Case Report
A 39-year-old male reported with the complaint of an ulcer on left lateral aspect of tongue since a month which was associated with dull, continuous and non radiating pain. Patient was a known gutka (smokeless tobacco) chewer since 15 years, with a frequency of four to five times/day.
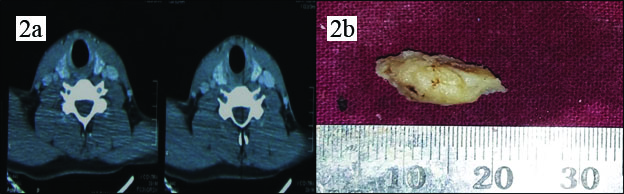
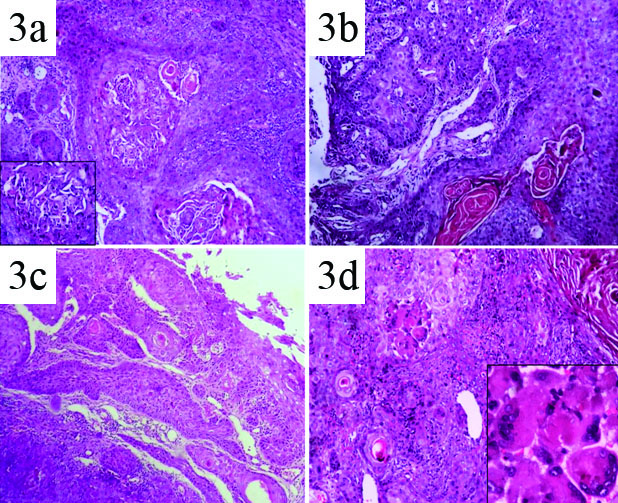
On intraoral examination, an irregular ulcer of approximately 2.5 cm × 1.5 cm in size was noticed on the left lateral border of the tongue [Table/Fig-1]. The left maxillary and mandibular permanent first molars were decayed and had sharp jagged edges. Classic features such as everted margins and induration on palpation lead to a provisional diagnosis of malignancy of tongue. There were no palpable regional and cervical lymph nodes. Further a CT scan: plain and contrast were performed which did not show any nodal involvement [Table/Fig-2a]. Routine haematological investigations showed that all values were in normal range. Representative area was biopsied and sent for histopathological examination [Table/Fig-2b].
Ulcer on the left lateral border of tongue.

a) Computed tomography (contrast) image with absence of nodal metastasis; b) Gross photograph of incisional biopsy specimen which was whitish brown in colour and firm in consistency.
Histopathological and Immunohistochemical Report
Haematoxylin and Eosin (H&E) stained serial sections showed both basaloid and squamous components in the form of solid islands, nests and strands [Table/Fig-3a]. The tumour islands were lined peripherally by palisading basaloid cells with hyperchromatic nuclei [Table/Fig-3b], minimum or absence of nucleoli and scant cytoplasm. The islands with squamous differentiation displayed keratin pearls and central area of comedonecrosis [Table/Fig-3a-c]. These basaloid tumour islands were accompanied by component of well differentiated squamous cell carcinoma meeting Broder’s grading system and foci of tumour giant cells [Table/Fig-3d]. Mitotic figures and abnormal mitosis were also evident [Table/Fig-4a,b].
Photomicrographs of H&E stained sections showing features of basaloid squamous cell carcinoma: a) 4x: Basaloid tumour cells in the form of islands and nests. Areas of comedonecrosis and squamous differentiation. Comedonecrosis inset (40x); b,c) 10x: Islands of squamous cells and keratin pearl formation; d) 10x: Foci of tumour giant cells, inset (40x).
Photomicrographs of features of basaloid squamous cell carcinoma: a,b) 10x: numerous mitotic figures, inset (40x) (H&E stain); c) 10x: small cystic spaces containing PAS positive material resembling mucin (PAS stain); d) 10x: stromal hyalinosis showing PAS positivity. (PAS stain)
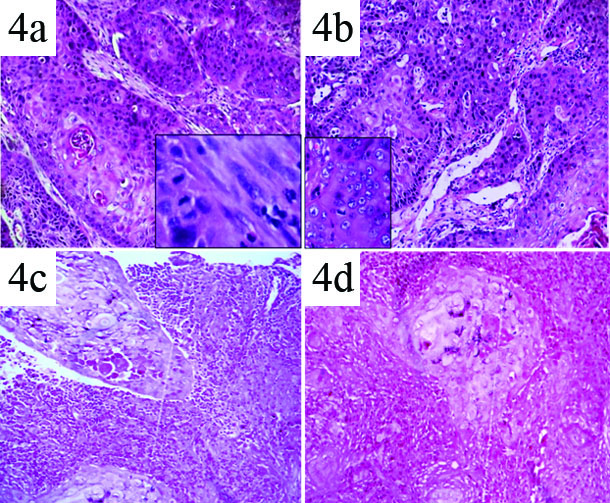
Periodic Acid Sciff (PAS) staining was employed to demonstrate hyalinosis and eosinophilic material. The stromal hyaline material and the basement membrane surrounding the tumour nests were positive for PAS staining, favouring the diagnosis of BSCC [Table/Fig-4c,d].
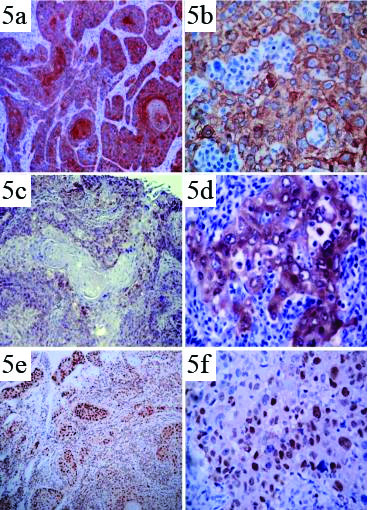
Further, immunohistochemistry with antibodies for pancytokeratin (AE1/AE3) [Table/Fig-5a,b], p16 [Table/Fig-5c,d] and PCNA [Table/Fig-5e,f] was performed which revealed cytoplasmic, membranous positivity for AE1/AE3 with strong nuclear positivity for PCNA and diffuse cytoplasmic positivity for p16. Thus, the final diagnosis of basaloid squamous cell carcinoma with high proliferative index was confirmed.
Photomicrographs of immunohistochemical staining: a,b) Basaloid tumour cells showing diffuse positive immunoreactivity in cytoplasm and cell membrane for PAN cytokeratin (AE1/AE3); c,d) Basaloid tumour cells showing diffuse positive immunoreactivity in cytoplasm for p16; e,f) Basaloid tumour cells showing diffuse nuclear positive immunoreactivity for PCNA.
Discussion
BSCC is a rare entity that is distinct from conventional Squamous Cell Carcinoma (SCC) and other variants of Oral Squamous Cell Carcinoma (OSCC) like verrucous, papillary, adenosquamous, adenoid, spindle cell and undifferentiated carcinoma [1].
In 2005, World Health Organisation (WHO) has considered BSCC as a separate clinico-pathological entity and described it as “an aggressive, high-grade variant of SCC composed of both basaloid and squamous components, with histopathologic appearance being divergent from well or moderately differentiated SCC”. The neoplasm displays varying proportion of typical squamous component interspersed with nests of basaloid cells arranged in lobules with prominent peripheral palisading and central foci of comedonecrosis. Until 2005 the true incidence rate of BSCC in head and neck was uncertain due to the lack of definitive criteria to diagnose these cases [1,2]. BSCC is one of the rare variant among seven histological subtypes of SCC that accounts for 15% of all SCCs encountered in the head and neck [3].
BSCC was first described as a separate entity in the head and neck region by Wain SL et al., with highest predilection rate in the tongue, larynx and hypopharynx [4]. As with conventional OSCC, tobacco and alcohol abuse are strong risk factors. HPV types 16 and 18 are thought to cause SCC and have been detected in some BSCCs, especially those of the glans penis and anus, but the exact role of HPV and its subtypes in BSCC is uncertain and debatable [1,2,4].
Clinically, the symptoms of BSCC resemble that of conventional SCC and these vary according to the site of origin. BSCC has male sex predilection occurring in the age group between 27-88 years with an average of 63 years, as in the present case. Macroscopically, BSCC are firm to hard exophytic masses with central ulceration and marginal submucosal induration [5–7].
As the name implies, microscopically BSCC is composed, of two main components basaloid and squamous component. The basaloid cells being one of the primary components of lesion are arranged in lobules, sheets, cords or islands and peripheral palisaded arrangement with central part of the islands composed of squamous cells. Few islands show characteristic central ischemic necrosis (comedonecrosis) and frequent abnormal mitosis suggestive of aggressive behaviour. Basaloid cells have scanty cytoplasm, round to oval shaped prominent hyperchromatic or vesicular nuclei with or without nucleoli [1,4,7–9].
The other component of BSCC is squamous differentiation, which can be identified by the presence of polyhedral epithelial cells with prominent intercellular bridges, arranged in mosaic pattern with keratin pearl formation and dyskeratosis in the form of individual cell keratinization [4]. Other ancillary features of BSCC include microcysts with central area of eosinophilic material which will often be weakly positive for PAS and alcian blue stains, as well as deposition of amorphous material in between tumour cells and lobules termed as hyalinosis [1,4]. The present case showed positivity with PAS for hyaline material.
The stroma of lesional area may display myxoid areas with basophilic extracellular component as background. Other than aforementioned features, metastasis to regional lymphnode is one of the common features of BSCC. Few cases have been reported with perineural and perivascular invasion [7,10]. To make the definitive diagnosis of BSCC, at least 10% of definable squamous cell carcinoma element along with predominant basaloid component must be present [4]. Immunohistochemical markers like p53, p63, PCNA, Ki67, p16, AE1/AE3, CK1, CK14 and CK7 are valuable to reflect the biological behaviour of the BSCC and helps to distinguish from conventional SCC and other malignancies [9,11].
The diagnosis of BSCC on incisional biopsy becomes a challenging task for pathologist as the histopathological features of BSCC overlap with many other neoplasms sharing similar microscopic appearance. In the oral cavity, the differential diagnosis of BSCC includes Adenoid Cystic Carcinoma (AdCC), Adenosquamous Carcinoma (ASC), Polymorphous Low Grade Adenocarcinoma (PLGA), Basal Cell Carcinoma (BCC) and Salivary Duct Carcinoma (SDC) [5]. Few features that help us to differentiate these lesions from BSCC are high mitotic activity, well/moderate squamous cell carcinoma component, prominent comedonecrosis along with high and diffuse immunoreactivity for p53, Ki67, PCNA, p63 markers [1,9].
The five year survival rate of lip cancer is 90%, tongue is 40% and other sites in oral cavity are around 50% [12]. Tongue has comparatively poor prognosis because of extensive lymphatic drainage system and vascular supply [13].
However, the case presented here is unique with respect to younger age group, location on lateral aspect of tongue and non-aggressive biological behaviour with absence of lymph node involvement. Although being clinically deceptive as T2 N0 lesion, the histopathological features are in contrast with high mitotic figures, areas of comedonecrosis, tumour giant cells and high PCNA index. Use of special stains and immunohistochemistry has ruled out other malignancies like AdCC, PLGA and SDC.
Further, p16 immunostaining was carried out to ascertain the HPV status in BSCC as p16 is a cell cycle protein that prevents the inactivation of retinoblastoma protein and progression of S phase of the cell cycle. It is well documented that HPV oncoprotein E7–mediated inactivation of retinoblastoma protein leads to a loss of inhibition of p16 transcription and overexpression of the same. A p16 overexpression is considered as a diagnostic marker of HPV-induced tumours of the cervix and upper aerodigestive tract and is very uncommon in HPV-negative SCC. Earlier studies postulate that the HPV-positive BSCCs were limited to the oropharynx whereas, tumours of the larynx/hypopharynx were HPV negative. This signifies that tumour site decides the survival rate of the patient rather than their HPV status. So, p16 can be used as an indirect marker for the detection of HPV [11]. In the present case, we noticed diffuse immunoreactivity for p16 in areas with basaloid component compared to the other areas. By considering the above clinical, histopathological and immunohistochemical features a diagnosis of BSCC was made. Entire lesion was excised following surgical guidelines and patient is being followed up periodically.
Although, the present case had no distant metastasis, there have been cases associated with high rate of local and distant metastases [14]. Hence, thorough diagnostic work-up with surgical treatment and adjunct chemotherapy is recommended for patients with BSCC [1,2,5].
There is an ongoing debate over the prognosis of BSCC compared to conventional SCC. Although some studies have proved similar outcomes in both BSCC and SCC, others believe that BSCC has a worse survival outcome [3]. Fritsch VA et al., in his study concluded that poor prognosis of BSCC is unrelated to its location, disease stage and therapeutic strategy which is contrast to the present case [3]. However, patients presented with advanced BSCC clinically had poor prognosis [15].
Conclusion
BSCC is a histopathologically distinct form of conventional squamous cell carcinoma with aggressive biological behaviour affecting commonly upper aerodigestive tract and males with long standing history of tobacco use. Due to its biphasic nature, BSCC may not be identified if the sparse squamous component is overlooked or not appreciated, especially in incisional biopsies. Hence, BSCC needs to be differentiated from other histologically similar lesions like AdCC and small cell neuroendocrine carcinoma because of different management regimens and prognosis.
[1]. Barnes L, Basaloid squamous cell carcinoma. In: Barnes L, editorSurgical pathology of the head and neck 2001 2New YorkMarcel Dekker:184-89. [Google Scholar]
[2]. Barnes L, Eveson JW, Reichart P, Sidransky D, Pathology and genetics, head and neck tumoursWorld Health Organization classification of tumours 2005 Lyon, FranceIARC Press [Google Scholar]
[3]. Fritsch VA, Gerry DR, Lentsch EJ, Basaloid squamous cell carcinoma of the oral cavity: an analysis of 92 casesLaryngoscope 2014 124:1573-78. [Google Scholar]
[4]. Wain SL, Kier R, Vollmer RT, Bossen EH, Basaloid-squamous carcinoma of the tongue, hypopharynx, and larynx: report of 10 casesHum Pathol 1986 17(11):1158-66. [Google Scholar]
[5]. Yamagata K, Karube R, Yanagawa T, Zemann W, Metzler P, Onizawa K, Basaloid squamous cell carcinoma of the oral cavity: A case seriesIJCAI 2013 4(4):199-207. [Google Scholar]
[6]. Kuan EC, Peng KA, Bhuta S, Diaz MF, Zhang ZF, Abemayor E, Basaloid squamous cell carcinoma of the maxilla: Report of a case and literature reviewAmerican Journal of Otolaryngology 2015 36(3):402-07. [Google Scholar]
[7]. Ereño C, Gaafar A, Garmendia M, Etxezarraga C, Bilbao FJ, López JI, Basaloid squamous cell carcinoma of the head and neck: a clinicopathological and follow-up study of 40 cases and review of the literatureHead and Neck Pathology 2008 2(2):83-91. [Google Scholar]
[8]. Sundharam BS, Krishnan PA, Basaloid squamous cell carcinoma report of a case and review of literatureIndian J Dent Res 2003 14:184-86. [Google Scholar]
[9]. de Sampaio Goes FC, Oliveira DT, Dorta RG, Nishimoto IN, Landman G, Kowalski LP, Prognoses of oral basaloid squamous cell carcinoma and squamous cell carcinoma: a comparisonArch Otolaryngol Head Neck Surg 2004 130(1):83-86. [Google Scholar]
[10]. Choussy O, Bertrand M, François A, Blot E, Hamidou H, Dehesdin D, Basaloid squamous cell carcinoma of the head and neck: report of 18 casesThe Journal of Laryngology & Otology 2011 125(06):608-13. [Google Scholar]
[11]. Lantuejoul S, Faure C, Righini C, Soriano E, Claraz C, Reyt E, Basaloid squamous cell carcinoma of the head and neck: histological and immunohistochimical analysis of 47 casesMod pathol 2004 15(Suppl 1):227A [Google Scholar]
[12]. Cancer Research UK. Survival statistics for mouth or oropharyngeal cancer [Internet]. [Updated 2014 Oct 14; cited 19th June 2016]. Available from:http://www.cancerresearchuk.org/about-cancer/type/mouthcancer/treatment/statistics-and-outlook-for-mouth-cancers [Google Scholar]
[13]. Azimi H, Khajehahmadi S, Rahpeyma A, Tongue squamous cell carcinoma: a clinical studyIranian Journal of Pathology 2014 9(1):28-32. [Google Scholar]
[14]. Soriano E, Faure C, Lantuejoul S, Reyt E, Bolla M, Brambilla E, Course and prognosis of basaloid squamous cell carcinoma of the head and neck: a case control study of 62 patientsEur J Cancer 2008 44:244-50. [Google Scholar]
[15]. Winzenburg SM, Niehans GA, George E, Daly K, Adams GL, Basaloid squamous carcinoma: a clinical comparison of two histologic types with poorly differentiated squamous cell carcinomaOtolaryngol Head Neck Surg 1998 119:471-75. [Google Scholar]