
Our study was a prospective comparative study with Level II evidence. Institutional ethics committee approval was obtained before beginning the study. The study was planned in a prospective observational manner between May–September 2013. It included 51 consecutive primary TKAs performed during the study period. They were performed by the same surgeon, using the same technique at our tertiary care center.
All the patients included in the study showed clinical and radiological evidence of advanced knee osteoarthritis and required primary TKA. Patients showing clinical or radiological evidence of osteoarthritis but not requiring TKA were excluded from the study. Also, patients showing preoperative evidence of patellar maltracking, or patella alta or baja were excluded. The patients included were explained regarding the purpose of the study and a written informed consent in their vernacular language was obtained from these patients. Patients not willing to give consent were excluded from the study. Patients included in the study underwent primary TKA using either All Polythene or Metal backed primary TKA implant.
The patient’s demographic information including name, age, sex and duration of symptoms, height in centimeters (cm) and weight in kilograms (Kg) were recorded. The preoperativeerative and postoperative (24 weeks) passive knee ROM of patients was measured using standard goniometer with the patient in supine position. The same technique for measuring preoperative and postoperative knee ROM was followed throughout the study period.
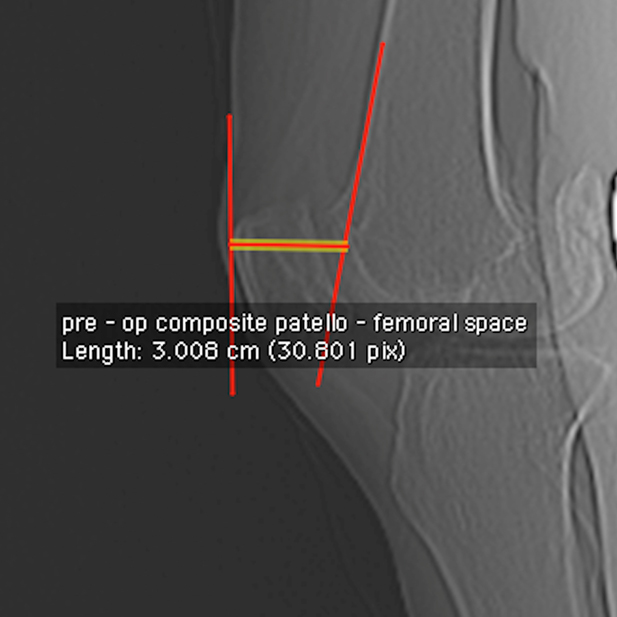
The preoperative and postoperative radiological parameters [Table/Fig-1] relevant to the study were recorded using the CT Scanogram image of patient’s knee in lateral view with full extension and perfect overlap of both the femur condyles. Parameters were measured using DICOM format of the CT Scanogram image on DICOM viewer. Preoperative PFC [Table/Fig-2] was the maximum distance from anterior border of patella to anterior femoral cortical line with knee in full extension and both femur condyles overlapping. It included the thickness of the patella and the maximum thickness of the femur beyond the anterior femur cortical line and the patella-femoral space.
Preoperative radiological parameters, pictorial representation of the radiological parameters included in study PFC, PT and AFO.
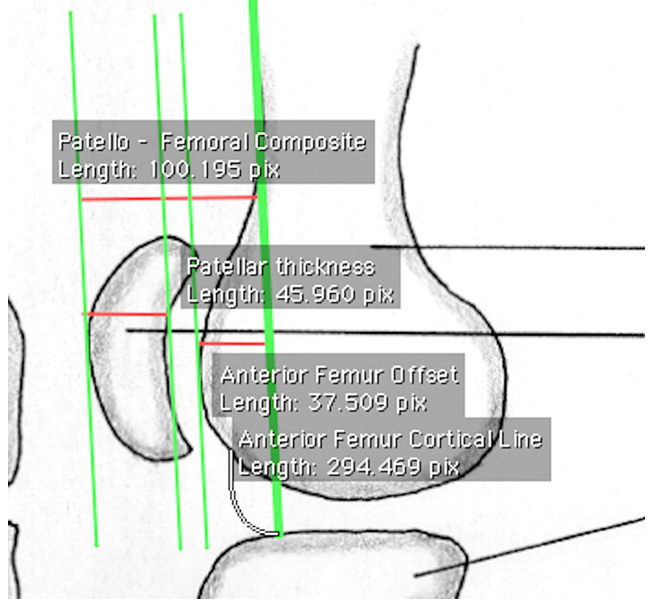
Preoperative PFC, Distance between anterior cortex of patella and anterior femur cortical line.
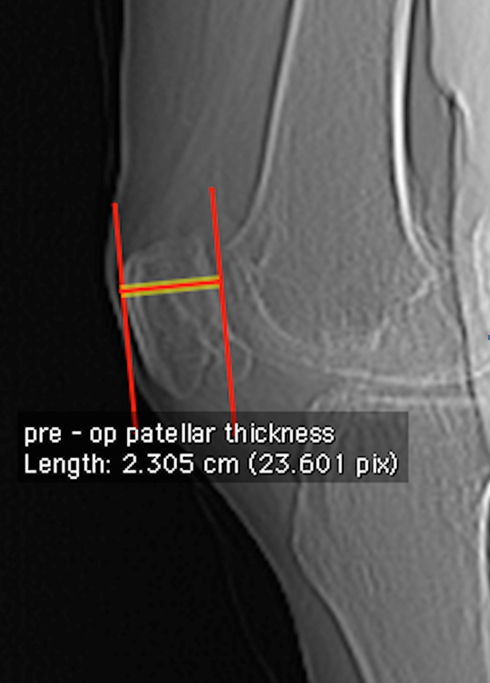
Preoperative PT [Table/Fig-3] was defined as the thickness from the anterior to posterior cortex of patella with the knee in full extension and both femur condyles overlapping.
Preoperative PT, Distance between anterior and posterior cortex of patella.
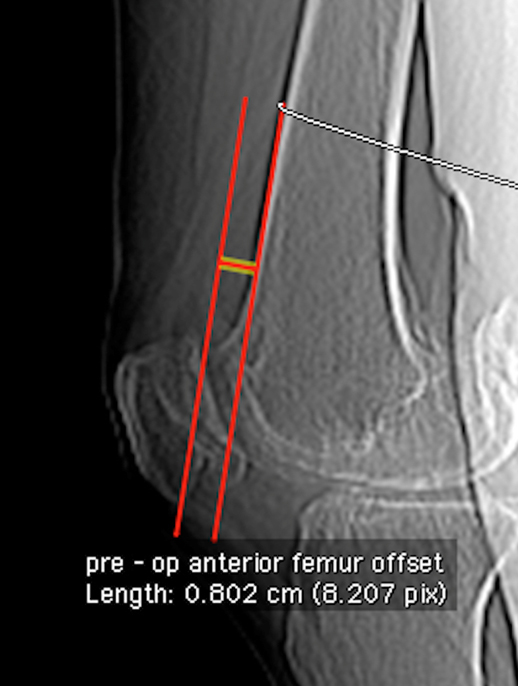
Preoperative AFO [Table/Fig-4] was defined as the maximum anterior thickness of the distal femur beyond the anterior femur cortical line.
Preoperative AFO, Maximum anterior thickness of distal femur beyond the anterior femur cortical line.
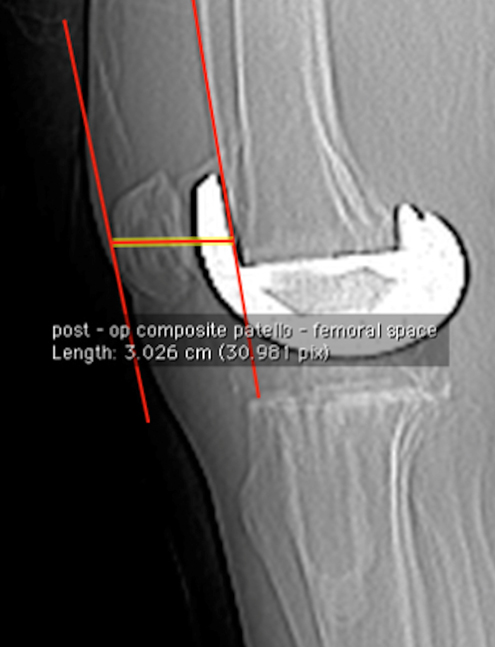
Postoperative PFC [Table/Fig-5] was the maximum distance from the anterior border of patella to anterior femoral cortical line with knee in full extension and both femur condyles overlapping. It includes thickness of the patella (thickness of remaining native patella + patellar button thickness) + thickness of the anterior flange of the femoral component of TKA implant.
Postoperative PFC, Distance between anterior cortex of patella and anterior femur cortical line.
Postoperative PT [Table/Fig-6] was defined as the sum of the thickness of remaining native patella and patellar button.
Postoperative PT, Maximum thickness of remaining native patella and thickness of patellar button.

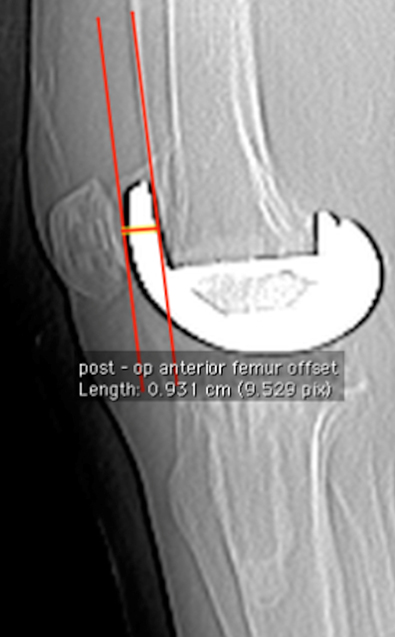
Postoperative AFO [Table/Fig-7] was defined as the maximum anterior thickness of the distal femur beyond the anterior femur cortical line i.e. the thickness of the anterior flange of the femoral component.
Postoperative AFO, Thickness of the anterior flange of the femur component of the TKA implant.
Statistical Analysis
The patients were grouped into those with or without PFJ overstuffing depending on whether the postoperative PFC was more or less than the preoperative PFC and analysed using the IBM SPSS STATISTICS software version 22.0 64 - bit edition. We used the unpaired Student’s t-test to compare the means of the parameters of the preoperative and the postoperative groups of patients with or without PFJ overstuffing. The results derived are discussed further in the following section.
Results
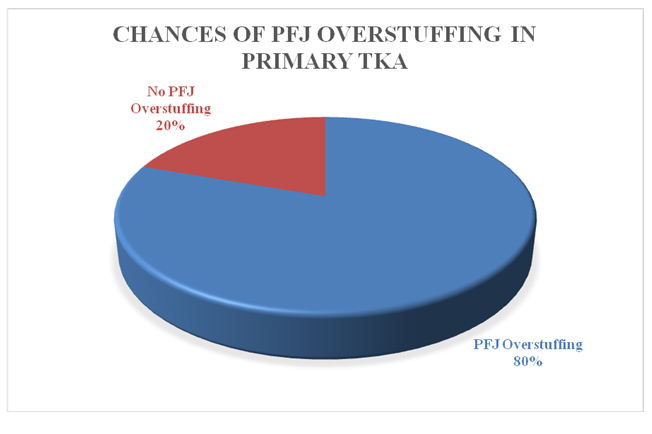
During the study period 51 TKAs were performed on 44 patients - 12 males and 32 females. Age group of the patients included in the study ranged from 45 years to 75 years with Mean (M)±Standard Deviation (SD) of 62.02±7.33 years. Twelve males and 25 females underwent unilateral TKA and seven females underwent bilateral TKA. Data collected was analysed grouping the patients depending on the increase, or decrease in the postoperative PFC i.e., patients were grouped as those with or without PFJ overstuffing respectively. In our study, 41 out of 51 postoperative TKAs showed evidence of PFJ overstuffing (Increased postoperative PFC). Thus, the chances of overstuffing of the PFJ were 80.39% [Table/Fig-8].
Chances of PFJ Overstuffing in primary TKA.
We found significant increase in post PFC in the group with PFJ overstuffing {postoperative PFC: Mean (M)±SD-3.58±0.16 cm} (preoperative PFC: M±SD–3.28±0.21 cm) (p-value<0.001), while the postoperative PFC decreased significantly in the group without postoperative PFJ overstuffing (postoperative PFC: M±SD - 3.55±0.1 cm) (preoperative PFC: M±SD – 3.69±0.16 cm) (p-value – 0.014)] compared to their preoperative-values.
The mean preoperative AFO of patients with or without postoperative PFJ overstuffing was significantly less than mean postoperative AFO [Table/Fig-9] Comparing the postoperative (M±SD – 2.41±0.16 cm) and preoperative (M±SD – 2.32±0.08 cm) PT in those with PFJ overstuffing, showed a significantly higher postoperative PT (p-value – 0.02) but comparing postoperative (M±SD – 2.36±0.19 cm) and preoperative (M±SD – 2.38±0.1 cm) PT in group of TKAs without PFJ overstuffing did not show any significant difference (p-value – 0.538) [Table/Fig-9]. Patients who had postoperative PFJ overstuffing had significantly less preoperative AFO (M±SD – 0.35±0.14 cm) compared to the patients who did not have postoperative PFJ overstuffing (M±SD – 0.65±0.09 cm) (p-value 0.00) . Comparing the postoperative AFO in patients with (M±SD – 0.91±0.02 cm) or without (M±SD – 0.93±0.03 cm) PFJ overstuffing, no significant difference was found (p-value – 0.077) [Table/Fig-10]. Female patients in our study had significantly less preoperative AFO compared to males (males – M±SD – 0.54±0.22 cm; females: M±SD – 0.36±0.14) (p-value 0.016) [Table/Fig-11].
Comparison of radiological parameters in postoperative TKA Vs preoperative TKA.
| Mean | Standard Deviation (SD) | Mean | SD | p-value |
|---|
| PFC (centimeters) |
| Postoperative with PFJ overstuffing | Preoperative with PFJ overstuffing | 0.000 |
| 3.58 | 0.16 | 3.28 | 0.21 |
| Postoperative without PFJ overstuffing | Preoperative without PFJ overstuffing | 0.014 |
| 3.55 | 0.1 | 3.69 | 0.15 |
| AFO (centimeters) |
| Postoperative with PFJ overstuffing | Preoperative with PFJ overstuffing | 0.000 |
| 0.91 | 0.02 | 0.35 | 0.14 |
| Postoperative without PFJ overstuffing | Preoperative without PFJ overstuffing | 0.000 |
| 0.932 | 0.03 | 0.646 | 0.09 |
| PT (centimeters) | |
| Postoperative with PFJ overstuffing | Preoperative with PFJ overstuffing | 0.002 |
| 2.41 | 0.16 | 2.32 | 0.08 |
| Postoperative without PFJ overstuffing | Preoperative without PFJ overstuffing | 0.538 |
| 2.36 | 0.19 | 2.38 | 0.1 |
Preoperative and postoperative AFO (centimeters) with post of PFJ overstuffing.
| Mean | SD | Mean | SD | p-value |
|---|
| Preoperative AFO (centimeters) |
| With postoperative PFJ overstuffing | Without postoperative PFJ overstuffing | 0.000 |
| 0.35 | 0.14 | 0.65 | 0.09 |
| Postoperative AFO (centimeters) |
| With postoperative PFJ overstuffing | Without postoperative PFJ overstuffing | 0.077 |
| 0.91 | 0.02 | 0.93 | 0.03 |
Preoperative AFO Gender differences.
| Gender difference in patients – Preoperative AFO (centimeters) | p-value |
|---|
| Males | Females | |
|---|
| Mean | SD | Mean | SD | |
|---|
| 0.54 | 0.22 | 0.36 | 0.14 | 0.016 |
In our study, the 24 weeks passive knee ROM in patients with postoperative PFJ overstuffing (M±SD–122.8°±6.34°) was significantly less compared to the group without postoperative PFJ overstuffing (M±SD – 128°±6.33°) [Table/Fig-12]. The mean PFJ overstuffing i. e. the mean increase in postoperative PFC in patients with PFJ overstuffing was 3 mm {(Mean postoperative PFC in patients with postoperative PFJ overstuffing - Mean postoperative PFC in patients without postoperative PFJ overstuffing) (3.58 cm – 3.28 cm = 0.30 cm i.e., 3 mm)} and the mean decrease in the passive knee ROM in the patients with PFJ overstuffing was 5.2 degrees {(Mean 24 weeks postoperative passive knee ROM in patients without postoperative PFJ overstuffing - Mean 24 weeks postoperative passive knee ROM in patients with postoperative PFJ overstuffing) (128° – 122.8° = 5.2°)} [Table/Fig-12].
Correlation of PFJ overstuffing with passive knee range of motion (degrees°).
| Weekspostoperative | Range of motionpostoperative withPFJ overstuffing | Range of motionpostoperative withoutPFJ overstuffing | p-value |
|---|
| Mean | SD | Mean | SD |
|---|
| 24 weeks | 122.8 | 6.34 | 128 | 6.33 | 0.024 |
Discussion
Recently there has been an increased interest in the management of PFJ arthritis to avoid complications related to PFJ in postoperative TKA patients. The PFJ in TKA has complex biomechanics and is a crucial factor in patient satisfaction, knee ROM, and outcome measurements [1,6]. Majority of the problems are related to the overstuffing of this joint leading to stiffness postoperatively.
The situation in which the postoperative antero-posterior size of the patella or anterior condyle of femur (or both) is increased compared to its preoperative-value is referred to as overstuffing of the PFJ [6,7]. Some studies have shown that overstuffing of this joint causes reduced knee ROM [1,6]. It also has been suggested that overstuffing might result in pain and inferior function of the joint [1,7–9].
Overstuffing in postoperative TKA patients can be the result of either a prominent anterior flange of the femur prosthesis or a patella that has been thickened by the prosthetic preparation beyond its preoperative dimensions. Berger RA first pointed out to this less commonly recognized problem i.e., the overstuffing of the PFJ by replacing more anterior femur than is resected in postoperative TKA patients [1]. This is a particular problem in women, where the anterior trochlea is often not as thick as the standard component that replaces it. We encountered PFJ overstuffing in 80.39% of the patients included in our study. In our study, patients who had significantly less preoperative AFO i.e., those with thinner anterior cortex of distal femur, had significantly more chances of postoperative PFJ overstuffing [Table/Fig-10]. Female patients included in our study had significantly thinner AFC of distal femur compared to males and thus had more chances of postoperative PFJ overstuffing [Table/Fig-11].
Lee A et al., in their study of PFJ overstuffing in TKA concluded that the PFJ overstuffing does affect the decrease of the angle of maximum flexion in TKA and the effect of anterior femur condyle overstuffing is superior to patellar overstuffing for the decrease in maximum flexion [9]. This finding is consistent with the results of our study, as majority of the TKA patients with postoperative PFJ overstuffing were secondary to replacement of the thinner anterior cortex of distal femur with a thicker anterior flange femur component.
Yamada K and Tawada K did a study to find effect of patellar thickness on intraoperative knee flexion and patellar tracking in navigated TKA [10]. They found that on average, passive knee flexion decreased 3 degree for every 2 mm increment of patellar thickness. Abolghasemian M et al., did a biomechanical study to evaluate the effects of patellar thickness on the passive knee ROM and found knee flexion to decrease exponentially with increased patellar thickness [4].
In our study also, we evaluated the effect of PFJ overstuffing on passive knee ROM in postoperative TKA patients. Patients having higher preoperative knee ROM tend to achieve better knee ROM postoperative [11]. In our study group, there was no significant difference in the preoperative knee ROM in both the groups {with PFJ overstuffing (M±SD – 98.9±7.2°); without PFJ overstuffing (M±SD – 98.5±8.83°) (p-value – 0.88)}. Thus, preoperative knee ROM did not have any significant influence on the knee ROM achieved postoperatively. The passive knee ROM in the postoperative TKA patients approximately decreased by 2 degrees for every 1 mm of increase in PFC compared to its preoperative value in the patients with PFJ overstuffing. This result was also consistent with the study of Bengs BC et al., [12]. In their study - The effect of PT on intraoperative knee flexion and patellar tracking in TKA, they showed that on an average, passive knee flexion decreased 3° for every 2 mm increment of patellar thickness. These findings are also supported by Lee A et al., [9] who concluded that the PF overstuffing does affect the decrease of maximum flexion angle in TKA.
Limitation
Sample size calculation was not done. All the patients operated for primary TKA suiting the inclusion and exclusion criteria during the study duration were studied. Also the study is purely radiological and does not rely on in vivo intraoperative measurements. We urge readers to carry out further studies using intraoperative measurements to validate the results and make use of PFC during TKA to avoid PF overstuffing in postoperative TKA patients.
Conclusion
Overstuffing of the PFJ in postoperative TKA is present in 80.39% patients. Higher chances of postoperative PFJ overstuffing are present in female patients and those with thinner anterior cortex of distal femur. Postoperative passive knee ROM decreases significantly in patients with postoperative PFJ overstuffing (Every 1 mm increase in the postoperative PFC, passive knee ROM decreased by approximately 2 degrees).